Continuing Education Activity
Talar neck fractures are uncommon but can have life-altering consequences and are typically associated with high-energy mechanisms and multiple traumas. This continuing medical education (CME) course offers an in-depth exploration of talar neck fractures, covering their evaluation, treatment strategies, and potential complications. Given the limited availability of high-quality literature for these injuries, this course aims to equip healthcare professionals with evidence-based insights and best practices in managing talar neck fractures.
This activity explores the intricacies of talar neck fractures, emphasizing the critical role of the interprofessional team in the patient's care. Participants gain a comprehensive understanding of the challenges posed by these injuries, such as severe soft tissue damage, bony comminution, and frequent fracture displacement. The consequences of talar neck fractures can be devastating and include permanent stiffness, deformity, and pain, often leading to hindfoot arthrosis. More than 90% of displaced talar neck fractures result in hindfoot arthrosis. The course addresses surgical treatment with open reduction internal fixation as the standard of care for most cases but also addresses nonoperative options for specific injury patterns or cases where surgical intervention is not feasible. Participants learn about the common complications following open fixation, including osteonecrosis, posttraumatic arthritis, and malunion. The course discusses the relationship between high-energy mechanisms and soft tissue injuries as well as the challenges of surgical wound healing.
Objectives:
Identify the pathophysiology of talar neck fractures.
Evaluate potential complications associated with talar neck fractures, including osteonecrosis, posttraumatic arthritis, and malunion, to inform ongoing patient care.
Select appropriate interventions based on the severity of soft tissue damage, bony comminution, and fracture displacement associated with talar neck fractures.
Communicate the importance of improving care among the interprofessional team to refine care delivery for patients with talar neck fractures.
Introduction
Talar neck fractures are relatively uncommon but potentially devastating injuries with often life-altering sequelae. The talus is located in the hindfoot and permits pain-free motion of the ankle, subtalar, and transverse tarsal joints. Talar neck fractures are associated with high-energy mechanisms, with severe soft tissue injury, bony comminution, and fracture displacement commonly co-occurring. Injury to the talar neck with resulting displacement can lead to permanent stiffness, deformity, and pain, with hindfoot arthrosis estimated to occur in greater than 90% of displaced talar neck fractures.[1]
The uncommon nature of these injuries partially explains the lack of high-quality literature to drive evidence-based treatment strategies. Open reduction internal fixation is the predominant treatment for displaced talar neck fractures, with nonoperative approaches reserved for the uncommon nondisplaced injury pattern or cases involving patients ineligible for surgery. Classic complications following open fixation of talar neck fractures include osteonecrosis or avascular necrosis, posttraumatic arthritis, and malunion.[2]
The high-energy traumatic mechanism is often a feature in these injuries, and fracture fragment displacement can disrupt the tenuous supply to the talus, resulting in necrosis. Unrecognized comminution of the medial talar neck predisposes these injuries to malreduction, leading to varus malunion deformity. Many of these injuries ultimately require hindfoot arthrodesis procedures for pain relief, regardless of the fixation timing and reduction quality. The high-energy mechanism of talar neck fractures also leads to significant soft tissue injury, making surgical wound healing a considerable concern.
Etiology
Anderson first reported a small case series of 18 talar neck fracture-dislocations in 1919. He coined the term “aviator astragalus” to describe this injury pattern.[3] Aviator astragalus referred to the increased incidence of talar neck fractures observed in fighter pilots during wartime following plane crashes. Typically, fractures of the talar neck occur with forced dorsiflexion of the ankle in the setting of a high-energy axial load.[1][4] Common injury mechanisms today include motor vehicle accidents or falls from height. The fracture occurs when the dense cortical bone of the anterior tibia is driven inferiorly and encounters the less dense trabecular bone of the talar neck.[4] Once the weak talar neck becomes disrupted, force propagates through the ligamentous structures surrounding the talus, including the talocalcaneal ligament and the complex subtalar and posterior ankle ligamentous complexes.[1] This action leads to subluxation or dislocation of the talar body from its articulations with the tibia superiorly and the calcaneus inferiorly. Hindfoot supination also influences the degree of displacement in talar neck fractures by exerting significant rotational forces. Hawkins reported a 26% rate of concomitant medial malleolus in a series of 27 talar neck fractures.[5]
Epidemiology
Fractures of the talus are the second most common injuries of all tarsal bone fractures, with talar neck fractures accounting for approximately 50% of all talus fractures.[1] Although the most common site of injury in the talus, talar neck fractures remain a rare injury pattern and classically reported a rate of less than 1% of all bony injuries of the foot and ankle.[4][6] However, an increase in survival rates for severe motor vehicle and motorcycle-related foot traumas may explain the current incidence rate, which is now closer to 2%, according to recent data.[27][6][7]
Pathophysiology
The junction between the head and body of the talus houses the talar neck, which is angled 10° to 44° medially and 5° to 50° plantar, respective to the talar body.[1] This junction contains less trabecular bone than the talar head or body.[7] The trabecular bone in the talar body orients in a direction that facilitates the transfer of weight-bearing force from the tibial plafond through the talar dome.[7] The trabecular bone of the talar neck is abruptly oriented in a different direction, predisposing this already weaker anatomic area to fracture.[4]
The talus receives blood through 3 major arteries: 47% from the posterior tibial artery, 36% from the anterior tibial artery, and 17% from the peroneal artery.[8] To comprehend why talar neck fractures pose a significant risk for avascular necrosis, it is essential to understand the vascular anatomy surrounding the talar neck. The artery of the tarsal canal, which is a branch of the posterior tibial artery, passes caudal to the talar neck between the middle and posterior talar facets. In addition, under the talar neck is a dense cluster of vascular nutrient foramina where the artery of the tarsal canal forms an anastomosis with the artery of the tarsal sinus, a branch of the anterior tibial artery.[9]
History and Physical
Patients with fractures of the talar neck typically present following a high-energy traumatic mechanism such as a motor vehicle accident or fall from height with hindfoot pain, ecchymosis, and swelling. Given that these patients are often victims of polytrauma with potential additional bony, vascular, or soft tissue injuries, prioritizing basic principles of acute trauma care, including airway, breathing, and circulation, is crucial. A complete neurovascular examination is necessary with the dorsalis pedis and posterior tibial artery pulses palpated or evaluated with ultrasonography. Examine the cutaneous sensory distribution of the following nerves: superficial peroneal, deep peroneal, saphenous, sural, and tibial nerve.
Conduct a motor examination, including great toe and ankle movements such as plantar and dorsiflexion, along with foot inversion and eversion, and document any observed neurovascular deficits. The skin should undergo close inspection for abrasion or laceration that suggests an open fracture. If a clinician finds an open fracture, they must perform thorough bedside irrigation and debridement and administer intravenous antibiotics and tetanus vaccination. Reduce dislocations and correct bony deformities, then apply a temporary splint to the extremity. This intervention helps alleviate pain and reduces pressure on the soft tissues surrounding the talus. If an extruded talus is present, the bone should be thoroughly washed with sterile saline and placed back inside the soft tissue envelope if possible.
Evaluation
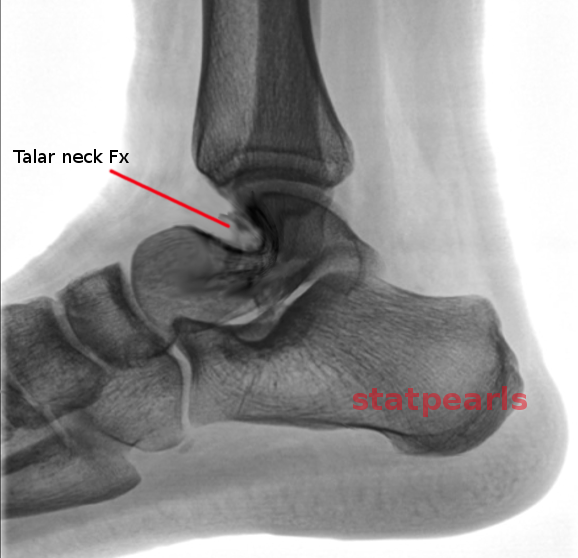
Evaluating a talar neck fracture should begin with plain radiographic imaging with an appropriate plain-film x-ray series of anteroposterior, lateral, and Canale views (see Image. Talar Neck Fracture). The Canale view provides the best visualization of the talar neck. This view is obtained by angling the x-ray beam 75° from the horizontal axis and positioning the foot in maximum equinus with varying degrees of eversion, usually of an angle around 15°.[6] Computed tomography (CT) scans have drastically improved the evaluation of talar neck fractures by allowing visualization of complex periarticular anatomy. CT is the best study to assess the degree of displacement, congruity of the articular surfaces, and comminution of these fracture patterns, with additional information gained in 93% of cases.[7] Three-dimensional (3D) reconstructions of CT imaging demonstrate sagittal or coronal alignment and facilitate surgical planning. Magnetic resonance imaging is limited in evaluating talar neck fractures in the acute setting.
In 1970, Dr. Leland Hawkins published a landmark paper describing a classification system for talar neck fractures.[5] This classification system is now known as the Hawkins Classification of Talar Neck Fractures. Initially, only types I to III were described, and it was not until 1978 that Canale and Kelly added type IV.[8] A literature review by Day et al, revealed Dr. Hawkins’ classic publication had 263 citations, and the revision by Canale and Kelly a further 206.[9] The Hawkins Classification is based on fracture displacement and the location of joint dislocation surrounding the talus.
- Hawkins I: nondisplaced fracture
- Hawkins II: fracture with an associated subtalar dislocation
- Hawkins III: fracture with associated subtalar and tibiotalar dislocation
- Hawkins IV: fracture with associated subtalar, tibiotalar, and talonavicular dislocations
The value of a classification system rests on its ability to predict outcomes or guide treatment. The Hawkins classification is predictive, with more severe injury such as Hawkins IV has the highest rate of osteonecrosis.[4]
- Hawkins I: 0% to 13% (avascular necrosis) AVN
- Hawkins II: 20% to 50% AVN
- Hawkins III: 20% to 100% AVN
- Hawkins IV: 70% to 100% AVN
Treatment / Management
Clinicians almost exclusively use open reduction and internal fixation to treat displaced talar neck fractures. Specialists reserve nonoperative treatment for rare nondisplaced injury patterns or cases involving patients ineligible for surgery. Nonoperative treatment includes immobilization with a splint in the acute setting and transitioning into a short leg cast when the swelling has subsided. A spanning external fixator is often selected as a temporizing measure to stabilize the bony injury and allow observation of the soft tissue envelope. The goal of surgery is anatomic reduction, which can be challenging in cases involving high displacement, comminution, or angulation. A biomechanical study demonstrated that as little as 2 mm of malreduction of the articular surface alters contact stresses.[10]
A dual-incision technique involving anteromedial and anterolateral approaches is commonly used to ensure accurate fracture reduction. An alternative sinus tarsi approach can be utilized as a lateral window, with a slightly more plantar incision from the distal fibula toward the 4th metatarsal. This approach provides an easier visualization of the lateral process. Exposures can be augmented with malleolar osteotomies to aid in visualizing the talar neck and body. Soft tissue considerations, fracture type, and other associated injuries often dictate the exact surgical approach. There are various reports of screw, plate, and hybrid fixation strategies. An estimated 96% of reported talar neck fractures were addressed with some combination of plate and screw constructs.[13] Longitudinal lag screws, especially on the medial side, are typically contraindicated because too much compression through medial comminution may result in a varus collapse or deformity. Published literature comparing screw constructs versus plate and screw constructs did not find one method superior to the other in terms of maintaining fixation and providing biomechanical stability.[11] Results from a study evaluated and compared screws alone versus screw and blade plate fixation, and the authors found no significant differences in yield point, stiffness, or load to create a 3 mm deformation.[12] This study utilized conventional 3.5 mm cortical or 4.0 mm cancellous screws. However, the authors suggest that headless variable-pitch screws would improve fixation strength compared to the conventional cannulated screws used in their investigation.
Historically, talar neck fractures were treated with the urgency reserved for open fractures or irreducible dislocations. The theory was that prompt reduction and fixation maintained the tenuous blood supply to the talus.[5][8][13] New literature has provided conflicting results.[14] The current understanding is that the risk for osteonecrosis is related to the degree of displacement at the time of injury.[14] An important distinction is that although delayed fixation is acceptable, delayed fracture reduction is not.
Differential Diagnosis
Differential diagnoses of talar neck fractures include talar body fractures, talar head fractures, rotational ankle fractures, ankle fracture-dislocations, simple ankle dislocations, calcaneal fractures such as the tongue and depression type, and subtalar joint simple or fracture-dislocations. These traumatic hindfoot pain and deformity etiologies can be differentiated using computed tomography imaging.
Prognosis
Given the associated high-energy mechanism and severe soft tissue injury often seen in talar neck fractures, the prognosis is poor. The frequently encountered concomitant injuries limit many talar neck fracture cases, as isolated talar neck fractures are unusual. The high association with other lower extremity and axial spine injuries may contribute to worse outcomes.[11][12] In a series of 70 talar neck fractures, Sanders et al, demonstrated that the incidence of foot and ankle reconstructive surgery following fixation increased over time.[13] The authors also reported an association with poor patient-reported outcomes and the development of postoperative complications.[13] Failure to recognize the displacement of fracture fragments and subsequent malreduction could also lead to poor outcomes.[14] Patients with talar neck fractures should receive counseling that residual hindfoot pain is frequent even after surgery, with 18.6% of patients requiring arthrodesis within 6 years.[15]
Complications
Extensive reports of high rates of complications following talar neck fractures exist in the literature.[5][8] Reported rates of osteonecrosis of the talus after talar neck fracture range from 11% to 100%.[11][16][17] Clinicians widely consider posttraumatic arthritis to be even more common than necrosis, affecting 30% to 90% of patients, according to reports.[17][18][19][20] Involvement of the subtalar joint accounts for 81% of cases of posttraumatic arthritis.[21][15] Postoperative infection is a concern given the high incidence of open fracture and soft tissue injury, with a reported deep infection rate of 21%.[15] Nonunion of talar neck fractures is relatively uncommon with rates under 5%, while malunion rates range from 20% to 37%.[15][22][23] Varus malunion is the most commonly reported deformity resulting from unappreciated or malreduced medial comminution.[20]
Postoperative and Rehabilitation Care
The postoperative and rehabilitation course after talar neck fractures differs depending on the type of fracture and whether or not surgery was required. Non-surgical management is indicated if the patient with a talar neck fracture has a strict contraindication to operative repair at this site. Moreover, genuinely nondisplaced talar neck fractures are exceptionally rare, prompting clinicians to conduct a computed tomography scan to assess the feasibility of non-operative treatment. Patients will need non-weight-bearing and immobilization if deemed appropriate for 6 to 8 weeks until the fracture healing is confirmed. However, most talar neck fractures are displaced and require surgery to reposition the bones to allow for healing. Recovery after surgery typically requires 6 to 12 weeks of non-weight-bearing and immobilization. Depending on patient risk factors, patients may be placed on anticoagulant therapy to decrease the risk of deep venous thrombosis or venous thromboembolism. Finally, after the period of non-weight-bearing ends, patients likely require a 6 to 8 week course of physical therapy.
Consultations
If the examiner identifies a talar neck fracture, consulting an orthopedic surgeon with a fellowship in trauma or foot and ankle is indicated. Prompt transportation to an orthopedic care facility is recommended for the patient if a clinician is unavailable.
Deterrence and Patient Education
Talar neck fractures account for about 50% of all fractures to the talus. These fractures are associated with a relatively high rate of avascular necrosis and posttraumatic arthritis due to the anatomical position of these fractures, technically challenging surgical approaches, and the complexity of the blood supply to the talar neck. Early recognition and management are critical in treating injuries that include hind foot pain, swelling, and ecchymosis. Recognition of these should prompt immediate presentation to an emergency department, especially in a mechanism consistent with an axial load applied across the ankle with forced dorsiflexion. Although rare, a nondisplaced talar neck fracture usually does not require surgical intervention and may be treated with immobilization for 6 to 8 weeks. However, most talar neck fractures are displaced and require surgical fixation. The inability to diagnose a displaced talar neck fracture can result in complications such as osteonecrosis, malunion, or nonunion. These complications have the potential to result in debilitating pain, loss of motion, and rigid deformity.
Pearls and Other Issues
The Hawkins sign is a helpful radiographic tool to assess the development of osteonecrosis following a talar neck fracture. This prognostic sign occurs as a lucency beneath the subchondral bone in the talar dome, typically observed approximately 6 to 8 weeks following injury.[21] Typically, the lucency is first visible in the medial aspect of the talus, followed by progression laterally. The presence of the subchondral lucency or Hawkins sign correlates with intact talar vascularity and rare progression to osteonecrosis.[4]
Enhancing Healthcare Team Outcomes
Talar neck fractures typically undergo management with dual-incision open reduction and internal fixation techniques. While recommending the prompt reduction of fracture dislocations, one can delay definitive fixation until the soft tissue envelope is amenable without an increased risk of osteonecrosis. In a series of 25 patients with 26 displaced talar neck fractures with a mean follow-up of 74 months, Lindvall et al observed a union rate of 88% and concluded that a delay in surgical fixation does not affect the outcome, such as osteonecrosis or union.[24]
Talar neck fractures require an interprofessional team that includes physicians, orthopedic and possibly neurological specialists, nurses with specialized orthopedic training, and, when necessary, pharmacists, all collaborating across disciplines to achieve optimal patient outcomes.