Definition/Introduction
Most Americans prefer to die at home or in a home-like setting, yet over 30% die in acute care hospitals.[1] Seriously ill patients often state preferences for receiving adequate pain and symptom management, avoiding inappropriate prolongation of dying, achieving a sense of control, and strengthening their relationships with their loved ones.[2] Similarly, caregivers want their loved ones to receive care that is concordant with their wishes and comfort. Hospice helps to achieve these goals for terminally ill patients.[3][4] Hospice is a model of high-quality, compassionate care for people suffering from a life-limiting illness. It provides expert medical care, pain and symptom management, and emotional and spiritual support tailored to the patient’s needs and wishes. Hospice also provides emotional support to the patient’s loved ones even into bereavement. This chapter will review hospice care in the US, its structure and delivery, and its growth and barriers to utilization.
The hospice movement began with the work of Dame Cicely Saunders, whose predominant concern was alleviating the suffering of dying patients. In 1967, Saunders opened St. Christopher’s Hospice in South London and is now credited with developing the principles of hospice care that have become the core values reflected in hospice program policies worldwide.
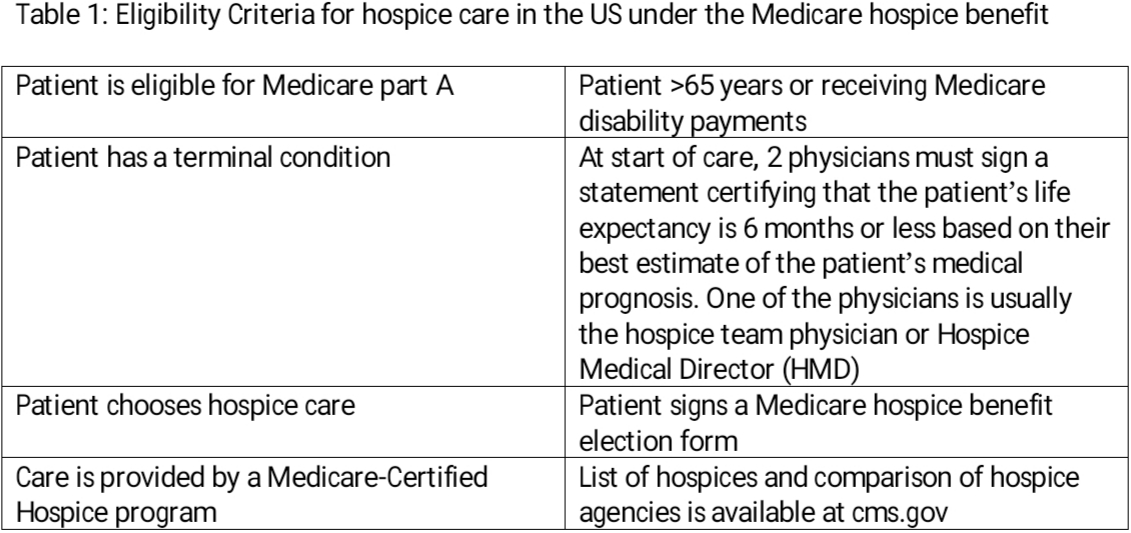
The first hospice program established in the US was Connecticut Hospice in 1974, spearheaded by Florence Wald, RN, who modeled it on St. Christopher’s Hospice. Both programs were in an inpatient setting.[5] US hospice programs follow a model that emphasizes care in the patient’s home and supports patients to die at home. Since 1983 hospice services have become available through Medicare, Medicaid, and almost all US insurance plans (see Table 1).
Table 1: Eligibility Criteria for hospice care in the US under the Medicare hospice benefit
Hospice Care in America
The most recent decade has seen significant growth in the number of hospice programs and hospice utilization. In 2016, there were 4382 Medicare-certified hospices in operation.
An estimated 1.4 million people received hospice care in the US, with almost half being older than 84 years and 27.2% (the largest portion) having cancer as their terminal diagnosis. Over 50% of patients were cared for at home, with 42% cared for in a nursing home setting. On closer examination, there is tremendous geographic variation in the availability and use of hospice services. For example, the proportion of Medicare decedents enrolled in hospice at the time of death varied across states from a low of 23% (Puerto Rico) to a high of 58% (Utah). Hospice utilization also varies by race and ethnicity. Almost 50% of Whites who died in 2016 used hospice care compared to 31% to 37% of African American, Asian, or Native American descent. While longer Lengths of Stay (LOS) in hospice have been shown to be more beneficial to patient and family,[6] family satisfaction with hospice care is more closely associated with the quality of hospice care, meaning fewer unmet needs and fewer reported concerns.[7] The median LOS in hospice in 2016 was 24 days, while the average was 71 days. There is also a notable racial disparity in the timing of referral to hospice, which impacts LOS. One study looking at a dataset of 43 869 home hospice enrollees found that African Americans are referred more frequently from a hospital location and have a greater chance of dying within seven days.[8]
Variations in hospice use can also have a basis on hospice and physician characteristics. One study found that 78 percent of hospices had at minimum one enrollment policy that might prove restrictive to access to care for patients with potentially high-cost medical care needs, such as chemotherapy or total parenteral nutrition. Smaller hospices, for-profit hospices, and hospices in some areas of the country consistently reported more limited enrollment policies.[9] This may be an important contributor to previously observed under-use of hospice by patients and families. Another contributor is physician characteristics. Patients cared for by physicians who frequently refer to hospice are more likely to be enrolled in hospice care earlier.[10]
To enable more timely referrals, educational interventions need to target physicians, and hospice programs need to expand patient access to potentially costlier palliative treatments that provide symptom relief. Ultimately, reform of the Medicare Hospice Benefit to include concurrent care or extend beyond a 6-month prognosis could also improve access to hospice in the United States.
Issues of Concern
The Medicare Hospice Benefit
Medicare was designed to provide comprehensive medical care for older Americans. Among its sections, Medicare Part A covers hospice services almost entirely—all services being provided without cost to the beneficiary, as long as the services are related to the terminal condition and have been approved by the hospice for payment. Given that this is a “carve-out” benefit, patients enrolled in hospice waive their traditional Medicare Parts A and D and elect the Medicare hospice benefit for care related to their terminal illness, including prescription medications. Historically, the Medicare hospice benefits only applied to medications related to the terminal diagnosis; for example, a hospice patient with congestive heart failure as their terminal diagnosis but with coexistent Diabetes and Hypertension would remain covered by traditional Medicare Parts A and D for the latter two comorbidities. Since 2015, under new guidance from Medicare, the hospice benefit now centers around a terminal prognosis rather than a diagnosis, given that prognosis is often worse in the setting of multiple comorbidities. For example, patients on hospice benefit from congestive heart failure who also suffer from chronic stage 4 kidney disease have a worse prognosis than patients with congestive heart failure but preserved kidney function.
Hospice Benefit Periods
All hospice services are rendered during benefit periods. Hospice care begins with two 90-day periods, followed by an unlimited number of 60-day periods. At the end of each benefit period and before the next one begins, the hospice team reevaluates the patient and recertifies that the patient has a terminal illness and that prognosis is less than 6 months. Each 60-day benefit period also requires a face-to-face visit from a hospice physician or nurse practitioner, who must provide clinical information to the certifying hospice physician in a timely manner. At any time during this process, a patient can change their mind about continuing hospice care.
Patients also may be discharged from hospice care for specific reasons, such as if they no longer have an expected prognosis of 6 months or if the patient moves away from the hospice’s service area. Patients are also free to re-enroll in the hospice benefit and need to be recertified for eligibility to resume hospice services. Whether patients revoke the hospice benefit or are discharged, traditional Medicare coverage becomes immediately available.
Since its inception, the Medicare hospice benefit has been a per diem capitated payment arrangement; hospices are paid a fixed dollar amount per day of patient care, based on the level of care. The rates of reimbursement are fixed annually and vary by geographic location.
Hospice Levels of Care
Four levels of care exist under the Medicare hospice benefit—two levels of care in the home and two inpatient levels. These are reimbursed differently by Medicare, with higher or more intense levels of care receiving higher reimbursement.
Routine Home Care
This level of care is administered in the patient’s place of residence, which could be a private home, a personal care home, a nursing facility, or a prison. In most states, the benefit does not cover the cost of a patient’s room and board in a nursing home. For a hospice program to obtain certification by Medicare, it is required to have 80% of its patients in their own homes. During home visits, the hospice team makes physical and environmental assessments and assesses the patient’s and family’s needs for additional services and assistance. Physical assessment involves reviewing the patient’s symptoms, the need for adjustment of medications, level of dependence, and psychological and spiritual distress. Environmental assessments focus on patient safety (e.g., gait and balance, loose carpets, or inadequate lighting) as well as adaptations required to adjust to the patient’s changing condition, such as having a hospital bed available for a patient who has become bedbound. Family assessment is crucial to detect caregiver burden and needs for additional support. When hospice care is rendered in the patient’s home, a family member serves as the primary caregiver and, when appropriate, helps make decisions for the terminally ill individual. Hospice staff, usually nurses, are on-call 24 hours a day, seven days a week.
Continuous Home Care
This level of hospice care, which is more intense than routine home care, is given during brief periods of crisis management of acute symptoms with the intention of maintaining the patient in their home setting. To justify continuous home care, the patient needs direct skilled care for 8 hours a day, over 50% of which has to be delivered by the nurse. An example of skilled care would be intractable pain management with frequent assessment and administration of intravenous medications. A nursing home cannot provide this level of care.
General Inpatient Care (GIP)
Provision of this level of care is outside of the patient’s usual home environment, in a Medicare-approved facility such as a free-standing inpatient hospice facility, a contracted nursing home, or hospital. This setting does not include custodial or residential. Indications that might determine a need for General Inpatient Care include managing uncontrolled pain, delirium, or other symptoms, especially ones that fall outside the purview of home care. Like continuous home care, a skilled need is necessary with GIP. Though GIP does not have a specified limit, patients are assessed daily by the hospice team regarding the necessity and eligibility of continuing that level of care. The expectation is for the patient to be stabilized and returned to their previous level of care/residence if possible.
Respite Care
This level is designed to provide relief to caregivers; it is allowable for no more than 5 consecutive days for every occurrence and is provided in a Medicare-approved facility such as an inpatient hospice facility or a nursing home. These patients don’t require skilled care.
Clinical Significance
Benefits of Hospice Care
Hospice care offers numerous benefits, including greater patient and family control of medical care, familiar surroundings for patients, decreased isolation of patients, and better access to loved ones. Hospice care does not require patients to accept their terminal prognosis or have a do-not-resuscitate (DNR) order. Instead, hospice works with each patient and family member to provide support and education to help them come to terms with approaching death. At the crux of hospice care is the interprofessional hospice team.
Hospice Interprofessional Team
The core hospice team is comprised of the hospice nurse, social worker, and chaplain. Medicare requires the core team members to be employed by the hospice agency. The core hospice team provides every level of hospice care, with the nurse being at the forefront of coordinating all the care the patient receives. The hospice medical director is also required to be a part of the interprofessional team (IDT). Together these comprise a hospice IDT, which develops an individualized plan of care for each patient-family unit. The plan of care is designed to meet the patient’s physical needs as well as the psychological, social, and even spiritual needs of the patient and family.
The interprofessional hospice team serves numerous roles. It manages the patient’s pain and other symptoms, assists the patient and family members with the psychosocial, emotional, and spiritual aspects of dying; it provides medications and medical equipment, instructs the family on how to care for the patient, and provides grief support and counseling both to the patient, surviving family, and friends after the patient’s death. Additionally, it makes short-term inpatient care available when pain or symptoms become unmanageable at home or when the caregiver needs respite time. When available, an IDT can provide specialized services like speech and physical therapy.
Role of the Physician
A physician can serve in one of three roles in hospice care; either the Hospice Medical Director (HMD), the attending physician, or the consultant physician. As the HMD, the physician assumes overall responsibility for the medical component of the care plans for all hospice patients, certifies and re-certifies a patient’s terminal illness, reviews, and updates a patient’s plan of care, participates in hospice’s quality improvement initiatives and educates members of the IDT on evidence-based symptom management and communication techniques.
The HMD also collaborates closely with the patient’s attending physician—the physician with the most significant role in determining and delivering the patient’s medical care. In most cases, the patient’s usual attending physician is a primary care physician but can also be a sub-specialist. The intent is for the attending physician to be the clinician who knows the patient best, likely from a previous provider-patient relationship. The patient/family must choose the hospice attending if they are able to identify one. The attending physician can then continue to serve in a similar collaborative capacity when the patient is admitted for hospice care.
A consultant physician must be contracted with the hospice and is typically a sub-specialist who provides a particular service related to a hospice patient’s terminal condition (e.g., a single fraction palliative radiation treatment for a painful metastatic lesion administered by a consulting radiation oncologist). The Hospice can bill Medicare part A for these services and any medically indicated services provided by the HMD. These physician charges get reimbursed in addition to the per diem hospice rates paid by Medicare. The hospice per diem rate includes all of the administrative responsibilities of the Hospice Medical Director. The hospice attending physician typically bills Medicare directly for their services under Part B, using a hospice modifier to indicate if service was 'related' or 'unrelated' to the terminal hospice diagnosis.
Nursing, Allied Health, and Interprofessional Team Interventions
Hospice end-of-life care requires an interprofessional team that includes clinicians (e.g., family doctors, specialists as outlined above), specialty trained nursing staff, home and inpatient health aids, psychological and mental health professionals, pharmacists, and, if necessary, clergy. All these specialties and disciplines must coordinate their activities, utilize open communication, work with the patient's family and friends, and exercise the utmost compassion during this sensitive time. While no actions can change the final outcome, an interprofessional team can make the experience much less traumatic and more comfortable for patients and their families. [Level 5]