Introduction
The medial pterygoid muscle, a major elevator of the jaw is a square-shaped masticatory muscle, located on the medial aspect of the lower jaw bilaterally. It is also known as internal pterygoid muscle. This muscle lies medial to the lateral pterygoid muscle.
Structure and Function
The medial pterygoid muscle has a triple function. First, bilateral contraction of the muscle with lateral pterygoid muscle results in protrusion of the mandible.[1] This action results as the muscle fibers are aligned anteroposteriorly.[1] Second, unilateral contraction of the medial pterygoid muscle with lateral pterygoid muscle ipsilaterally results in lateral movement of the mandible towards the opposite side. This action occurs due to the mediolateral direction of the muscle fibers. Third, the muscle functions with masseter and temporalis muscles to elevate the mandible.[1]
The medial pterygoid muscle is characterized by short muscle fibers and large physiological cross-sectional area in comparison to other pterygoid muscle (lateral pterygoid). As a result of this configuration, the medial pterygoid muscle can exert about 1.6 times higher force than that produced by the lateral pterygoid muscle.[2]
Embryology
The entire masticatory musculature originates from the muscular component of the first branchial arch. Hence, the medial pterygoid muscle also develops from the mandibular arch.
Blood Supply and Lymphatics
The medial pterygoid muscle receives vascular supply from the maxillary artery through its pterygoid branches and by the facial artery through its muscular branches. The pterygoid branches of the maxillary artery are 2 or 3 in number. They run in an anterior and inferior direction to enter the medial aspect of the medial pterygoid muscle.
The literature describes as many as three different types of muscular branches of facial artery that supply the medial pterygoid muscle.[3] The first muscular branch arises directly from the facial artery near the mandibular angle. The second muscular branch arises from the ascending palatine artery, which arises from the facial artery in the cervical area. The third branch is an anterior muscular branch that arises from either the tonsillar or submental branch of the facial artery. This branch enters the muscle from the anteromedial direction.
Sometimes, the medial pterygoid muscle may receive its vascular supply from a direct branch from the external carotid artery that enters the lower part of the muscle posteriorly about 2 cm above the gonion.
Nerves
The medial pterygoid muscle is innervated by the medial pterygoid nerve, which is a branch of the main trunk of the mandibular branch of cranial nerve V (trigeminal nerve). The nerve to the medial pterygoid enters from the upper region of the posterior border or the medial area of the superoposterior border of the muscle.[4]
The accessory medial pterygoid muscle gets independent innervation from the branch of the mandibular nerve that branches 1 cm below the foramen ovale.[5]
Muscles
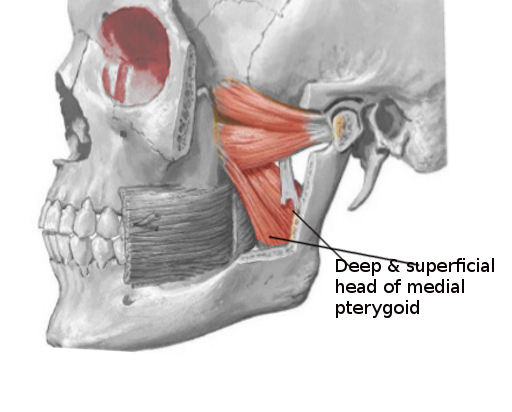
The medial pterygoid muscle has a superficial and a deep head which arise from different areas of the jaw. The lateral pterygoid muscle via its lower head separates the two distinct heads. The smaller superficial head has its origin mainly from the maxillary tuberosity with some fibers arising from the pyramidal process of the palatine bone. The larger deep head has its origin from the medial side of a horseshoe-shaped extension of the sphenoid bone (lateral pterygoid plate) at the base of the skull.
Its fibers pass in a downward, lateral, and posterior direction and have their insertion via a strong tendinous lamina, into the roughened area on the lower and posterior part of the medial or inner surface of the ramus and angle of the mandible, as high as the mandibular foramen.
The muscle is divided by the tendinous sheets into three layers recognizable in its upper one third.[4]
The lingual nerve runs in an anteroinferior direction lateral to the belly of the medial pterygoid muscle and medial to the mandible. The area between the medial pterygoid muscle and superior constrictor muscle is referred to as the prestyloid space, which is filled with fat.
Physiologic Variants
Sometimes, an accessory medial pterygoid muscle is also present as a separate muscle near the deep head of the medial pterygoid muscle. Its origin is from the posterior end of the superior border of the lateral pterygoid plate near foramen ovale and merges with the fibers of the medial pterygoid muscle. The merging occurs either on the middle region of the medial surface of the deep head of medial pterygoid muscle or the superior border of the deep head of medial pterygoid muscle near its tendinous portion approximately 1-2cm beyond the point of exit of the muscle from pterygoid fossae.[5]
This accessory muscle is flat and triangular, 2 cm long with its narrowest part towards the insertion. The function is unknown; however, there have been suggestions that it assists the medial pterygoid muscle in lateral jaw positioning during protrusion and closure.
Surgical Considerations
In patients with a prognathic mandible (Class III malocclusion) requiring orthognathic surgery to provide mandibular setback, a standard procedure is to prevent interference by muscle and ligament by stripping the medial pterygoid muscle and stylomandibular ligament off the medial side of the proximal segment.[6]
During nerve block procedure for the mandibular arch, the area where the needle should focus is occupied to a large extent by the medial pterygoid muscle. During an inferior alveolar nerve block, if the needle placement is too medial, there are chances that the needle might pierce the medial pterygoid muscle resulting in less effective anesthesia as well as postoperative trismus.[7]
Clinical Significance
The medial pterygoid muscle along with masseter muscle forms a 'pterygomassetric sling' that suspends the mandible. After orthognathic surgery to treat mandibular prognathism, this sling greatly affects the stability of the two segments of the mandible. Also, the healing process of bone between the two segments (distal and proximal) is subject to influence by the magnitude of force applied by the sling.[8]
Infection in the mandibular teeth more frequently involves the lower compartment of the masticatory space, which contains medial pterygoid muscle; this could result in pterygoid muscle abscess. Since both masticator space and infratemporal fossa share the medial pterygoid muscle, there are chances of the potential spread of infection from this space to the infratemporal fossa.
Sometimes, an occlusal interference may occur due to movement of the accessory medial pterygoid muscle, which is clinically evident on the buccal cusps of the third molar. This occlusion abnormality may act as a trigger point for spasm of the muscle, which can be clinically checked by fixing the mandible under pressure in the most posterior and centric position to make the interfering occlusal contacts evident.[5]
During vertical jaw movements, lateral pterygoid muscle act as a primary muscle that generates horizontal forces. However, the medial pterygoid muscle may also play a role in controlling horizontal jaw positions.[9]
Other Issues
Utmost care is necessary during the surgical removal of the third molar in the mandibular arch as the tooth can easily get displaced into the space present between the ramus of the mandible and medial pterygoid muscle.[10]