[2]
Jurkovich GJ, Hoyt DB, Moore FA, Ney AL, Morris JA Jr, Scalea TM, Pachter HL, Davis JW. Portal triad injuries. The Journal of trauma. 1995 Sep:39(3):426-34
[PubMed PMID: 7473903]
[3]
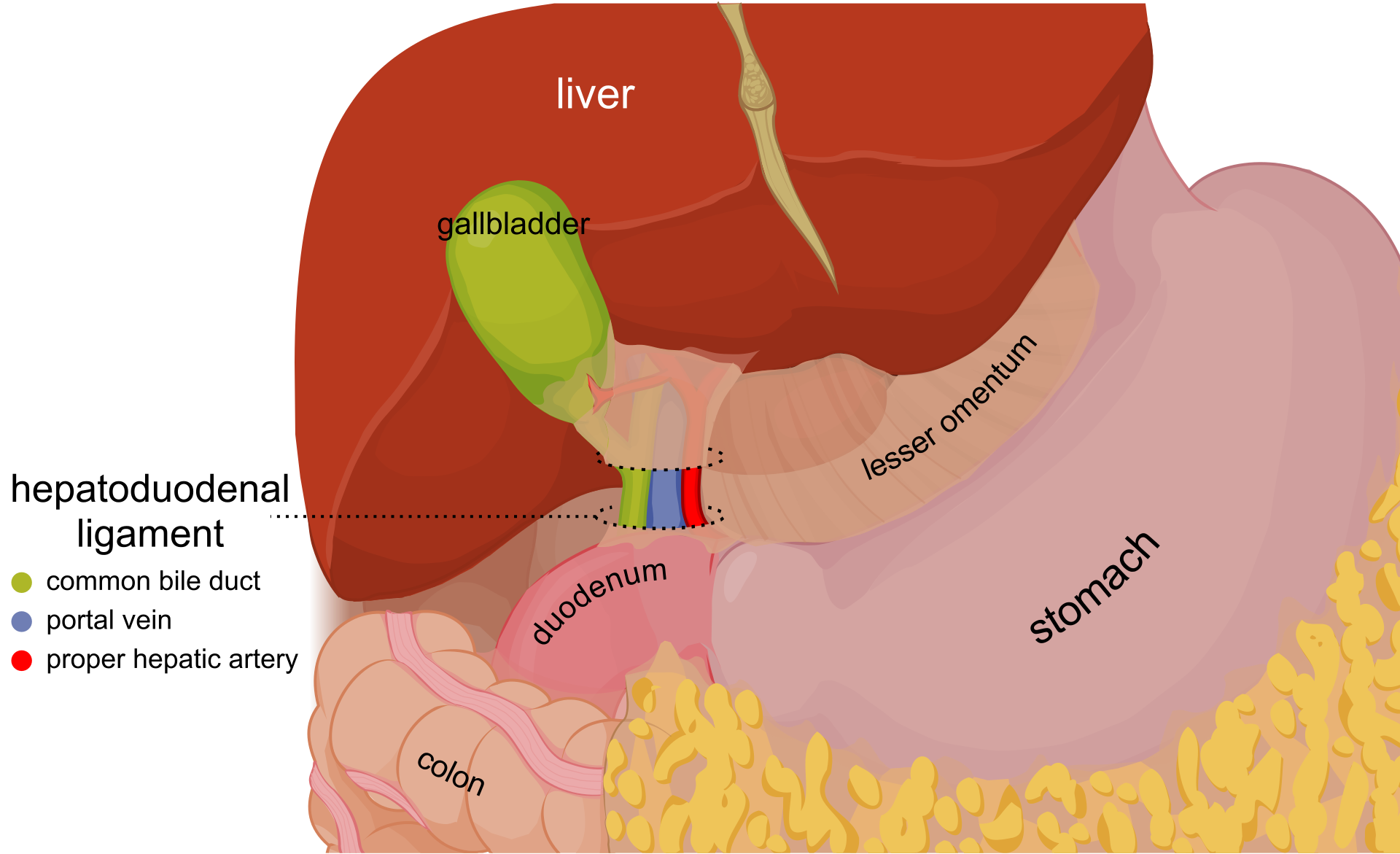
Takahashi N, Itoh K, Itoh H, Haba H, Ishii Y. [Anatomy of hepatoduodenal ligament on MR imaging]. Rinsho hoshasen. Clinical radiography. 1989 Dec:34(13):1585-9
[PubMed PMID: 2622050]
[5]
Thomas JM, Van Fossen K. Anatomy, Abdomen and Pelvis: Foramen of Winslow (Omental Foramen, Epiploic Foramen). StatPearls. 2024 Jan:():
[PubMed PMID: 29489171]
[6]
Qiao JL, Sun J, Li J, Zhang JJ, Meng XK. Liver dual arterial blood supply maintains liver regeneration: Analysis of signaling pathways in rats. Molecular medicine reports. 2018 Jan:17(1):979-987. doi: 10.3892/mmr.2017.7961. Epub 2017 Nov 3
[PubMed PMID: 29115531]
Level 2 (mid-level) evidence
[7]
Ibukuro K, Fukuda H, Tobe K, Akita K, Takeguchi T. The vascular anatomy of the ligaments of the liver: gross anatomy, imaging and clinical applications. The British journal of radiology. 2016 Aug:89(1064):20150925. doi: 10.1259/bjr.20150925. Epub 2016 May 10
[PubMed PMID: 27163944]
[9]
Noussios G, Dimitriou I, Chatzis I, Katsourakis A. The Main Anatomic Variations of the Hepatic Artery and Their Importance in Surgical Practice: Review of the Literature. Journal of clinical medicine research. 2017 Apr:9(4):248-252. doi: 10.14740/jocmr2902w. Epub 2017 Feb 21
[PubMed PMID: 28270883]
[10]
Delva E, Camus Y, Paugam C, Parc R, Huguet C, Lienhart A. Hemodynamic effects of portal triad clamping in humans. Anesthesia and analgesia. 1987 Sep:66(9):864-8
[PubMed PMID: 3619092]
[11]
Alessandrino F, Ivanovic AM, Souza D, Chaoui AS, Djokic-Kovac J, Mortele KJ. The hepatoduodenal ligament revisited: cross-sectional imaging spectrum of non-neoplastic conditions. Abdominal radiology (New York). 2019 Apr:44(4):1269-1294. doi: 10.1007/s00261-018-1829-0. Epub
[PubMed PMID: 30448917]
Level 2 (mid-level) evidence
[12]
Lee SL,Lee HH,Ko YH,Song KY,Park CH,Jeon HM,Kim SS, Relevance of hepatoduodenal ligament lymph nodes in resectional surgery for gastric cancer. The British journal of surgery. 2014 Apr;
[PubMed PMID: 24615472]
[13]
Okada Y, Yao YK, Yunoki M, Sugita T. Lymph nodes in the hepatoduodenal ligament: US appearances with CT and MR correlation. Clinical radiology. 1996 Mar:51(3):160-6
[PubMed PMID: 8605744]
[14]
Taylor I, Bennett R, Sherriff S. The blood supply of colorectal liver metastases. British journal of cancer. 1978 Dec:38(6):749-56
[PubMed PMID: 743492]
[15]
Sharma M, Rameshbabu CS, Dietrich CF, Rai P, Bansal R. Endoscopic ultrasound of the hepatoduodenal ligament and liver hilum. Endoscopic ultrasound. 2018 May-Jun:7(3):168-174. doi: 10.4103/2303-9027.193584. Epub
[PubMed PMID: 27824022]