[1]
Phillippi JA. On vasa vasorum: A history of advances in understanding the vessels of vessels. Science advances. 2022 Apr 22:8(16):eabl6364. doi: 10.1126/sciadv.abl6364. Epub 2022 Apr 20
[PubMed PMID: 35442731]
Level 3 (low-level) evidence
[2]
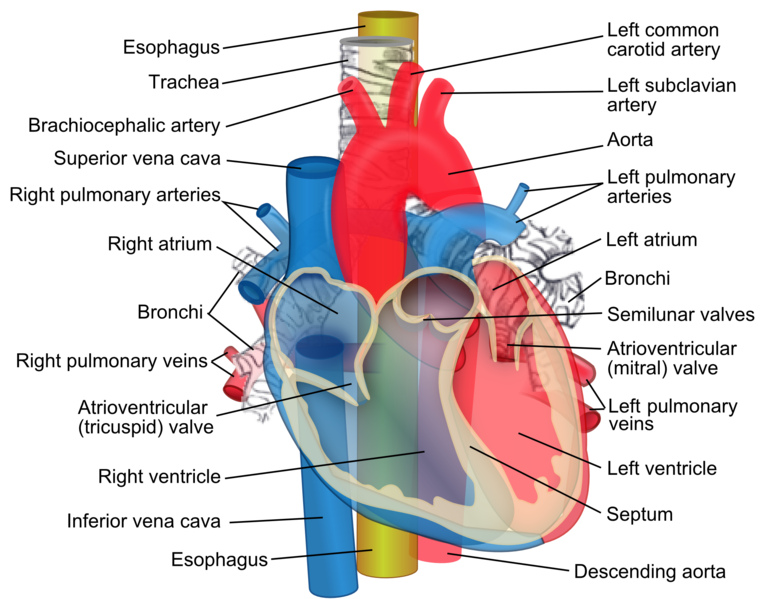
Sanjeev S, Karpawich PP. Superior vena cava and innominate vein dimensions in growing children : an aid for interventional devices and transvenous leads. Pediatric cardiology. 2006 Jul-Aug:27(4):414-9
[PubMed PMID: 16830087]
[3]
Badshah M, Soames R, Ibrahim M, Khan MJ, Khan A. Surface anatomy of major anatomical landmarks of the neck in an adult population: A Ct Evaluation of Vertebral Level. Clinical anatomy (New York, N.Y.). 2017 Sep:30(6):781-787. doi: 10.1002/ca.22907. Epub 2017 Jun 7
[PubMed PMID: 28514499]
[4]
Truong QA, Massaro JM, Rogers IS, Mahabadi AA, Kriegel MF, Fox CS, O'Donnell CJ, Hoffmann U. Reference values for normal pulmonary artery dimensions by noncontrast cardiac computed tomography: the Framingham Heart Study. Circulation. Cardiovascular imaging. 2012 Jan:5(1):147-54. doi: 10.1161/CIRCIMAGING.111.968610. Epub 2011 Dec 16
[PubMed PMID: 22178898]
[5]
Hassani C, Saremi F. Comprehensive Cross-sectional Imaging of the Pulmonary Veins. Radiographics : a review publication of the Radiological Society of North America, Inc. 2017 Nov-Dec:37(7):1928-1954. doi: 10.1148/rg.2017170050. Epub
[PubMed PMID: 29131765]
Level 2 (mid-level) evidence
[6]
Erbel R, Eggebrecht H. Aortic dimensions and the risk of dissection. Heart (British Cardiac Society). 2006 Jan:92(1):137-42
[PubMed PMID: 16365370]
[7]
Roman MJ, Devereux RB, Kramer-Fox R, O'Loughlin J. Two-dimensional echocardiographic aortic root dimensions in normal children and adults. The American journal of cardiology. 1989 Sep 1:64(8):507-12
[PubMed PMID: 2773795]
[8]
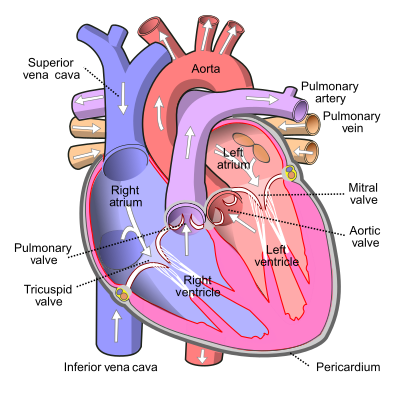
Vuillemin M, Pexieder T. Normal stages of cardiac organogenesis in the mouse: II. Development of the internal relief of the heart. The American journal of anatomy. 1989 Feb:184(2):114-28
[PubMed PMID: 2712003]
[9]
Dunham-Snary KJ, Wu D, Sykes EA, Thakrar A, Parlow LRG, Mewburn JD, Parlow JL, Archer SL. Hypoxic Pulmonary Vasoconstriction: From Molecular Mechanisms to Medicine. Chest. 2017 Jan:151(1):181-192. doi: 10.1016/j.chest.2016.09.001. Epub 2016 Sep 16
[PubMed PMID: 27645688]
[10]
Kirby ML, Gale TF, Stewart DE. Neural crest cells contribute to normal aorticopulmonary septation. Science (New York, N.Y.). 1983 Jun 3:220(4601):1059-61
[PubMed PMID: 6844926]
[11]
Phang K, Bowman M, Phillips A, Windsor J. Review of thoracic duct anatomical variations and clinical implications. Clinical anatomy (New York, N.Y.). 2014 May:27(4):637-44. doi: 10.1002/ca.22337. Epub 2013 Dec 2
[PubMed PMID: 24302465]
[12]
Duncan CP, Shim SS. J. Edouard Samson Address: the autonomic nerve supply of bone. An experimental study of the intraosseous adrenergic nervi vasorum in the rabbit. The Journal of bone and joint surgery. British volume. 1977 Aug:59(3):323-30
[PubMed PMID: 19482]
[13]
Lau EO, Lo CY, Yao Y, Mak AF, Jiang L, Huang Y, Yao X. Aortic Baroreceptors Display Higher Mechanosensitivity than Carotid Baroreceptors. Frontiers in physiology. 2016:7():384. doi: 10.3389/fphys.2016.00384. Epub 2016 Aug 31
[PubMed PMID: 27630578]
[14]
Pen D,Shanks J,Barrett C,Abukar Y,Paton JFR,Ramchandra R, Aortic Body Chemoreceptors Regulate Coronary Blood Flow in Conscious Control and Hypertensive Sheep. Hypertension (Dallas, Tex. : 1979). 2022 Jun
[PubMed PMID: 35382553]
[15]
Berlin DA, Bakker J. Understanding venous return. Intensive care medicine. 2014 Oct:40(10):1564-6. doi: 10.1007/s00134-014-3379-4. Epub 2014 Jun 26
[PubMed PMID: 24966066]
Level 3 (low-level) evidence
[16]
Wang J, Li J, Liu G, Deslauriers J. Nerves of the mediastinum. Thoracic surgery clinics. 2011 May:21(2):239-49, ix. doi: 10.1016/j.thorsurg.2011.01.006. Epub
[PubMed PMID: 21477774]
[17]
Fell SC. Surgical anatomy of the diaphragm and the phrenic nerve. Chest surgery clinics of North America. 1998 May:8(2):281-94
[PubMed PMID: 9619305]
[18]
Schumpelick V, Steinau G, Schlüper I, Prescher A. Surgical embryology and anatomy of the diaphragm with surgical applications. The Surgical clinics of North America. 2000 Feb:80(1):213-39, xi
[PubMed PMID: 10685150]
[19]
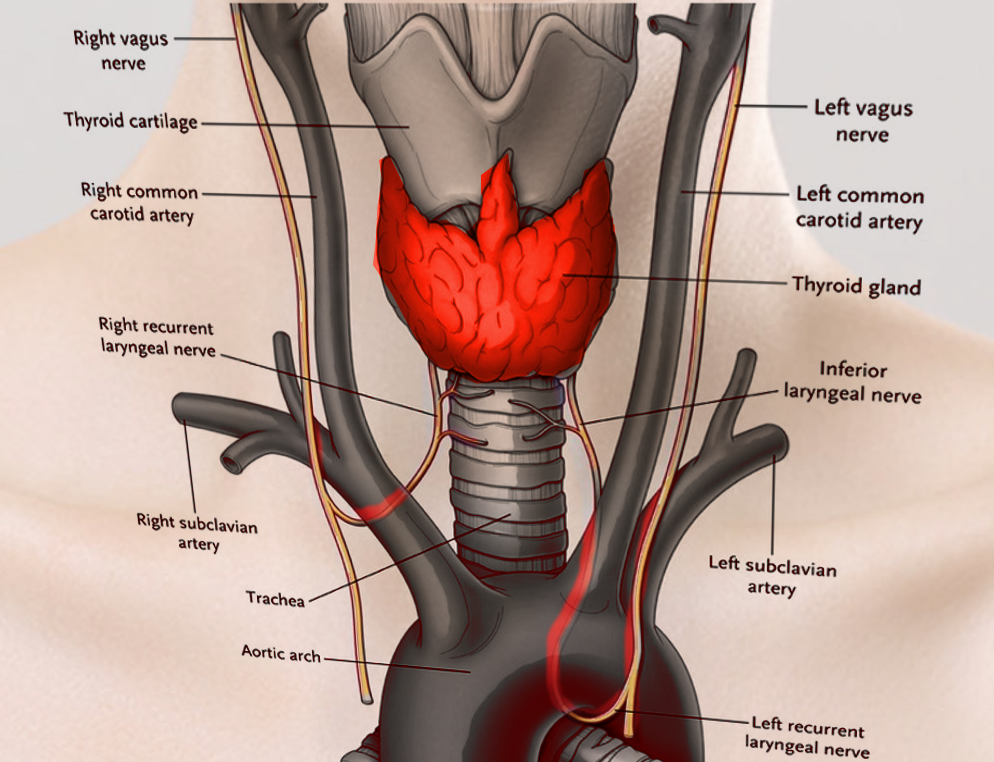
Myssiorek D. Recurrent laryngeal nerve paralysis: anatomy and etiology. Otolaryngologic clinics of North America. 2004 Feb:37(1):25-44, v
[PubMed PMID: 15062685]
[20]
Prifti E, Bonacchi M, Luisi SV, Vanini V. Coronary revascularization after arterial switch operation. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2002 Jan:21(1):111-3
[PubMed PMID: 11788276]
[21]
Roos-Hesselink JW, Meijboom FJ, Spitaels SE, van Domburg R, van Rijen EH, Utens EM, McGhie J, Bos E, Bogers AJ, Simoons ML. Decline in ventricular function and clinical condition after Mustard repair for transposition of the great arteries (a prospective study of 22-29 years). European heart journal. 2004 Jul:25(14):1264-70
[PubMed PMID: 15246646]
[23]
Villafañe J, Lantin-Hermoso MR, Bhatt AB, Tweddell JS, Geva T, Nathan M, Elliott MJ, Vetter VL, Paridon SM, Kochilas L, Jenkins KJ, Beekman RH 3rd, Wernovsky G, Towbin JA, American College of Cardiology’s Adult Congenital and Pediatric Cardiology Council. D-transposition of the great arteries: the current era of the arterial switch operation. Journal of the American College of Cardiology. 2014 Aug 5:64(5):498-511. doi: 10.1016/j.jacc.2014.06.1150. Epub
[PubMed PMID: 25082585]
[24]
Beauchesne LM, Warnes CA, Connolly HM, Ammash NM, Tajik AJ, Danielson GK. Outcome of the unoperated adult who presents with congenitally corrected transposition of the great arteries. Journal of the American College of Cardiology. 2002 Jul 17:40(2):285-90
[PubMed PMID: 12106933]
[25]
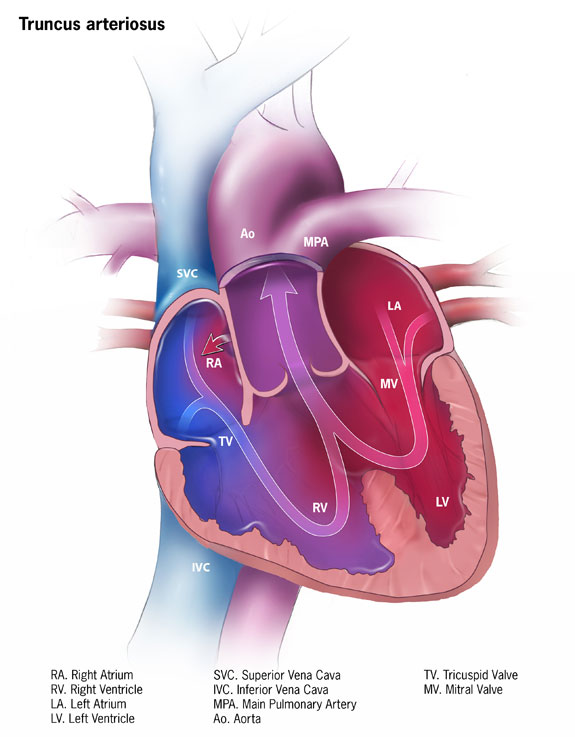
Alamri RM, Dohain AM, Arafat AA, Elmahrouk AF, Ghunaim AH, Elassal AA, Jamjoom AA, Al-Radi OO. Surgical repair for persistent truncus arteriosus in neonates and older children. Journal of cardiothoracic surgery. 2020 May 11:15(1):83. doi: 10.1186/s13019-020-01114-1. Epub 2020 May 11
[PubMed PMID: 32393289]
[26]
Yacoub MH, Hosny H, Afifi A, Nagy M, Mahgoub A, Simry W, AbouZeina MG, Doss R, El Sawy A, Shehata N, Elafifi A, Abdullah H, Romeih S. Novel concepts and early results of repairing common arterial trunk. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2022 Feb 18:61(3):562-571. doi: 10.1093/ejcts/ezab336. Epub
[PubMed PMID: 34347066]
[27]
Raisky O, Ali WB, Bajolle F, Marini D, Metton O, Bonnet D, Sidi D, Vouhé PR. Common arterial trunk repair: with conduit or without? European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2009 Oct:36(4):675-82. doi: 10.1016/j.ejcts.2009.03.062. Epub 2009 May 22
[PubMed PMID: 19464907]
[28]
Dice JE, Bhatia J. Patent ductus arteriosus: an overview. The journal of pediatric pharmacology and therapeutics : JPPT : the official journal of PPAG. 2007 Jul:12(3):138-46. doi: 10.5863/1551-6776-12.3.138. Epub
[PubMed PMID: 23055849]
Level 3 (low-level) evidence
[29]
Gillam-Krakauer M, Reese J. Diagnosis and Management of Patent Ductus Arteriosus. NeoReviews. 2018 Jul:19(7):e394-e402. doi: 10.1542/neo.19-7-e394. Epub
[PubMed PMID: 30505242]
[30]
Tort M, Ceviz M, Sevil F, Becit N. Surgical Treatment for Patent Ductus Arteriosus: Our Experience of 12 Years. Cureus. 2021 Apr 28:13(4):e14731. doi: 10.7759/cureus.14731. Epub 2021 Apr 28
[PubMed PMID: 34079678]
[31]
Fiore AC, Brown JW, Weber TR, Turrentine MW. Surgical treatment of pulmonary artery sling and tracheal stenosis. The Annals of thoracic surgery. 2005 Jan:79(1):38-46; discussion 38-46
[PubMed PMID: 15620911]
[32]
Santos N, Almeida T, Janeiro MC, Martins D. Pulmonary artery sling: a rare cause of stridor and respiratory distress. BMJ case reports. 2020 Feb 11:13(2):. doi: 10.1136/bcr-2019-233793. Epub 2020 Feb 11
[PubMed PMID: 32051151]
Level 3 (low-level) evidence
[33]
Oshima Y, Yamaguchi M, Yoshimura N, Sato S, Muraji T, Nishijima E, Tsugawa C. Management of pulmonary artery sling associated with tracheal stenosis. The Annals of thoracic surgery. 2008 Oct:86(4):1334-8. doi: 10.1016/j.athoracsur.2008.04.020. Epub
[PubMed PMID: 18805188]
[34]
Harold JG. Cardiology patient page. Screening for critical congenital heart disease in newborns. Circulation. 2014 Aug 26:130(9):e79-81. doi: 10.1161/CIRCULATIONAHA.113.008522. Epub
[PubMed PMID: 25156919]
[35]
Kishore S, Kumar M, Kumar A, Gupta A, Chandan C, Anshuman A, Prakash J, Sinha S, Kumar N. Clinical and Echocardiographic Profile of Congenital Heart Diseases in the 0-12-Year Age Group in a Tertiary Care Medical Institute in Eastern India: A Retrospective, Cross-Sectional Study. Cureus. 2022 Jun:14(6):e26114. doi: 10.7759/cureus.26114. Epub 2022 Jun 20
[PubMed PMID: 35747105]
Level 2 (mid-level) evidence
[36]
Plana MN, Zamora J, Suresh G, Fernandez-Pineda L, Thangaratinam S, Ewer AK. Pulse oximetry screening for critical congenital heart defects. The Cochrane database of systematic reviews. 2018 Mar 1:3(3):CD011912. doi: 10.1002/14651858.CD011912.pub2. Epub 2018 Mar 1
[PubMed PMID: 29494750]
Level 1 (high-level) evidence
[37]
Rüegger C, Bucher HU, Mieth RA. Pulse oximetry in the newborn: is the left hand pre- or post-ductal? BMC pediatrics. 2010 May 21:10():35. doi: 10.1186/1471-2431-10-35. Epub 2010 May 21
[PubMed PMID: 20492689]
[38]
Thangaratinam S, Brown K, Zamora J, Khan KS, Ewer AK. Pulse oximetry screening for critical congenital heart defects in asymptomatic newborn babies: a systematic review and meta-analysis. Lancet (London, England). 2012 Jun 30:379(9835):2459-2464. doi: 10.1016/S0140-6736(12)60107-X. Epub 2012 May 2
[PubMed PMID: 22554860]
Level 1 (high-level) evidence