Introduction
The foramen spinosum is a small circular foramen present posterolateral to the foramen ovale in the greater wing of the sphenoid. The greater wing of the sphenoid is a bony projection arising from both sides of the sphenoid body forming a part of the floor of the middle cranial fossa. Jakob Benignus Winslow coined the term foramen spinosum because of the foramen's location in the spinous process of the greater wing of the sphenoid.[1]
Structure and Function
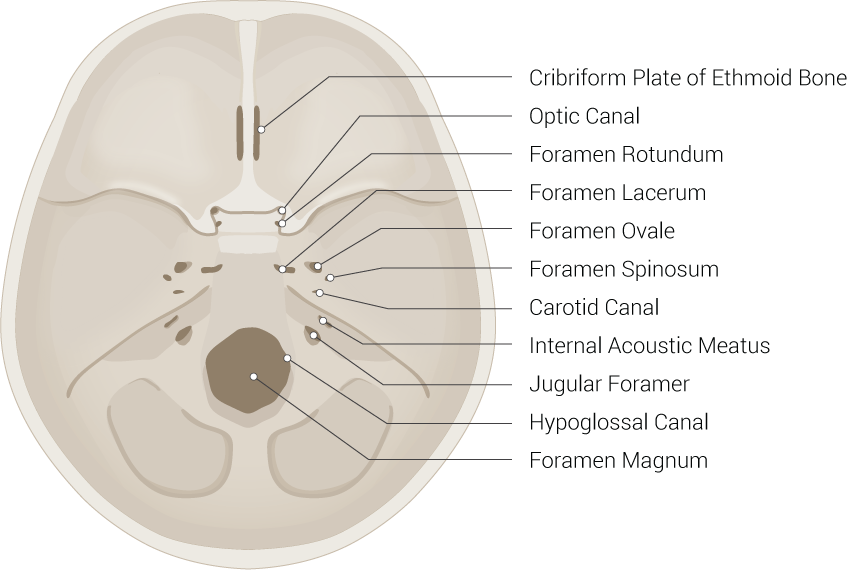
The foramen spinosum plays a role in connecting the infratemporal fossa with the middle cranial fossa along with other foramina like foramen ovale and foramen rotundum. The neurovasculature passing through the foramen spinosum includes the middle meningeal artery, the mandibular branch of the mandibular nerve or the nervus spinosus, and the middle meningeal vein. The middle meningeal artery, which is the largest of the three paired arteries that supply the meninges, supplies the dura mater and the calvaria, or skullcap. The anterior branch of the middle meningeal artery passes through the foramen spinosum, then runs underneath the pterion. The pterion is the region in which the frontal bone, parietal bone, and temporal bone along with the sphenoid bone meet. A blow to this region can cause a rupturing of the vessel causing an epidermal hematoma. This artery arises from the maxillary branch of the external carotid artery and will divide into anterior and posterior branches. Several smaller branches of this artery also appear around the foramen spinosum. The middle meningeal vein drains into the subclavian vein. The foramen spinosum is clinically significant since it is a comfortably identifiable anatomical landmark during neurosurgical and radiographic-based diagnostic procedures. In the adult population, the average diameter of the foramen spinosum is 2.63 mm.[2]
Embryology
The foramen spinosum derives from the first pharyngeal arch, which is also known as the mandibular arch, within the sphenoid. It begins to ossify eight months after birth and can take as long as seven years to develop fully into its bony ring-shaped formation.[2] The first pharyngeal arch forms during the fourth week of development and is located between the stomodeum and the first pharyngeal groove. The trigeminal nerve supplies the first pharyngeal arch. The sphenoid originates from neural crest cells.
Nerves
The mandibular branch of the mandibular nerve, which branches off of the trigeminal nerve, passes through the foramen spinosum and innervates the posterior portion of the dura mater of the middle cranial fossa. This nerve is otherwise known as the nervus spinosus. The nervus spinosus also supplies sensation to the cartilaginous part of the Eustachian tube. The mandibular branch then continues between the squamous and petrous portions of the temporal bone where it then enters and supplies the mastoid air cells and mastoid antrum.[3][4][3]
Physiologic Variants
The foramen spinosum approximately measures 2.25 mm in length in newborns and 2.56 mm in adults. In most cases, it is bilaterally present, but in a few individuals, there may be a unilateral or bilateral duplication of the foramen. In some individuals, the foramen spinosum may be smaller than the usual size, or it may be completely absent. Rarely when the foramen spinosum is absent, the middle meningeal vessels and the meningeal branch of the mandibular nerve pass through the foramen ovale. One study found an anomaly in the foramen spinosum in which the foramen appeared “channel-shaped,” providing direct access to the foramen ovale. This anomaly was unilateral and did not seem to have any accompanying abnormalities. Another potential defect in this area occurs when the middle meningeal artery originates directly from the persistent stapedial artery. In these cases, the foramen spinosum is typically either absent or reduced in size.[5][3]
Surgical Considerations
The foramen spinosum is a surgical landmark that serves as a guide during the microsurgery of the middle cranial fossa. One other notable surgical consideration relates to the middle meningeal artery that runs through the foramen spinosum, which is surrounded by the auriculotemporal nerve. The close association of the two can lead to unintended damage to the nerve during surgery. [6]
Clinical Significance
The proximity of the foramen spinosum to the foramen ovale and trigeminal nerve provides it with significant clinical relevance. The foramen spinosum acts as an anatomical landmark during neurosurgical procedures. Some example procedures include surgeries to treat trigeminal neuralgia, tumors, and epilepsy. There have been various techniques used to treat trigeminal neuralgia such as microvascular decompression, stereotactic radiosurgery, and percutaneous procedures including radiofrequency rhizotomy or balloon decompression. The percutaneous procedures, in particular, require cannulation of the foramen ovale which may become difficult due to the potential anatomical variation of the shape of the foramen. The majority of times the foramen ovale is oval in shape, but in some individuals, it is almond, round or slit-shaped. Having an idea of the anatomical location of the foramen ovale can play an essential role in facilitating successful CT-guided cannulation percutaneously. One study of interest looked at 100 dry human skulls (70 male, 30 female), studying them for any anatomical variations of the foramen ovale. Researchers measured the distance between the foramen oval and foramen spinosum. According to the study, the mean distance between the foramen ovale and foramen spinosum in the male subjects was 4 mm on the right and 3.8 mm on the left side, and in the females, 3.6 mm on the right and 3.2 mm on the left side, respectively. This estimated distance between the foramen ovale and foramen spinosum may ease our ability to locate the foramen ovale for percutaneous cannulation and can increase the chances of success of the procedure. There are other studies that have examined which angle of cannulation the foramen ovale has.[1][7][8]
The middle cranial fossa is the most commonly fractured fossa in accidental injuries. The fracture line follows a particular course. It starts from the parietal tuber, passes through the parietal bone, squamous temporal, petrous temporal bone, and usually involves the tegmen tympani, internal acoustic meatus, foramen ovale and may also involve the foramen spinosum due to its close proximity. Damage to the foramen spinosum or the temporal bone due to a head injury caused by a road traffic accident or direct trauma can sever the middle meningeal artery at the level of the foramen spinosum. This trauma can lead to bleeding between the skull and dura mater resulting in an epidural hematoma.[9][10]