[1]
Kaur C, Foulds WS, Ling EA. Hypoxia-ischemia and retinal ganglion cell damage. Clinical ophthalmology (Auckland, N.Z.). 2008 Dec:2(4):879-89
[PubMed PMID: 19668442]
[2]
Kergoat H, Hérard ME, Lemay M. RGC sensitivity to mild systemic hypoxia. Investigative ophthalmology & visual science. 2006 Dec:47(12):5423-7
[PubMed PMID: 17122132]
[3]
Harris AL. Hypoxia--a key regulatory factor in tumour growth. Nature reviews. Cancer. 2002 Jan:2(1):38-47
[PubMed PMID: 11902584]
[4]
Kitagawa K,Matsumoto M,Tagaya M,Hata R,Ueda H,Niinobe M,Handa N,Fukunaga R,Kimura K,Mikoshiba K, 'Ischemic tolerance' phenomenon found in the brain. Brain research. 1990 Sep 24
[PubMed PMID: 2245337]
[5]
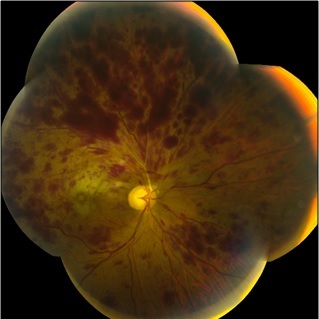
Karia N. Retinal vein occlusion: pathophysiology and treatment options. Clinical ophthalmology (Auckland, N.Z.). 2010 Jul 30:4():809-16
[PubMed PMID: 20689798]
[6]
Shahid H, Hossain P, Amoaku WM. The management of retinal vein occlusion: is interventional ophthalmology the way forward? The British journal of ophthalmology. 2006 May:90(5):627-39
[PubMed PMID: 16622095]
[7]
Cugati S, Wang JJ, Rochtchina E, Mitchell P. Ten-year incidence of retinal vein occlusion in an older population: the Blue Mountains Eye Study. Archives of ophthalmology (Chicago, Ill. : 1960). 2006 May:124(5):726-32
[PubMed PMID: 16682596]
[8]
Scott IU, Ip MS, VanVeldhuisen PC, Oden NL, Blodi BA, Fisher M, Chan CK, Gonzalez VH, Singerman LJ, Tolentino M, SCORE Study Research Group. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular Edema secondary to branch retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 6. Archives of ophthalmology (Chicago, Ill. : 1960). 2009 Sep:127(9):1115-28. doi: 10.1001/archophthalmol.2009.233. Epub
[PubMed PMID: 19752420]
Level 1 (high-level) evidence
[9]
Rogers S, McIntosh RL, Cheung N, Lim L, Wang JJ, Mitchell P, Kowalski JW, Nguyen H, Wong TY, International Eye Disease Consortium. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology. 2010 Feb:117(2):313-9.e1. doi: 10.1016/j.ophtha.2009.07.017. Epub
[PubMed PMID: 20022117]
[10]
. Argon laser scatter photocoagulation for prevention of neovascularization and vitreous hemorrhage in branch vein occlusion. A randomized clinical trial. Branch Vein Occlusion Study Group. Archives of ophthalmology (Chicago, Ill. : 1960). 1986 Jan:104(1):34-41
[PubMed PMID: 2417579]
Level 1 (high-level) evidence
[11]
Funk M,Kriechbaum K,Prager F,Benesch T,Georgopoulos M,Zlabinger GJ,Schmidt-Erfurth U, Intraocular concentrations of growth factors and cytokines in retinal vein occlusion and the effect of therapy with bevacizumab. Investigative ophthalmology
[PubMed PMID: 19060280]
[12]
Park KS, Kim JW, An JH, Woo JM. Elevated plasma pentraxin 3 and its association with retinal vein occlusion. Korean journal of ophthalmology : KJO. 2014 Dec:28(6):460-5. doi: 10.3341/kjo.2014.28.6.460. Epub 2014 Nov 19
[PubMed PMID: 25435748]
[13]
Pe'er J, Folberg R, Itin A, Gnessin H, Hemo I, Keshet E. Vascular endothelial growth factor upregulation in human central retinal vein occlusion. Ophthalmology. 1998 Mar:105(3):412-6
[PubMed PMID: 9499769]
[14]
Noma H, Funatsu H, Yamasaki M, Tsukamoto H, Mimura T, Sone T, Jian K, Sakamoto I, Nakano K, Yamashita H, Minamoto A, Mishima HK. Pathogenesis of macular edema with branch retinal vein occlusion and intraocular levels of vascular endothelial growth factor and interleukin-6. American journal of ophthalmology. 2005 Aug:140(2):256-61
[PubMed PMID: 16086947]
[15]
Noma H,Funatsu H,Yamasaki M,Tsukamoto H,Mimura T,Sone T,Hirayama T,Tamura H,Yamashita H,Minamoto A,Mishima HK, Aqueous humour levels of cytokines are correlated to vitreous levels and severity of macular oedema in branch retinal vein occlusion. Eye (London, England). 2008 Jan
[PubMed PMID: 16826241]
[16]
Brown DM, Campochiaro PA, Bhisitkul RB, Ho AC, Gray S, Saroj N, Adamis AP, Rubio RG, Murahashi WY. Sustained benefits from ranibizumab for macular edema following branch retinal vein occlusion: 12-month outcomes of a phase III study. Ophthalmology. 2011 Aug:118(8):1594-602. doi: 10.1016/j.ophtha.2011.02.022. Epub
[PubMed PMID: 21684606]
[17]
Qian T, Zhao M, Xu X. Comparison between anti-VEGF therapy and corticosteroid or laser therapy for macular oedema secondary to retinal vein occlusion: A meta-analysis. Journal of clinical pharmacy and therapeutics. 2017 Oct:42(5):519-529. doi: 10.1111/jcpt.12551. Epub 2017 Jun 22
[PubMed PMID: 28639290]
Level 2 (mid-level) evidence
[18]
Haller JA, Bandello F, Belfort R Jr, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jacques ML, Jiao J, Li XY, Whitcup SM, OZURDEX GENEVA Study Group. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010 Jun:117(6):1134-1146.e3. doi: 10.1016/j.ophtha.2010.03.032. Epub 2010 Apr 24
[PubMed PMID: 20417567]
Level 1 (high-level) evidence
[20]
. Argon laser photocoagulation for macular edema in branch vein occlusion. The Branch Vein Occlusion Study Group. American journal of ophthalmology. 1984 Sep 15:98(3):271-82
[PubMed PMID: 6383055]
[21]
Patz A. Argon laser photocoagulation for macular edema in branch vein occlusion. American journal of ophthalmology. 1984 Sep 15:98(3):374-5
[PubMed PMID: 6540993]
[22]
Brar M, Grewal DS, Sharma M, Grewal SPS. Rapid regression of retinal neovascularization following intravitreal bevacizumab in branch retinal vein occlusion imaged by optical coherence tomography angiography. Indian journal of ophthalmology. 2018 Apr:66(4):572. doi: 10.4103/ijo.IJO_868_17. Epub
[PubMed PMID: 29582824]
[23]
Mastropasqua R,Di Antonio L,Di Staso S,Agnifili L,Di Gregorio A,Ciancaglini M,Mastropasqua L, Optical Coherence Tomography Angiography in Retinal Vascular Diseases and Choroidal Neovascularization. Journal of ophthalmology. 2015
[PubMed PMID: 26491548]