Introduction
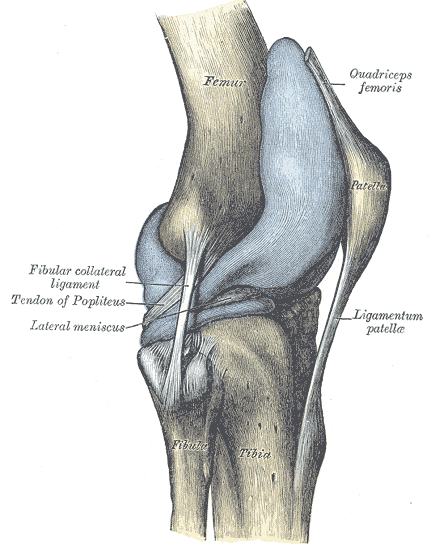
The knee is the largest joint in the body (see Image. Lateral View of the Right Knee). The knee is primarily a hinge joint, allowing leg flexion and extension. Other movements are also possible, though to a limited extent. Tibiofemoral and patellofemoral articulations make the knee a compound synovial joint.[1][2]
The knee is critical to efficient bipedal movements like walking, running, and jumping. Muscular support is this joint's most important stabilizing factor, and proper conditioning and training can help prevent sports injuries. Understanding its structure helps optimize lower limb rehabilitative strategies.
Structure and Function
Knee Structure
The bones articulating at the knee are large and complex. The femur has a slight medial slant, while the tibia is nearly vertical. The patella is a sesamoid bone—the largest in the body—occupying the anterior part of the knee. It is the distal attachment point of the quadriceps tendon. The patella also protects the anterior articular surface of the distal femur. The fibula is not part of the knee joint.
The surfaces articulating at the knee are the following:
- Lateral and medial condylar surfaces of the femur and tibia
- Anteroposterior articulation between the patella and femur
The knee joints are weak on their own but are stabilized by the following structures.[3][4][22]
- Quadriceps femoris: a 4-component muscle complex that attaches to the patella via the quadriceps tendon
- Fibrous capsule: attaches to the femur proximally, the tibia distally, and the intercondylar fossa posteriorly; deficient on the lateral condylar area, where the tendon of the popliteus exits the joint to insert on the tibia; has a synovial membrane lining
- Extracapsular ligaments, which include the following:
- Patellar ligament: extends inferiorly from the patella and attaches distally to the anterosuperior aspect of the tibia; reinforces the capsule anteriorly
- Fibular collateral ligament or lateral collateral ligament (LCL): runs inferiorly from the lateral femoral epicondyle to the fibular head's lateral surface; prevents varus stress on the knee (bowed knees)
- Tibial collateral ligament or medial collateral ligament (MCL): extends from the medial femoral epicondyle to the medial condyle and superomedial tibial surface; typically firmly attached to the medial meniscus; prevents valgus stress on the knee (knocked knees)
- Oblique popliteal ligament: a continuation of the semimembranosus tendon; reinforces the fibrous capsule posteriorly
- Arcuate popliteal ligament: originates from the fibular head's posterior margin, extends superomedially over the tendon of the popliteus, and occupies the posterior aspect of the knee joint
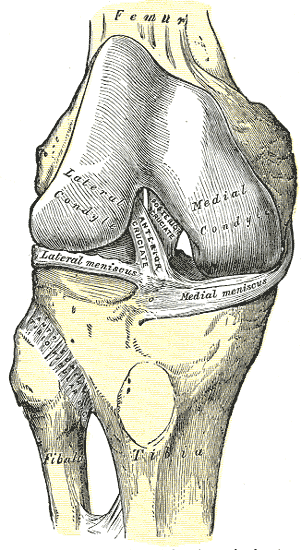
- Intraarticular ligaments, which include the following (see Image. Intraarticular Ligaments Of The Right Knee, Anterior View):
- Anterior cruciate ligament (ACL): emerges from the anterior tibial intercondylar area posterior to the medial meniscal attachment and inserts on the posteromedial surface of the lateral femoral condyle; prevents knee hyperextension, posterior femoral displacement, and anterior tibial displacement in the flexed knee; is the weaker cruciate ligament with poor circulation
- Posterior cruciate ligament (PCL): originates from the posterior tibial intercondylar region and inserts on the anterolateral aspect of the medial femoral condyle; tightens during knee flexion and prevents hyperflexion and posterior tibial displacement; stronger cruciate ligament; supports the body weight when the knee is flexed
- Medial and lateral menisci: fibrocartilaginous structures lying between the tibiofemoral articular surfaces; function as shock absorbers, static stabilizers, and friction reducers during articulation
Bursae are small sacs surrounding the joints. They are lined with synovial membranes and contain synovial fluid. The bursae around the knee reduce friction between its different components during movement. These structures also help stabilize the knee. There are at least 12 knee bursae, but the notable ones are the following:
- Suprapatellar bursa: extension of the knee joint cavity; located deep to the quadriceps femoris tendon
- Popliteus bursa: between the popliteal tendon and lateral tibial condyle
- Anserine bursa: located between the sartorius, gracilis, and semitendinosus tendons
- Gastrocnemius bursa: deep to the superior attachment of the gastrocnemius' medial head
- Prepatellar bursa: a subcutaneous bursa protecting the anterior patellar surface
- Deep and subcutaneous infrapatellar bursae: lie inferior to the patella posterior to the patellar ligament
- Medial collateral ligament bursa: lies within the superficial and deep parts of the MCL
- Iliotibial bursa: situated in the distal iliotibial band close to its insertion on the Gerdy tubercle
Four of the knee's bursae communicate with its synovial cavity, namely, the suprapatellar, popliteus, anserine, and gastrocnemius bursae.
Knee Functions
The knee is a weight-bearing joint primarily for sagittal plane motion, ie, flexion and extension. Secondary movements include the following, though their range is limited by the joint's soft tissue support:[5][6]
- Internal and external rotation
- Compression and distraction
- Anterior and posterior translation
- Medial and lateral translation
- Varus and valgus movements
The muscles around the knee are the joint's "dynamic stabilizers," preserving the moving knee's integrity. The other soft tissues are "static stabilizers," keeping the resting joint intact.
Embryology
Knee structures arise from the mesoderm during the 2nd week of development. The muscles and neurovascular components supporting the joint also emerge from the mesodermal layer around the 4th week of development. In the 6th week, chondrocytes start to form cartilaginous femur and tibia. Mesenchymal tissue gives rise to the knee's connective tissues, eg, the menisci and ligaments, in the 10th week. All long bones would have developed primary ossification centers by the 12th week.
Blood Supply and Lymphatics
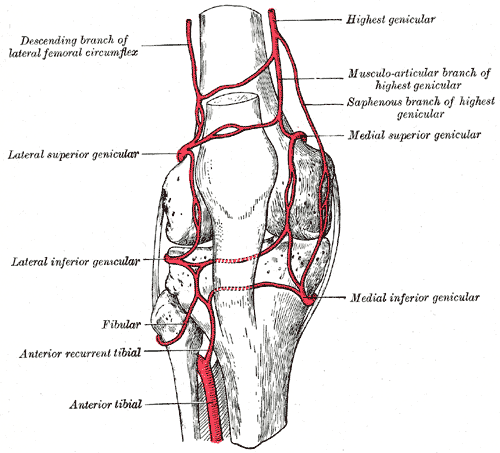
The "genicular anastomosis," the vast arterial network in the knee region, has contributions from the following blood vessels (see Image, Genicular Anastomosis):
- Femoral artery: its superficial branch gives off the descending genicular artery
- Popliteal artery: bifurcates from the superficial femoral artery and gives off the superior medial, inferior medial, superior lateral, and inferior lateral genicular branches; the medial genicular artery supplies the fibrous capsule, cruciate ligaments, synovial membranes, and menisci
- Anterior and posterior recurrent branches of the circumflex fibular and anterior tibial recurrent arteries
Venous drainage around the knee is via the superficial and deep lower limb veins. Superficial veins in the region include the following:
- Great saphenous vein: ascends in the knee region's posteromedial aspect and anastomoses with the small saphenous vein
- Small saphenous vein: emerges between the gastrocnemius' heads and drains into the popliteal vein in the popliteal fossa
Perforating veins pierce the deep fascia and connect the superficial and deep lower limb veins.
The posterior tibial veins are the deep lower extremity veins passing posterior to the knee area. These blood vessels empty into the deep veins of the thigh (vena profunda femoris).
Most lymph from the knee and leg drains into the popliteal lymph nodes in the popliteal fossa. The popliteal nodes and other knee and lower limb lymphatics empty into the deep inguinal and subinguinal nodes.
Nerves
The structures of the knee and most knee extensors are innervated by the femoral nerve (L1 to L3). The gracilis muscle, which crosses the knee superoinferiorly and flexes the leg, is innervated by the obturator nerve (L2 and L3). The knee flexors in the posterior thigh compartment are supplied by the sciatic nerve (L4 to S3), which branches into the tibial and common peroneal nerves. The tibial nerve innervates the gastrocnemius, a knee flexor in the posterior leg compartment.
Muscles
Muscles around the knee are not only responsible for the joint's movements; they also assist the knee ligaments in preventing its excessive displacement in any direction. These muscles include knee extensors and knee flexors.
Knee extensors (mainly the quadriceps femoris) form the quadriceps tendon conjointly and are innervated by the femoral nerve. The quadriceps tendon attaches the quadriceps to the patella. Knee extensors are the main muscular stabilizers of the knee joint and include the following:
- Rectus femoris
- Vastus lateralis
- Vastus medialis
- Vastus intermedius
Knee flexors include the semimembranosus, biceps femoris, gracilis, gastrocnemius, and popliteus. The gracilus is a thigh adductor that flexes and medially rotates the knee. The popliteus unlocks and weekly flexes the knee. Divisions of the sciatic nerve or tibial nerve innervate knee flexors. The knee flexors and their innervations are listed below.
- Semitendinosus: innervated by the tibial division of the sciatic nerve
- Semimembranosus: innervated by the tibial division of the sciatic nerve
- Biceps femoris: innervated by the tibial (long head) and common peroneal (short head) divisions of the sciatic nerve
- Gracilis: innervated by the obturator nerve
- Gastrocnemius: innervated by the tibial nerve
- Popliteus: innervated by the tibial nerve
Physiologic Variants
Genu varum (bowed legs) and genu valgum (knocked knees) may be considered normal conditions in very young children. Persistence into late childhood may be due to an underlying pathology, which must be investigated and promptly corrected. Conservative treatment is achieved through knee bracing, which is recommended for mild-to-moderate cases. Severe knee deformities require surgery.[7]
Surgical Considerations
Ligamentous and meniscal tears are common knee injuries typically requiring surgical intervention. Ligament repairs are often done arthroscopically, using grafts such as hamstring, patellar, and allografts to repair the defect. Extensive post-surgical rehabilitation by knee bracing and exercises is typically recommended. Meniscal tears may be repaired by arthroscopic meniscectomy, an outpatient procedure that allows faster recovery.
Knee osteoarthritis arises from cartilaginous depletion in the knee's articulating surfaces. Contributory factors to its development include genetics, weight, activity, and previous injury. Mild-to-moderate cases can be treated conservatively by measures such as weight reduction and orthotics. Severe knee osteoarthritis presents with great pain and limited range of motion, which may reduce quality of life. Total knee arthroplasty with metal, ceramic, or plastic prosthetics is recommended in such cases. This type of surgery is more often performed in older individuals and requires extensive rehabilitation.[8][9][10]
Clinical Significance
ACL Injury
The ACL is the most commonly injured intrinsic knee ligament during non-contact sports activities. The mechanism involves changing one's direction of motion with the planted leg rotated. Patients report feeling a pop in the knee followed immediately by pain and joint effusion. The Lachman and anterior drawer tests are techniques frequently used to assess for ACL damage.
MRI is the best imaging modality when evaluating soft tissue pathology, as in ACL injuries. Surgery is recommended for young patients with a torn ACL to maintain knee stability, especially when participating in sports. Meanwhile, older individuals with the same condition may be treated with conservative treatment by activity modification and physical therapy.
Meniscal Tear
Meniscal tears often accompany ACL rupture. Thus, they have the same injury mechanism. The lateral meniscus is more often involved in acute injuries, while chronic degenerative cases more commonly affect the medial meniscus. Typical symptoms include pain, joint effusion, and knee clicking, locking, and catching during activity. However, the condition may sometimes be asymptomatic.[23]
The McMurray test helps detect meniscal tears during physical examination. MRI is the preferred diagnostic test to confirm the diagnosis. Treatment is variable, ranging from conservative to surgical.
MCL Injury
MCL injuries have a pathophysiological mechanism different from ACL tears. A direct force lateral to the knee and causing excessive valgus stress is typically required. Pain and joint effusion develop soon after the injury. On physical examination, valgus stress causes pain in the affected knee. MRI is the best imaging modality for MCL assessment.
Treatment for mild cases is frequently conservative, with knee bracing and non-weight-bearing activities. However, surgery may be indicated in some cases, eg, the "unhappy triad of knee injuries" from sports activities. This condition arises when the MCL ruptures and also tears the medial meniscus and ACL due to their firm attachment.[24]
PCL Injury
The PCL is the largest and strongest knee ligament. PCL rupture usually requires great force, enough to damage other knee structures. Thus, isolated PCL tears are uncommon. The injuring force must come posteriorly and hit the flexed knee—a mechanism usually associated with high-energy trauma. A positive posterior drawer test on physical examination helps detect PCL injury. Treatment may be conservative or nonconservative, depending on the severity.
Patellofemoral Pain Syndrome
Patellofemoral pain syndrome is another common sports-related condition. The most notable symptom is anterior knee pain aggravated by flexion of the weight-bearing knee during activities such as running, coming down a hill, climbing stairs, or jumping. The pathophysiology of this condition is unclear, though overuse, muscular imbalance, and improper patellar tracking have been implicated.
The diagnosis is made clinically, with imaging typically done only to rule out other conditions. Management includes resting, stretching, physical therapy, and a gradual return to activity.
Knee Dislocation
Knee dislocations can affect all 3 articulations, though tibiofemoral injuries are typically more severe and require emergency treatment. A tibiofemoral dislocation is usually caused by a great injuring force that may damage other knee structures. Knee x-ray and MRI aid in assessing the extent of the injury.
Popliteal artery damage is the most urgent complication of a tibiofemoral dislocation and must be repaired quickly to prevent irreversible deficits. Arterial injury may be assessed initially by palpating the lower limb arteries, taking the ankle-brachial index, and ultrasound imaging. Spontaneous reduction may occur in mild cases, but closed or open reduction may be performed to repair extensive injuries.
Osteoarthritis
Osteoarthritis is predicted to become a worsening problem in developed countries due to obesity and increased longevity.[11][12] In the US, osteoarthritis-related costs are estimated to reach $185 million annually.[13] The condition most frequently affects the hips, knees, hands, and vertebral column. The ankles and feet are less commonly involved.
Osteoarthritis arises from erosion and subsequent loss of knee articular cartilage. Meniscal degeneration and subchondral knee bone and cartilage alterations are also common. Symptoms are chronic and progressive and include knee pain, stiffness, loss of range of motion, and loss of functional ability.[14] Osteoarthritis highly correlates with engagement in sports activities, as revealed by studies involving American football, baseball, ice hockey, wrestling, and handball players. Aging is a factor in the development of the condition, though it is also prevalent in middle-aged patients.[15][16][17][18][19]
Individuals with mild symptoms may be treated conservatively with bodyweight reduction, nonsteroidal anti-inflammatory drugs, physical therapy, and intraarticular steroid injections. Total knee arthroplasty may be performed if the condition severely compromises quality of life. Novel therapies in the pipeline include biologics and nanotechnology-based gene delivery systems. Platelet-rich plasma treatment is another option, though evidence proving its effectiveness is inadequate.[12][20][21]
Septic Bursitis
Infection of the knee bursae can occur secondary to direct inoculation, direct spread, or hematogenous spread. Direct inoculation makes subcutaneous bursae, eg, the prepatellar and infrapatellar bursae, vulnerable to this condition. Suprapatellar infection can arise from any of the 3 mechanisms. The suprapatellar bursa's communication with the knee cavity can spread the infection to the knee joint.
Septic bursitis is time-sensitive, as delayed treatment can impair mobility. The most common etiologic agent is Staphylococcus aureus. Broad-spectrum intravenous antibiotics may be given empirically to septic patients and tailored to culture results. An orthopedic referral for immediate joint drainage must be considered.[25]
Other Issues
Systemic conditions may affect the knee joint. The following are examples:
- Connective tissue disorders such as Ehlers-Danlos syndrome may cause knee ligamentous laxity. Knee hypermobility and dislocation are common among affected patients and may lead to chronic joint pain.
- Skeletal dysplasia is a rare, congenital condition that may affect the knee.
- Vitamin D deficiency causes osteomalacia and may present with bowleggedness.
Proper management requires prompt assessment and intervention. Some of these conditions require lifelong care.