[1]
Brouillard P, Boon LM, Mulliken JB, Enjolras O, Ghassibé M, Warman ML, Tan OT, Olsen BR, Vikkula M. Mutations in a novel factor, glomulin, are responsible for glomuvenous malformations ("glomangiomas"). American journal of human genetics. 2002 Apr:70(4):866-74
[PubMed PMID: 11845407]
[2]
Abbas A, Braswell M, Bernieh A, Brodell RT. Glomuvenous malformations in a young man. Dermatology online journal. 2018 Oct 15:24(10):. pii: 13030/qt2w54142d. Epub 2018 Oct 15
[PubMed PMID: 30677819]
[3]
Arens C, Dreyer T, Eistert B, Glanz H. Glomangioma of the nasal cavity. Case report and literature review. ORL; journal for oto-rhino-laryngology and its related specialties. 1997 May-Jun:59(3):179-81
[PubMed PMID: 9186975]
Level 3 (low-level) evidence
[4]
Chatterjee JS, Youssef AH, Brown RM, Nishikawa H. Congenital nodular multiple glomangioma: a case report. Journal of clinical pathology. 2005 Jan:58(1):102-3
[PubMed PMID: 15623496]
Level 3 (low-level) evidence
[5]
Munoz C, Bobadilla F, Fuenzalida H, Goldner R, Sina B. Congenital glomangioma of the breast: type 2 segmental manifestation. International journal of dermatology. 2011 Mar:50(3):346-9. doi: 10.1111/j.1365-4632.2010.04565.x. Epub
[PubMed PMID: 21342169]
[6]
Tewattanarat N, Srinakarin J, Wongwiwatchai J, Areemit S, Komvilaisak P, Ungarreevittaya P, Intarawichian P. Imaging of a glomus tumor of the liver in a child. Radiology case reports. 2020 Apr:15(4):311-315. doi: 10.1016/j.radcr.2019.12.014. Epub 2020 Jan 20
[PubMed PMID: 31988680]
Level 3 (low-level) evidence
[7]
Leger M, Patel U, Mandal R, Walters R, Cook K, Haimovic A, Franks AG Jr. Glomangioma. Dermatology online journal. 2010 Nov 15:16(11):11
[PubMed PMID: 21163162]
[8]
Souza NGA, Nai GA, Wedy GF, Abreu MAMM. Congenital plaque-like glomangioma: report of two cases. Anais brasileiros de dermatologia. 2017:92(5 Suppl 1):43-46. doi: 10.1590/abd1806-4841.20175766. Epub
[PubMed PMID: 29267443]
Level 3 (low-level) evidence
[9]
Cabral CR, Oliveira Filho Jd, Matsumoto JL, Cignachi S, Tebet AC, Nasser Kda R. Type 2 segmental glomangioma--Case report. Anais brasileiros de dermatologia. 2015 May-Jun:90(3 Suppl 1):97-100. doi: 10.1590/abd1806-4841.20152483. Epub
[PubMed PMID: 26312686]
Level 3 (low-level) evidence
[10]
Jha A, Khunger N, Malarvizhi K, Ramesh V, Singh A. Familial Disseminated Cutaneous Glomuvenous Malformation: Treatment with Polidocanol Sclerotherapy. Journal of cutaneous and aesthetic surgery. 2016 Oct-Dec:9(4):266-269. doi: 10.4103/0974-2077.197083. Epub
[PubMed PMID: 28163461]
[11]
Suárez-Magdalena O, Monteagudo B, Figueroa O, Gómez-Pérez MI. Glomulin gene c.157_161del mutation in a family with multiple glomuvenous malformations. International journal of dermatology. 2019 Feb:58(2):e43-e45. doi: 10.1111/ijd.14312. Epub 2018 Nov 21
[PubMed PMID: 30460983]
[12]
Boon LM, Mulliken JB, Enjolras O, Vikkula M. Glomuvenous malformation (glomangioma) and venous malformation: distinct clinicopathologic and genetic entities. Archives of dermatology. 2004 Aug:140(8):971-6
[PubMed PMID: 15313813]
[13]
Gonçalves R, Lopes A, Júlio C, Durão C, de Mello RA. Knee glomangioma: a rare location for a glomus tumor. Rare tumors. 2014 Oct 27:6(4):5588. doi: 10.4081/rt.2014.5588. Epub 2014 Dec 18
[PubMed PMID: 25568752]
[14]
Tony G, Hauxwell S, Nair N, Harrison DA, Richards PJ. Large plaque-like glomangioma in a patient with multiple glomus tumours: review of imaging and histology. Clinical and experimental dermatology. 2013 Oct:38(7):693-700. doi: 10.1111/ced.12122. Epub
[PubMed PMID: 24073652]
[15]
Boon LM, Brouillard P, Irrthum A, Karttunen L, Warman ML, Rudolph R, Mulliken JB, Olsen BR, Vikkula M. A gene for inherited cutaneous venous anomalies ("glomangiomas") localizes to chromosome 1p21-22. American journal of human genetics. 1999 Jul:65(1):125-33
[PubMed PMID: 10364524]
[17]
Goujon E, Cordoro KM, Barat M, Rousseau T, Brouillard P, Vikkula M, Frieden IJ, Vabres P. Congenital plaque-type glomuvenous malformations associated with fetal pleural effusion and ascites. Pediatric dermatology. 2011 Sep-Oct:28(5):528-31. doi: 10.1111/j.1525-1470.2010.01216.x. Epub 2010 Dec 7
[PubMed PMID: 21133993]
[18]
Scheithauer BW, Rodriguez FJ, Spinner RJ, Dyck PJ, Salem A, Edelman FL, Amrami KK, Fu YS. Glomus tumor and glomangioma of the nerve. Report of two cases. Journal of neurosurgery. 2008 Feb:108(2):348-56. doi: 10.3171/JNS/2008/108/2/0348. Epub
[PubMed PMID: 18240933]
Level 3 (low-level) evidence
[19]
Parker KL, Zervos MD, Donington JS, Shukla PS, Bizekis CS. Tracheal glomangioma in a patient with asthma and chest pain. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010 Jan 10:28(2):e9-e10. doi: 10.1200/JCO.2009.22.7942. Epub 2009 Oct 26
[PubMed PMID: 19858390]
[20]
Larsen DK, Madsen PV. [Glomus tumour of the distal phalanx]. Ugeskrift for laeger. 2018 Jul 23:180(30):. pii: V10170807. Epub
[PubMed PMID: 30037386]
[21]
Aneiros-Fernandez J, Retamero JA, Husein-ElAhmed H, Carriel V, Ruiz Villaverde R, O'Valle F, Aneiros-Cachaza J. Smoothelin and WT-1 expression in glomus tumors and glomuvenous malformations. Histology and histopathology. 2017 Feb:32(2):153-160. doi: 10.14670/HH-11-782. Epub 2016 May 17
[PubMed PMID: 27184662]
[22]
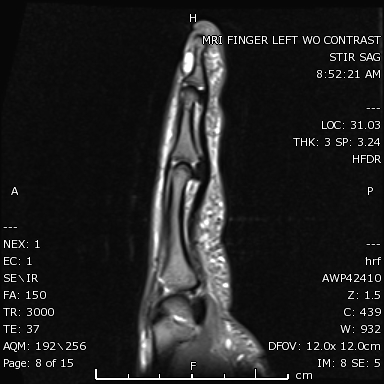
Flors L, Norton PT, Hagspiel KD. Glomuvenous malformation: magnetic resonance imaging findings. Pediatric radiology. 2015 Feb:45(2):286-90. doi: 10.1007/s00247-014-3086-x. Epub 2014 Jul 5
[PubMed PMID: 24996811]
[23]
Chirila M, Rogojan L. Glomangioma of the nasal septum: a case report and review. Ear, nose, & throat journal. 2013 Apr-May:92(4-5):E7-9
[PubMed PMID: 23599117]
Level 3 (low-level) evidence
[24]
Sharma JK, Miller R. Treatment of multiple glomangioma with tuneable dye laser. Journal of cutaneous medicine and surgery. 1999 Jan:3(3):167-8
[PubMed PMID: 10082598]
[25]
Rivers JK, Rivers CA, Li MK, Martinka M. Laser Therapy for an Acquired Glomuvenous Malformation (Glomus Tumour): A Nonsurgical Approach. Journal of cutaneous medicine and surgery. 2016 Jan:20(1):80-3. doi: 10.1177/1203475415596121. Epub 2015 Jul 15
[PubMed PMID: 26177926]
[26]
Phillips CB, Guerrero C, Theos A. Nd:YAG laser offers promising treatment option for familial glomuvenous malformation. Dermatology online journal. 2015 Apr 16:21(4):. pii: 13030/qt4nv6k7bv. Epub 2015 Apr 16
[PubMed PMID: 25933083]
[27]
Jha A, Ramesh V, Singh A. Disseminated cutaneous glomuvenous malformation. Indian journal of dermatology, venereology and leprology. 2014 Nov-Dec:80(6):556-8. doi: 10.4103/0378-6323.144200. Epub
[PubMed PMID: 25382523]
[28]
Babeau F, Knafo S, Rigau V, Lonjon N. Paravertebral glomangioma mimicking a schwannoma. Neuro-Chirurgie. 2013 Aug-Oct:59(4-5):187-90
[PubMed PMID: 24367799]
[29]
Jiga LP, Rata A, Ignatiadis I, Geishauser M, Ionac M. Atypical venous glomangioma causing chronic compression of the radial sensory nerve in the forearm. A case report and review of the literature. Microsurgery. 2012 Mar:32(3):231-4. doi: 10.1002/micr.20983. Epub 2012 Mar 8
[PubMed PMID: 22407591]
Level 3 (low-level) evidence
[30]
Arica DA, Arica IE, Yayli S, Cobanoglu U, Akay BN, Anadolu R, Bahadir S. Spitz nevus arising upon a congenital glomuvenous malformation. Pediatric dermatology. 2013 May-Jun:30(3):e25-6. doi: 10.1111/j.1525-1470.2011.01713.x. Epub 2012 Feb 3
[PubMed PMID: 22304367]