[1]
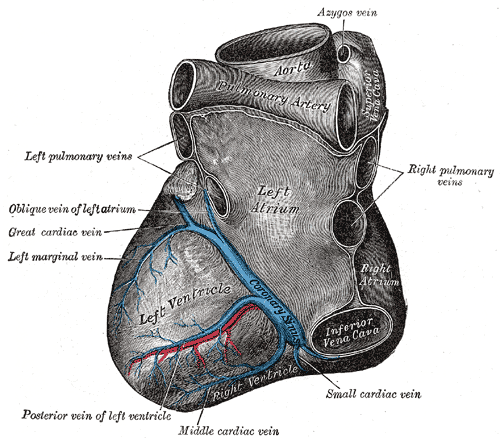
Loukas M, Bilinsky S, Bilinsky E, el-Sedfy A, Anderson RH. Cardiac veins: a review of the literature. Clinical anatomy (New York, N.Y.). 2009 Jan:22(1):129-45. doi: 10.1002/ca.20745. Epub
[PubMed PMID: 19097063]
[2]
Ortale JR, Gabriel EA, Iost C, Márquez CQ. The anatomy of the coronary sinus and its tributaries. Surgical and radiologic anatomy : SRA. 2001:23(1):15-21
[PubMed PMID: 11370136]
[3]
Mazur M, Kuniewicz M, Klimek-Piotrowska W, Kucharska A, Mizia E, Mróz I, Wandzel-Loch B. Human coronary sinus - from Galen to modern times. Folia medica Cracoviensia. 2015:55(1):5-15
[PubMed PMID: 26774627]
[4]
Goodwill AG, Dick GM, Kiel AM, Tune JD. Regulation of Coronary Blood Flow. Comprehensive Physiology. 2017 Mar 16:7(2):321-382. doi: 10.1002/cphy.c160016. Epub 2017 Mar 16
[PubMed PMID: 28333376]
[5]
von Lüdinghausen M. The venous drainage of the human myocardium. Advances in anatomy, embryology, and cell biology. 2003:168():I-VIII, 1-104
[PubMed PMID: 12645157]
Level 3 (low-level) evidence
[7]
Kapa S, DeSimone CV, Asirvatham SJ. Innervation of the heart: An invisible grid within a black box. Trends in cardiovascular medicine. 2016 Apr:26(3):245-57. doi: 10.1016/j.tcm.2015.07.001. Epub 2015 Jul 9
[PubMed PMID: 26254961]
[8]
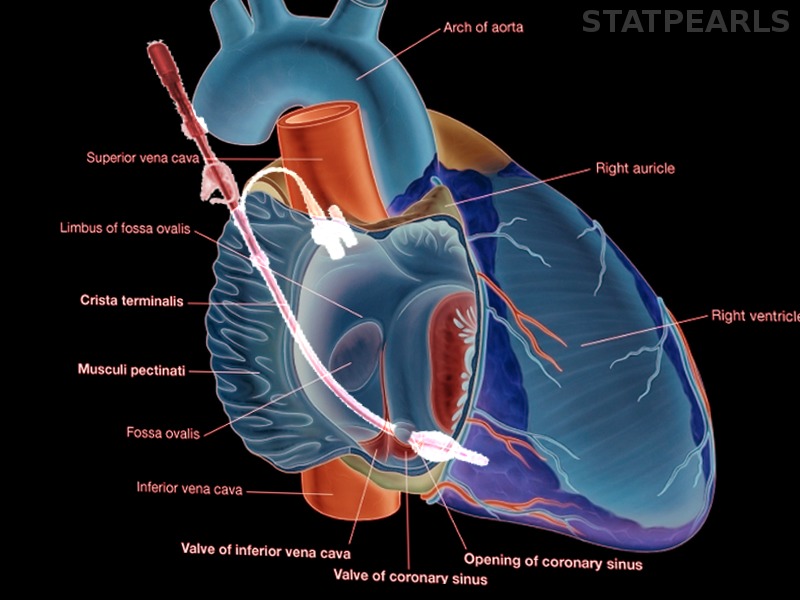
Antz M, Otomo K, Arruda M, Scherlag BJ, Pitha J, Tondo C, Lazzara R, Jackman WM. Electrical conduction between the right atrium and the left atrium via the musculature of the coronary sinus. Circulation. 1998 Oct 27:98(17):1790-5
[PubMed PMID: 9788835]
[9]
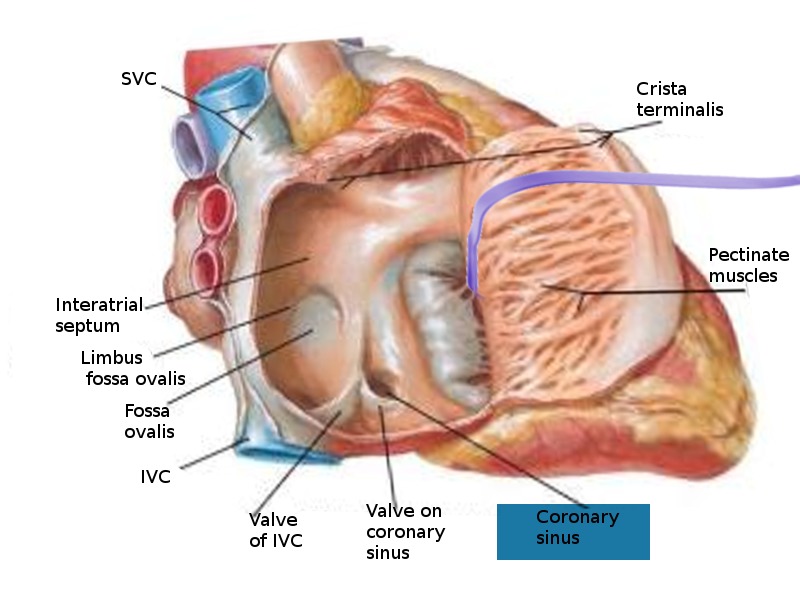
Karaca M, Bilge O, Dinckal MH, Ucerler H. The anatomic barriers in the coronary sinus: implications for clinical procedures. Journal of interventional cardiac electrophysiology : an international journal of arrhythmias and pacing. 2005 Nov:14(2):89-94
[PubMed PMID: 16374555]
[10]
Corcoran SJ, Lawrence C, McGuire MA. The valve of Vieussens: an important cause of difficulty in advancing catheters into the cardiac veins. Journal of cardiovascular electrophysiology. 1999 Jun:10(6):804-8
[PubMed PMID: 10376917]
[11]
Pahwa R, Kumar A. Persistent left superior vena cava: an intensivist's experience and review of the literature. Southern medical journal. 2003 May:96(5):528-9
[PubMed PMID: 12911199]
[12]
Gundry SR, Kirsh MM. A comparison of retrograde cardioplegia versus antegrade cardioplegia in the presence of coronary artery obstruction. The Annals of thoracic surgery. 1984 Aug:38(2):124-7
[PubMed PMID: 6465990]
[13]
Medical Advisory Secretariat. Biventricular pacing (cardiac resynchronization therapy): an evidence-based analysis. Ontario health technology assessment series. 2005:5(13):1-60
[PubMed PMID: 23074464]
[14]
Chen YA, Nguyen ET, Dennie C, Wald RM, Crean AM, Yoo SJ, Jimenez-Juan L. Computed tomography and magnetic resonance imaging of the coronary sinus: anatomic variants and congenital anomalies. Insights into imaging. 2014 Oct:5(5):547-57. doi: 10.1007/s13244-014-0330-8. Epub 2014 Jul 22
[PubMed PMID: 25048808]
[15]
Habib A, Lachman N, Christensen KN, Asirvatham SJ. The anatomy of the coronary sinus venous system for the cardiac electrophysiologist. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2009 Nov:11 Suppl 5():v15-21. doi: 10.1093/europace/eup270. Epub
[PubMed PMID: 19861386]