Introduction
The arteries of the forearm are muscular arteries that originate from the brachial artery at its bifurcation into the ulnar and radial arteries in the cubital fossa. The division occurs anterior to the radius and ulna at approximately the level of the radial neck or radial tuberosity.[1][2] Soon after the bifurcation of the brachial artery, branches from the ulnar and radial arteries travel superiorly to anastomose with branches of the brachial artery around the elbow joint. These branches include the radial recurrent artery and the anterior and posterior ulnar recurrent arteries. Distal to the origins of these branches, the common interosseous artery originates from the ulnar artery and bifurcates into the anterior and posterior interosseous arteries. The recurrent interosseous artery branches off the posterior interosseous artery to travel proximally and anastomose with a branch of the deep brachial artery. The ulnar, radial, and anterior and posterior interosseous arteries course down the forearm. They branch into dorsal and palmar carpal arteries that supply the wrist and deep and superficial palmar branches that supply the hand. The arteries of the forearm supply the muscles and nerves of the forearm that control the hands. Anatomists have described several variants of the arterial anatomy. This activity will discuss in detail the anatomic details of the arteries of the forearm and their clinical significance.
Structure and Function
For clarity, the structure and function of the arteries of the forearm will be discussed separately for each artery.
Ulnar Artery
The ulnar artery is the larger of the two branches of the brachial artery at the level of its bifurcation.[3] At its origin, it has a reported inner diameter of approximately 4 mm.[4] It first courses inferomedially down the forearm, until approximately half-way between the wrist and elbow, after which it courses inferiorly along the medial forearm. At its origin, the ulnar artery courses deep to the superficial and intermediate muscles of the anterior compartment of the forearm. Specifically, it courses deep to the pronator teres, flexor carpi radialis, palmaris longus, and flexor digitorum superficialis and superficial to the flexor digitorum profundus. Shortly after its origin, the ulnar artery gives off two branches that course proximally to the elbow: the anterior and posterior ulnar recurrent arteries. It then gives off another branch, the common interosseous artery. At the level of the mid-forearm, the ulnar artery courses deep to the flexor digitorum superficialis and lateral to the flexor carpi ulnaris. It continues down the forearm between the flexor carpi ulnaris and flexor digitorum profundus. At the wrist, the ulnar artery gives off palmar and dorsal carpal branches, and courses deep to the palmar carpal ligament, through Guyon’s canal, lateral to the pisiform, and superficial to the flexor retinaculum. It then becomes the superficial palmar branch after giving off a tributary to the deep palmar arch.
The ulnar artery and its branches are responsible for blood supply to the medial forearm, including the bones and muscles of the forearm and the ulnar and median nerves. It is also responsible for part of the blood supply to the carpal bones and the hands, specifically of the medial hand and the medial two digits. The proximal branches help supply structures of the elbow joint.
Radial Artery
The radial artery is the smaller of the two branches of the brachial artery at the level of its bifurcation. It branches off the brachial artery anteromedial to the biceps tendon, and courses inferolaterally along the forearm.[5] It travels down the arm together with the superficial branch of the radial nerve, deep to the brachioradialis. In the distal forearm, it lies lateral to the flexor carpi radialis tendon. At the level of the distal radius, the radial artery sends off the superficial palmar branch, which anastomoses with the superficial palmar arch, and sends off palmar and dorsal carpal branches to the wrist, which anastomose with the carpal branches from the ulnar artery. The radial artery then courses through the floor of the anatomical snuffbox, through the first dorsal interosseous muscle, and sends off arterial branches to the hand, where it terminates as the deep palmar branch, the main blood supply to the deep palmar arch.
The radial artery mainly supplies blood to the wrist and hand, as it does not have many branches in the proximal forearm. It is the main blood supply of the lateral hand and lateral three digits. It forms part of the blood supply of several forearm muscles. It supplies the radial nerve and helps supply the elbow joint.
Radial Recurrent Artery
The radial recurrent artery branches laterally off the radial artery in the cubital fossa anterior to the biceps tendon.[6] It travels superiorly up the arm between the brachioradialis and brachialis muscles and crosses the elbow joint. It terminates by anastomosing with the radial collateral artery just proximal to the distal humerus. The radial recurrent artery provides blood supply to the elbow joint, brachialis, brachioradialis, and other forearm muscles.
Anterior Ulnar Recurrent Artery
The anterior ulnar recurrent artery is the first branch of the ulnar artery. It branches medially in the cubital fossa and travels superiorly up the arm between the brachialis and pronator teres.[7] It courses anterior to the medial epicondyle and anastomoses with the inferior ulnar collateral artery just proximal to the distal humerus. The anterior ulnar recurrent artery provides blood to the elbow joint and pronator teres muscle.
Posterior Ulnar Recurrent Artery
The posterior ulnar recurrent artery branches laterally off the ulnar artery directly below the origin of the anterior ulnar recurrent artery.[7] The posterior ulnar recurrent artery is larger than the anterior recurrent ulnar artery. It travels superoposteromedially between the flexor digitorum profundus and flexor digitorum superficialis, coursing posterior to the medial epicondyle, deep to the flexor carpi ulnaris. It anastomoses with the superior ulnar collateral artery proximal to the distal humerus. The posterior ulnar recurrent artery supplies blood to the elbow joint, flexor carpi ulnaris, and palmaris longus.
Common Interosseous Artery
The common interosseous artery branches medially off the ulnar artery distal to the origin of the posterior ulnar recurrent artery.[8] It then bifurcates into the anterior interosseous artery and posterior interosseous artery.
Anterior Interosseous Artery
The anterior interosseous artery branches off the common interosseous artery and travels inferiorly down the arm anterior to the interosseous membrane.[9] It travels with the anterior interosseous nerve, between the flexor digitorum profundus and flexor pollicis longus. At the level of the pronator quadratus, it bifurcates, with one branch continuing down the arm, anastomosing with the palmar carpal arch. The other branch pierces the interosseous membrane and travels along its posterior surface to anastomose with the posterior interosseous artery, eventually anastomosing with dorsal carpal arch. The anterior interosseous artery contributes to the blood supply of the radius, ulna, flexor digitorum profundus, flexor pollicis longus, and pronator quadratus.
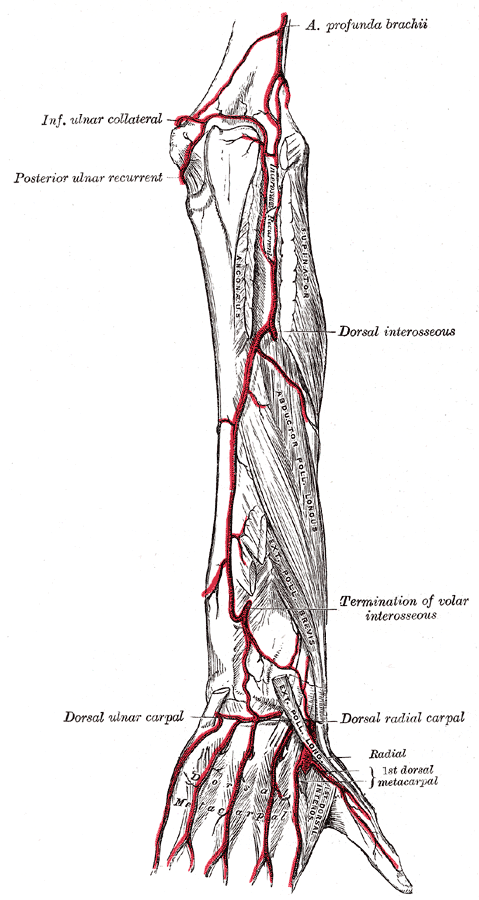
Posterior Interosseous Artery
The posterior interosseous artery branches off the common interosseous artery and travels inferiorly down the arm shortly before piercing the interosseous membrane and giving off a branch called the recurrent interosseous artery at the level of the supinator.[10] The posterior interosseous artery then courses inferiorly, posterior to the interosseous membrane. It travels deep to the supinator muscle and superficial to the abductor pollicis longus, extensor pollicis longus, and extensor indicis. At the distal forearm, it anastomoses with the anterior interosseous artery, and this artery continues down the arm to join the dorsal carpal arch. The posterior interosseous artery supplies blood to the ulna, abductor pollicis longus, supinator, and extensor muscles of the forearm.
Recurrent Interosseous Artery
The recurrent interosseous artery branches off the posterior interosseous artery at the level of the supinator muscle.[10] It then courses superiorly along the arm deep to the anconeus and superficial to the supinator, between the lateral epicondyle and the olecranon. It anastomoses with the middle collateral branch of the deep brachial artery just proximal to the distal humerus.[11] The recurrent interosseous artery provides some of the blood to the elbow joint.
Embryology
There is more than one theory on the embryologic development of the arteries of the arm. One theory suggests that the seventh intersegmental artery gives off a branch, the axis artery, which distally branches into the axillary, brachial, and interosseous arteries.[12] A separate superficial brachial artery allows the brachial and axillary branches to anastomose. The medial, ulnar, and radial arteries then form, and the superficial brachial artery involutes. The radial artery initially originates proximal to the ulnar artery, but as time progresses, the portion proximal to the ulnar artery involutes. Many of the variants in forearm anatomy, especially of the radial artery, are hypothesized to be a result of improper involution or branching during embryologic development.
The basis of another theory is a gradually developing capillary network, which differentiates along with other structures in the fetal arm.[13] At approximately 30 days into fetal development, the upper limb has a capillary network. By 32 days, an axial trunk develops, starting as a subclavian artery at the proximal part of the primitive limb. Distal to this artery is the capillary network. Over the next few days, the axial trunk continues differentiating, now forming an axillary artery distal to the subclavian artery. By 41 days, a brachial artery is developed and has branches proximal to the elbow. Distal to the elbow, the capillary network remains. Within a few days, as structures distal to the elbow are differentiating, the ulnar, median, interosseous, and radial arteries develop. As the limb continues to differentiate, the arteries become more developed. Using this theory, there is a potentially huge number of anatomic variants concerning the arteries of the forearm, because of possible changes in capillary differentiation pattern.[14]
Nerves
The nerves of the forearm include the median nerve, ulnar nerve, radial nerves, and their branches.[15][16][17] The median nerve gives off the anterior interosseous and palmar cutaneous branches. The anterior interosseous nerve travels with the anterior interosseous artery. The ulnar nerve travels with the ulnar artery from the mid-forearm to the wrist. It gives off the palmar cutaneous and dorsal cutaneous nerves. The radial nerve divides into the posterior cutaneous nerve of the forearm, the superficial branch of the radial nerve, and the posterior interosseous nerve. The superficial branch travels with the radial artery down the forearm, and the posterior interosseous nerve travels with the posterior interosseous artery. There are also lateral and medial cutaneous nerves of the forearm that branch off other parts of the brachial plexus.
Muscles
Several different arteries supply the various muscles of the forearm. Clinically, this allows for harvesting of the forearm arteries without causing permanent damage to the arm. The common interosseous and recurrent interosseous arteries are not known to supply any muscles. For clarity, the arterial supply to the forearm musculature is listed below, organized by the artery.
- Ulnar Artery: flexor digitorum profundus, flexor digitorum superficialis
- Radial Artery: extensor carpi radialis brevis, extensor carpi radialis longus, flexor carpi radialis, flexor digitorum superficialis
- Radial Recurrent Artery: brachialis, brachioradialis, extensor carpi radialis brevis, extensor carpi radialis longus, supinator
- Anterior Ulnar Recurrent Artery: pronator teres
- Posterior Ulnar Recurrent Artery: flexor carpi ulnaris, palmaris longus
- Anterior Interosseous Artery: flexor digitorum profundus, flexor pollicis longus, pronator quadratus
- Posterior Interosseous Artery: abductor pollicis longus, extensor carpi ulnaris, extensor digiti minimi, extensor digitorum, extensor indicis, extensor pollicis brevis, extensor pollicis longus, supinator
Physiologic Variants
There are many reported variants of the arteries of the forearm. Sometimes, patients undergoing procedures using radial artery access are found to have unusual arterial anatomy. One of the most common variations is a called the brachioradial artery, which is a radial artery that has an origin-proximal to the cubital fossa, higher on the brachial artery. Research reports the presence of a brachioradial artery in 13.8% of limbs.[18] It most commonly branches off the upper third of the brachial artery or the axillary artery. It travels down the upper arm superficial to the median nerve and travels along the usual route of the radial artery in the forearm. Another variation is called a superficial radial artery. It crosses the anatomical snuffbox superficially to the tendons rather than along the floor of the snuff-box. There are reports of this variant in 0.52% of cadaveric limbs. Another variation is called a superficial brachioulnar artery, which is an ulnar artery that has an origin-proximal to the cubital fossa, most commonly on the upper third of the brachial artery or the axillary artery. In the forearm, it travels a more superficial course than the normal ulnar artery, coursing superficial to the flexor muscles. This artery then resumes the usual course of the ulnar artery at around the middle third of the forearm. Another variant called a brachioulnar artery presents in 0.26% of cadaveric limbs. This variation is an ulnar artery with an origin-proximal to the cubital fossa, but then courses in the usual path of the ulnar artery in the forearm. Another variation is called a superficial brachioulnoradial artery, reported in 0.52% of cadaveric limbs. In this variation, the ulnar and radial arteries originate off the superficial brachial artery, while the common interosseous artery is the continuation of the normal brachial artery. Reports also exist of duplicated or absent radial and ulnar arteries. Another variation is called a persistent median artery. The median artery is an embryologic artery that supplies blood to the distal limb of the fetus but regresses once the radial and ulnar arteries develop. One study reported its prevalence in one study as 26.7% of pediatric patients.[19] These variations can have significant clinical implications for patients undergoing procedures or treatments requiring the use of the upper extremity arteries.
Surgical Considerations
The radial artery is a popular access site for endovascular procedures such as cardiac catheterization and uterine fibroid embolization. It also can serve as a flap in reconstructive surgery.[20] Both the ulnar and radial arteries are useful as potential coronary artery bypass grafts.[21] The radial artery is the primary site for placement of arterial lines that have a use for blood pressure monitoring during surgery. Due to collateral circulation at the wrist and hand, which receive blood from the radial, ulnar, and interosseous arteries, occlusion or harvest of the radial or ulnar arteries usually does not cause complications such as ischemia of the hand. However, patients with anatomic variations of the arteries of the hand can develop ischemia. The radial artery can spasm during the placement of catheters or sheaths into it, and medications such as nitroglycerin and verapamil can be used to prevent or reduce spasm.
Clinical Significance
Pulse
The most common place to evaluate a patient’s pulse is the radial artery at the wrist. Due to its superficial course near the lateral wrist, the radial artery is easily palpable. The ulnar artery is also palpable at the medial aspect of the wrist. Both arteries can be occluded with manual compression, which is done in the Allen test. The Allen test assesses the collateral circulation of the hand prior to performing any procedures that could involve the forearm arteries.
Arterial Lines
The radial artery is the primary site for the placement of arterial lines used for blood pressure monitoring. It is also the most common artery punctured to procure a sample for arterial blood gas analysis. When arterial catheters are left in for several days, complications such as infection, spasm, and occlusion can occur.[20]
Radial Artery Access
The radial artery is commonly used as an access site for endovascular procedures. This is becoming more common as evidence suggests that there are fewer vascular access complications when using the radial artery compared to the femoral artery, without any negative effects on the success of the procedure.[22] Radial access is used for cardiac catheterization, uterine fibroid embolization, renal artery stenting, prostate artery embolization, peripheral arterial intervention, visceral arterial intervention, and many other endovascular procedures. Anatomic variants such as a brachioradial artery may make procedures using radial access more difficult. The vessel may be tortuous near its origin and navigating it could prove difficult. The radial artery has a smaller diameter than the common femoral artery, which limits the size of the sheaths and catheters that can be used.
Dialysis Fistulas
The most common arteriovenous fistula used for hemodialysis is a radiocephalic fistula, between the radial artery and the cephalic vein.[23] These fistulas can be created in many places on the forearm, from the proximal radial artery to the distal radial artery at the wrist. The location depends on several factors, including the diameter of the radial artery and cephalic vein. Other vessels used for dialysis fistulas include the brachial artery, cephalic vein, and basilic vein (for brachiocephalic and brachiobasilic fistulas). One reason that radiocephalic fistulas are preferred is that its distal location leaves the other two more proximal locations available in the event of fistula failure.
Coronary Artery Bypass Grafting
The radial artery can be harvested for use in coronary artery bypass grafting. Ischemia of the hand is prevented in most cases due to the extensive collateral circulation from the ulnar and interosseous arteries. Evidence suggests that radial artery grafting is superior to saphenous vein grafting, as data shows a lower incidence of occlusion and adverse cardiac events when using a radial artery graft.[24] The ulnar artery can also be used as a graft. When one of the arteries of the forearm is harvested for grafting, the other arteries of the forearm compensate by increasing their diameter and blood flow.[20] It is important to evaluate the collateral circulation of the hand using the Allen test or with ultrasound before harvesting one of the arteries. This can help prevent any ischemic complications.
Forearm Flap Surgery
Another area of clinical significance for the arteries of the forearm is in reconstructive surgery using forearm flaps. In these surgeries, tissue from the forearm is harvested along with its blood supply and then attached to the area of the body in need of the flap. Keeping the blood supply together with the tissue allows for healing in a damaged area that cannot supply blood to a skin graft. The most common forearm flaps are the radial forearm free flap and ulnar forearm free flap.[25] There are published reports of other forearm arteries and their perforators being used for forearm flaps, including the posterior ulnar recurrent artery, the posterior interosseous artery, and the anterior interosseous artery.[7][26][27] These arteries and their perforating branches can be safely harvested with the adjacent tissues without detriment to the arm because of the extensive collateral circulation that exists in the forearm and hand.
Other Issues
Calciphylaxis or calcific uremic arteriolopathy is an arterial calcification, typically found in patients with long-term kidney disease. Radiography shows the process of arterial calcification, for example, in the forearm. The radial pulse may appear very strong; the causes remain unclear.
The adventitious cystic disease of the radial artery is a pathology that is difficult to find, but real. It appears as a painful mass in the forearm. It attaches with a stem at the intra-mural level of the artery. The approach is always surgical.