Introduction
Blood volume refers to the total amount of fluid circulating within the arteries, capillaries, veins, venules, and chambers of the heart at any time. The components that add volume to blood include red blood cells (erythrocytes), white blood cells (leukocytes), platelets, and plasma. Plasma accounts for about 60% of total blood volume, while erythrocytes make up roughly 40%, along with leukocytes and platelets.[1] The amount of blood circulating within an individual depends on size and weight, but the average human adult has nearly 5 liters of circulating blood. Women tend to have a lower blood volume than men. However, a woman's blood volume increases by roughly 50% during pregnancy.[2]
Blood volume is tightly regulated and related to multiple organ systems. Furthermore, it is closely associated with sodium content and hydration status. The maintenance of blood volume is crucial to normal function as it is necessary for the constant perfusion of body tissues. Blood volume can be increased or decreased by systemic dysfunction. Changes in blood volume can result in various clinical scenarios, such as hypovolemic shock or edema.
Two equations exist for estimating blood volume given the gender, height (H), and weight (W) of the patient. The Nadler equation is built upon the work of Dr. Allen in 1962, while the Lemmens-Bernstein-Brodsky equation is more accurate for higher ranges of body weight and body mass indices in patients without critical illnesses.
Nadler Equation[3]
- Men: Blood Volume = (0.3669 × H3) + (0.03219 × W) + 0.6041
- Women: Blood Volume = (0.3561 × H3) + (0.03308 × W) +0.1833
Lemmens-Bernstein-Brodsky Equation[4]
- Blood Volume = 70W/[√(body mass index/22)]
Organ Systems Involved
Multiple organ systems are involved in producing blood and regulating blood volume. These systems communicate with one another to optimally control blood volume.
The renal system, and more specifically the kidney, is primarily responsible for regulating blood volume. The kidney's primary function is to modify the solutes and water content of the blood through filtration, reabsorption, and secretion. As blood passes through the glomerulus of the kidney, solutes and water are filtered out depending on a variety of signaling molecules. Then, as the filtrate passes through the tubules, some filtrates are reabsorbed along with water. The amount of water and solute reabsorbed is what primarily regulates blood volume. If blood volume is too low, more filtrate reabsorbs; if blood volume is too high, less filtrate reabsorbs. The kidney is also responsible for the secretion of erythropoietin. Erythropoietin is the protein that signals the bone marrow to produce red blood cells. Therefore, the kidney is responsible for both the regulation and partial production of blood volume.
While blood is a component of the cardiovascular system, this system is hardly responsible for its regulation. Instead, the cardiovascular system maintains arterial pressure for the adequate perfusion of all bodily tissues. This system detects changes in blood volume and reflects it through increasing or decreasing arterial pressure. Reduced blood volume leads to collapsing vessels, reduced pressure, and subsequently reduced perfusion pressure. The cardiovascular system combats low blood volume by constricting blood vessels until the body reaches a blood pressure that restores proper perfusion pressure. Blood volume and blood pressure are interconnected through the renal and circulatory systems, specifically the renin-angiotensin-aldosterone system (RAAS).
As mentioned earlier, the skeletal system is responsible for producing blood cells that comprise blood volume. When signaled by erythropoietin, the bone marrow creates erythrocytes, which are eventually released into circulation. Leukocytes, which form a small portion of total blood volume, are also produced by the bone marrow when stimulated by colony-stimulating factors released from mature leukocytes. Lastly, the nervous system aids in regulating blood volume by interacting with all three other systems. It is responsible for some of the stimulus at the level of the glomerulus and the constriction of blood vessels through sympathetic nerve activity.
Function
Blood volume is necessary to maintain adequate perfusion to all of the tissues in the body. Nearly all cells in the body require replenishment of nutrients and a removal system for waste, both of which the blood provides. When a tissue loses its blood supply, ischemia occurs, potentially leading to an infarct after some time. Depending on the location of this tissue, an infarct could have a fatal effect. An infarct of the heart is a myocardial infarction; an infarct of cerebral tissue is a stroke.
Blood volume also functions in the maintenance of body osmolality. Osmolality refers to the balance of solutes and water within a solution, in this case, the blood. A properly functioning system maintains an osmolality of 275 to 295 mOsm/kg of water through water and sodium manipulation, primarily at the kidney.[5] When one of these two varies from the standard range, plasma osmolality changes and may increase or decrease plasma volume. Changing plasma osmolality results in an imbalance between intracellular and extracellular compartments. This imbalance can cause water entry or exit from cells. Overall, it may greatly increase or decrease blood volume. Increased blood volume is hypervolemia and decreased blood volume is hypovolemia.
Clinical Significance
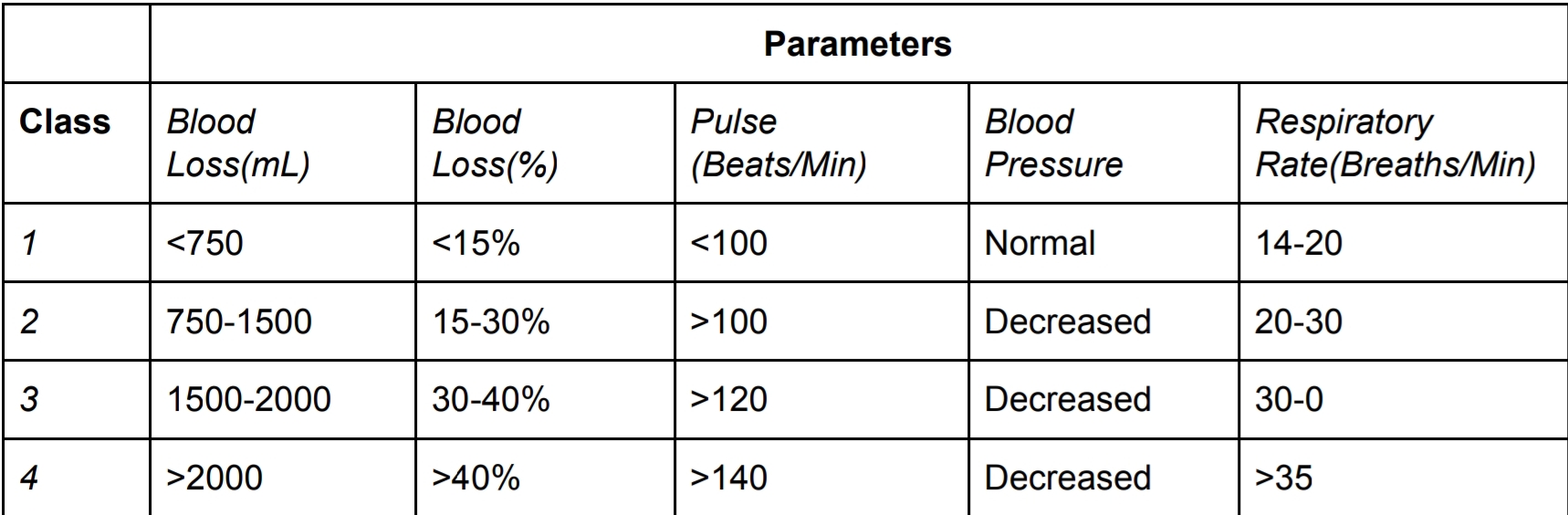
Both increased and decreased blood volumes have associated clinical complications. Hypovolemia can occur through a hemorrhage, sodium depletion, water loss, and the loss of plasma. Dehydration can also cause reduced blood volume but only occurs due to a lack of water. The two are distinct terms due to their effect on plasma osmolality, but both result in decreased blood volume.[6] Hypovolemia is classified as stages of hypovolemic shock which can be seen in the table below with corresponding vital signs for each stage.[7] The treatment of hypovolemic shock depends on the osmolality of the patient, and corresponding isotonic, hypertonic, or hypotonic fluids are administered. Hypovolemia may be monitored in the hospitalized patient through heart rate determination, systolic blood pressure, or central venous pressure devices.[8] When blood volume drops, regulatory mechanisms increase the pulse and respiratory rate in an attempt to restore regular perfusion while the blood pressure decreases.
Hypervolemia occurs when blood volume increases and can occur through renal failure, congestive heart failure, liver failure, excessive sodium intake, or any other dysfunction of sodium regulation.[8] Furthermore, prolonged hypertension may result in renal damage, eventually culminating in fluid imbalance. When sodium is retained in the body, water is as well. This retention results in increased plasma and subsequently increased blood volume. Uncontrolled hypervolemia results in fluid accumulation in various body cavities and other extracellular spaces. Ascites, pulmonary edema, and edema are all possible outcomes of hypervolemia.