Continuing Education Activity
Talocalcaneal coalition is an abnormal connection between the talus and calcaneum bones, which can cause painful, rigid, flat feet in older children and adolescents. The condition has 3 types of coalition: fibrous, cartilaginous, or bony, which can mature into a stiff cartilaginous bar and ossify into a rigid bar. This can result in severe symptoms for those affected. Clinicians in orthopedic surgery need to be aware of this condition, but it can also present in primary care or emergency settings. Therefore, accurate triage and consultation are essential for long-term prognosis. This activity reviews the condition's epidemiology, pathophysiology, evaluation, and management, including the clinical decision-making algorithm for surgical or non-surgical intervention. The critical role of an interprofessional, collaborative team in managing this complex condition is emphasized.
Objectives:
Identify the presentation of a patient with the talocalcaneal coalition in a clinical setting and describe typical imaging findings.
Screen children and adolescents showing signs of rigid flat feet for a potential talocalcaneal coalition.
Apply comprehensive knowledge of talocalcaneal coalition management options, considering conservative measures versus surgical intervention.
Implement interprofessional collaboration that can enhance outcomes for patients with a talocalcaneal coalition.
Introduction
The talocalcaneal coalition is a frequent cause of painful flatfoot in older children or adolescents. The talocalcaneal coalition is an anomalous connection between the talus and the calcaneus. The talocalcaneal coalition can be fibrous (syndesmosis), cartilaginous (synchondrosis), or bony (synostosis).[1] Although the anomaly is present at birth, it becomes symptomatic only when the abnormal fibrous connection matures into a stiff cartilaginous bar and, over time, ossifies to become a rigid bar. The age of onset is typically between 12 to 15. [2]
It is described as a peroneal spastic flat foot as the peroneal muscles spasm in a painful, rigid flat foot. Peroneal spasm tends to refer to the contracted peroneal tendons in a rigid flatfoot, however only 3.13% of patients with talocalcaneal coalitions present with this symptom.[3]
The subtalar joint has 3 facets: anterior, middle, and posterior, that articulate with the respective facets of the calcaneum. Historically, the middle facet is described as being the most commonly involved in talocalcaneal coalitions.[4] However, other authors reported the posterior facet having a higher involvement rate than the middle facet.[5] The middle facet is most commonly involved in the talocalcaneal coalition. The posterior facet is the largest, and the anterior facet is the smallest. 4 recognized anatomical patterns of the anterior and middle facets: a single small middle facet, a large middle facet that extends posteriorly, a middle facet that extends anteriorly, and both facets-middle and anterior in the medial compartment. The size of the talocalcaneal coalition determines the successful outcome after its resection.
The talocalcaneal coalition is the second most common tarsal coalition in the foot after the calcaneonavicular coalition. Tarsal coalitions cause gradual flattening of the medial longitudinal arch, resulting in a flat foot and stiffness of the subtalar joint.[2]
Archaeological evidence points to the presence of the tarsal coalitions in the Mayan and pre-Columbian Indian civilizations. Zuckerkandl described the anatomy of a talocalcaneal coalition in 1877. Slomann (1921), Badgeley (1927), and Harris and Beath (1948) associated the tarsal coalitions with peroneal spastic feet.[6]
Etiology
Talocalcaneal coalitions can be differentiated into congenital and acquired etiologies. The congenital type is the most common due to mesenchymal segmentation and differentiation failure.[3] The authors propose an autosomal dominant inheritance pattern with variable penetrance. The coalitions initially present as fibrous unions and may undergo metaplasia to cartilage or bone. Pfizner, on the other hand, theorized coalitions resulted from accessory bones that ossified into adjacent bones. Harris later disproved this theory by observing coalitions in fetuses.[7] The acquired type is less common due to trauma, degeneration, inflammatory arthritis, neoplasia, or infections of the hindfoot or midfoot. Tarsal coalitions are associated with Apert syndrome, Nievergelt-Pearlman syndrome, and clubfoot deformities.[6][8]
Epidemiology
The prevalence of the tarsal coalition is 1% to 2%, although cadaveric studies have established a prevalence of 13%[9]. The talocalcaneal coalition accounts for 45% of total tarsal coalitions. The talocalcaneal coalition is symptomatic in the early teenage years when the preexisting coalition ossifies around ages 12 to 15.
Pathophysiology
In a normal gait, the subtalar joint is pronating and supinating. When the foot is in the stance phase, the leg internally rotates, and in the toe-off phase, the leg externally rotates due to the closed chain movement. In a subtalar coalition, this torque converter movement gets lost, leading to increased stress on the neighboring joints, especially the ankle and talonavicular joints, leading to laxity in the ankle joint and beaking at the talar neck, leading to traction spurs. A primary impingement caused by the presence of an accessory facet in a child or young adult results in rigid flatfoot deformity leading to peroneal spasm.[10]
Histopathology
Few studies have looked at histological presentations of tarsal coalitions. Kumai and colleagues first described the microscopic presentation of non-osseous coalitions as fibrocartilaginous tissue with vascular proliferation localized at the coalition borders. The osteoblastic and osteoclastic activity was also identified at the bone boundary, though no inflammatory cells or nerve elements were seen at the coalition site.[11] In a 2022 systematic review, the authors found most of the coalitions in their adult population were osseous unions followed by fibrocartilaginous.[3]
History and Physical
Most coalitions are not symptomatic. The symptomatic presentation is of an adolescent with repeated ankle sprains and pain. The onset of pain is either insidious or sudden when associated with an ankle sprain. The pain is usually aggravated by running, jumping, or prolonged standing and is typically relieved by rest. Pain can be localized distal to medial malleolus at the coalition's site, ankle joint, talonavicular joint, sinus tarsi, medially under the head of the plantarflexed talus, and laterally over the peroneal tendons.[9] The patient can have associated calf pain due to a tight gastrosoleus muscle leading to peroneal spasms. The pain depends on the stage of metaplasia of the coalition.
On inspection, the hindfoot is in valgus, forefoot abduction, and varying degrees of medial longitudinal arch flattening. The arch does not reform on tiptoeing or Jack's test. The patient is unable to stand on the lateral aspect of the foot. The subtalar movement is reduced (fibrous) or completely absent (osseous). The gastrosoleus complex is tight, and lack of subtalar movement leads to peroneal spasms on forced inversion. A double medial malleolus sign may present: prominence palpated inferior to the medial malleolus, representing the medial facet.
Evaluation
Standing anteroposterior, lateral, and Harris views are helpful. Radiographs of the ankle joint may demonstrate an apparent ball-and-socket ankle. On the lateral view, talar beaking occurs at the distal dorsal aspect of the talar head near the talonavicular joint, and this is due to abnormal biomechanical stresses at the talonavicular joint. Talar beaking is 48% sensitive and 91% specific for diagnosing a talocalcaneal coalition. The lateral radiographs reveal the C sign, which results from the bony continuity of the inferomedial border of the talus and the posteroinferior aspect of the sustentaculum tali. First described by Lateur et al, the C sign is 88% sensitive and 87% specific. An absent middle facet sign with 100% sensitivity and 42% specificity is visualized on a true lateral radiograph. The sustentaculum tali is dysmorphic, and it appears enlarged and rounded (often referred to as the Drunken Waiter sign) with 82% sensitivity and 70% specificity.[12] The presence of the C-sign has been recorded in 69% of talocalcaneal cases, the beaking sign in 29%, dysmorphic sustentaculum in 75%, and the absence of the middle facet in 58% of cases, according to Phyo and colleagues.[13]
CT imaging is best used to visualize and assess talocalcaneal coalitions perpendicular to the subtalar joint in 1.0 x 1.0 mm slices to rule out associated coalitions and preoperative workup.[7] CT imaging is generally upfront in evaluating osseous subtalar coalitions but indeterminate in cases of a non-osseous coalition. CT scan is helpful to determine the location, size, and extent of the coalition. The posterior facet of the calcaneum width and the relative cross-sectional area of the talocalcaneal coalition to the area of the posterior facet of the calcaneus are calculated to determine the surgical procedure and outcome. The talocalcaneal coalitions are resectable if the size ratio is less than 50%, a wide posterior articular facet is apparent, and under 16° of hindfoot valgus deformity is measured on the coronal CT image.[14]
Another useful classification system has been proposed based on 3-dimensional CT reconstructions, which may help define the size, location, and orientation of talocalcaneal coalitions.
Mubarak et al divided the talocalcaneal coalition into 5 types[15]:
- Type 1- Linear
- Type 2- Linear with posterior hook
- Type 3- Shingled
- Type 4- Complete osseous
- Type 5- Posterior
CT SPECT scan can be used to localize the precise location of the symptoms.
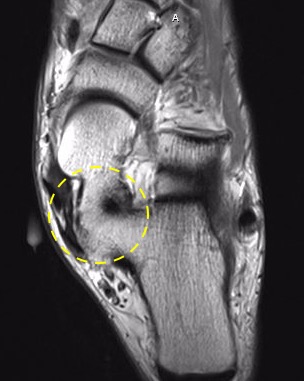
MRI scanning is useful for ruling out fibrous or cartilaginous coalitions and assessing bone marrow edema at the suspected coalition site, implying mechanical stress.[7] MRI findings can evaluate inflammatory changes in the neighboring tendons (see Image. Talocalcaneal Coalition on MRI).
Treatment / Management
Initial management consists of non-operative management. Conservative management is successful only in one-third of the cases.
Non-Operative Treatment
Conservative therapy aims to alleviate the discomfort associated with the coalition. Patients with mild to moderate symptoms may respond well to shoe modifications. Medial arch supports and custom-molded orthotics can help control or prevent motion of the painful subtalar joint and reduce the medial-lateral hindfoot force to minimize pain.
Pain-relieving measures include anti-inflammatory medications, steroid injections, and complete immobilization in a below-knee cast. In severe pain, 6 weeks of complete immobilization may be justified, with symptomatic relief obtained in roughly 30% of patients.[16] The patient can recommence activities if symptoms resolve with conservative measures. Symptoms often subside when the facet ossifies, especially if the heel is neutral.
If conservative measures fail, the patient should undergo re-evaluation for surgical intervention. The surgical procedure is necessary when (1) pain is not relieved and (2) if the non-operative management fails to resolve the recurrent ankle sprains.
Operative Measures
1. Resection of the coalition is the treatment of choice if the patient is aged less than 16. The results are less predictable than the resection of calcaneonavicular coalitions. The resection site is usually interposed by fat, bone wax, flexor hallucis longus tendon, allograft, or cartilage allograft to prevent a recurrence.[17] If mild hindfoot deformity is present, a sinus tarsi implant is an option, or a corrective calcaneal lengthening or medial calcaneal shift osteotomy is used to correct the foot deformity.
According to Wilde et al, 3 criteria need to be met for the resection to be successful.
- The area of the middle facet relative to the posterior facet should be less than 50%.
- The posterior facet should have wide and thick cartilage, and no degenerative changes should exist.
- The hindfoot valgus should be less than 16°.
A recent review article by Mubarak and Murphy advocated the restoration of hindfoot motion regardless of the size of the coalition[18]. If indicated, the resection may be accompanied by calf or peroneal lengthening. Incomplete resection is the most common cause of failure in the surgical management of talocalcaneal coalitions.
2. Subtalar fusion is necessary if the area of the talonavicular coalition is greater than 50%.[19] Arthroscopic subtalar joint fusion has also been described for talocalcaneal coalitions, with 81% of patients reporting excellent midterm outcomes.[20] A study by Saraiva and colleagues reported no nonunions in their posterior arthroscopic approach.[21]
3. Triple fusion (subtalar fusion with talonavicular and calcaneocuboid fusion) is associated with previously failed resection and associated degeneration in the Choparts joints (calcaneocuboid and talonavicular joints).
Differential Diagnosis
The talonavicular coalition requires differentiation from:
- Calcaneonavicular coalition - identified by lateral pain in the foot and an anteater sign on imaging
- Congenital vertical talus - rocker-bottom foot associated with a vertical talus on the imaging, uncorrected during dorsiflexion of the foot
- Calcaneovalgus foot - intrauterine positional packaging deformity characterized by hindfoot eversion and dorsiflexion - these contractures can sometimes lead to flexible flat foot deformities in the feet in adulthood
- Pes planovalgus
- Accessory navicular bone - can present with painful flat foot
- Tumors or rheumatoid arthritis in the subtalar joint
Prognosis
The conundrum with the talocalcaneal coalition is that patients do not manifest symptoms until they are aged 12 to 15. Flexible flat feet are common in children, and in most children, the reconstitution of the medial longitudinal arch occurs with age. Most patients (75%) are asymptomatic, and no treatment is necessary.[22] The minority with rigid symptomatic flat feet require assessment and early evaluation to diagnose talocalcaneal coalition for better outcomes. The spectrum of symptoms depends on the degree of ossification, ie, the metaplasia of the fibrous coalition into osseous synostosis. More commonly, the patients are diagnosed late, minimizing the chances of an early intervention.
Complications
In a neglected symptomatic talocalcaneal coalition, the natural progression would lead to restricted subtalar joint motion with progressive hindfoot valgus. As the rotary motion of the subtalar joint is restricted, the calcaneus goes into a fixed valgus position to compensate for the lack of external rotation of the foot during gait.[4] However, it should be noted that the calcaneus may be neutral or in a varus position.[23] [24] The progressive restriction of subtalar motion leads to degeneration in the subtalar, ankle, Choparts, and forefoot joints.[7]
Complications of resection of a talocalcaneal coalition include recurrence of the coalition, damage to posteromedial structures (flexor digitorum longus, tibialis posterior, flexor hallucis longus, and posterior tibial neurovascular structures), persistent discomfort, superficial infections, minor wound problems, scar sensitivity, hypertrophy, mild paraesthesia.[20]
Patient-reported outcome measures (PROMs) after surgical excision of a tarsal coalition reveal that over 70% of patients' activities are not subject to restriction from pain, and their functional outcome is good.[25]
Postoperative and Rehabilitation Care
Postoperative care following a coalition resection varies according to current literature. Some authors recommend immediate weight-bearing as tolerated, while others recommend immobilization for 2 to 3 weeks.[26][27]
Hubert and colleagues recommend 2 weeks of immobilization and 4 weeks of partial weight-bearing for resection with an interpositional graft. In their study cohort, patients completed physical therapy and returned to full weightbearing at 6 weeks.
Subtalar joint arthrodesis for treating medial facet coalition results in good outcomes with 2 weeks of non-weightbearing followed by progressive weight-bearing over the next 6 weeks. According to some studies' postoperative regimen, returning to normal shoe gear occurs around 8 to 12 weeks.[21]
Mosca and Bevan discussed their technique for calcaneal lengthening osteotomies for talocalcaneal coalitions. The authors recommend a similar postoperative protocol of calcaneal lengthening osteotomy for the treatment of symptomatic flatfoot. In their study, the patients remained non-weight-bearing for 8 weeks.[9]
Consultations
Recommended but not limited to:
- Podiatrists
- Orthopedic surgeons
- Physical therapists
- Orthotists
Deterrence and Patient Education
Patient education and a conservative approach can prevent the need for surgical intervention.
- Activity modification, including temporary discontinuation of the pain-inducing activity
- Regular stretches of the calf muscles if the patients are Silverskiold positive
- Using non-steroidal anti-inflammatory drugs (eg, ibuprofen, naproxen) for symptom relapses
- Judicious use of orthotics to correct and accommodate the mild to moderate foot deformities in the subtalar coalition
- If symptoms persist, then careful evaluation and appropriate testing before determining next steps of medical management
Enhancing Healthcare Team Outcomes
Talocalcaneal coalitions are asymptomatic in three-quarters of the population. The diagnosis poses a dilemma. The screening is best evaluated in the primary care setting, and then the patient is referred to a podiatric or orthopedic surgeon or physiotherapist for further workup. Diagnosis and management require the efforts of an interprofessional team.
Symptomatic patients can effectively manage their condition with the help of orthotics, physiotherapy, and pain relief medication. Conservative treatment of talocalcaneal coalition requires an interprofessional approach with physiotherapists and orthotics. Patient and caregiver education, combined with guidelines from the managing facility, is crucial for a successful outcome. A proper history and clinical examination supplemented by radiographs, CT, 3D CT, and MRI images are essential for diagnosing the condition and planning for future surgical intervention. The radiologist plays a vital role in surgical planning by calculating the coalition's size and area. Orthopedic nursing staff can prove helpful, assisting in procedures, answering patient questions, providing a bridge between therapists and the managing clinicians, and offering patient counsel. Surgical management is advocated based on the size, shape, and relation of the hindfoot valgus, typically at centers with multidisciplinary consults. The interprofessional approach to talocalcaneal coalitions is most appropriate for optimal management.