Continuing Education Activity
Epiretinal membrane is a commonly occurring condition affecting the posterior pole of the retina over the macula. It appears as a greyish semi-translucent avascular membrane over the internal limiting membrane (ILM) on the surface of the retina. Etiology is unknown and can be seen as an idiopathic (IERM) condition or secondary to trauma, post intraocular surgery, chronic ocular diseases, etc. It progressively affects the central vision and causes metamorphopsia. This activity reviews the evaluation and treatment of the epiretinal membrane and highlights the role of the interprofessional team in evaluating and treating patients with this condition.
Objectives:
- Identify the etiology of the epiretinal membrane.
- Describe the appropriate evaluation of the epiretinal membrane.
- List the management options available for the epiretinal membrane.
- Explain interprofessional team strategies for improving care coordination and improve outcomes in the management of the epiretinal membrane.
Introduction
In 1865, Iwanoff described an epiretinal membrane (ERM) as the proliferation of cellular tissue on the surface of the retina along the inner limiting membrane. Its a commonly occurring condition, affecting the posterior pole of the retina over the macula. It appears as a greyish semi-translucent avascular membrane over the internal limiting membrane (ILM) on the surface of the retina. The other synonyms for ERM are macular pucker, preretinal macular fibrosis, surface wrinkling retinopathy, epimacular proliferations, epiretinal fibrosis or gliosis, and cellophane maculopathy.
Etiology is unknown and can be seen as an idiopathic (IERM) condition or secondary to trauma, post intraocular surgery, chronic ocular diseases, etc. It progressively affects the central vision and causes metamorphopsia. Optical coherence tomography (OCT) is the diagnostic procedure of choice for diagnosing and assessing the extent of the epiretinal membrane and its impact on the retinal morphology. Treatment, when indicated, is pars-plana vitrectomy (PPV) with ERM and ILM peeling.
Etiology
Etiology is unknown, and the most common cause of the epiretinal membrane (ERM) is idiopathic (IERM). Secondary epiretinal membranes are seen in trauma, intraocular surgery, post-macular lasers, diabetic retinopathy, retinal vein occlusion, chronic macular edema, chronic intraocular inflammation, retinal detachment, and intraocular tumors. Increasing age, ERM in the other eye, and posterior vitreous detachment (PVD) are other risk factors. Several other names for ERM include cellophane maculopathy, macular pucker, preretinal fibrosis, and preretinal membrane. A systemic review involving 49,000 subjects found that greater age and female gender are significant risk factors for ERM.[1]
Epidemiology
The most common type of epiretinal membranes is idiopathic and is common in patients over the age of 50. Approximately 20% of patients over the age of 75 have an epiretinal membrane with both sexes equally affected. Some reports show a slightly higher incidence in females.
In a multi-ethnic study of the United States population done in 2011 involving 5960 participants aged 45 to 84 years, it was shown that Chinese(39%) show significantly higher prevalence compared to Hispanics (29.3%), Whites (27.5%) and Blacks (26.2%).[2] Increasing age, diabetes, and hypercholesteremia were found to be risk factors for the epiretinal membrane.
In a multicentric meta-analysis of population-based studies involving 40,000 participants, it was shown that 9% had some form of ERM. Epiretinal membranes are classified into two groups: one with retinal folds called preretinal macular fibrosis (PMF) and second without retinal folds called cellophane macula reflex (CMR). Of the ERM patients, 6.5% had CMR, and 2.6% had an advanced form of PMF. Older and female participants showed a higher risk.[1]
The Blue Mountains study was done over five years to study the incidence and progression of epiretinal membranes in the older Australian population.[3] Three thousand six hundred fifty-four persons, 49 years or older, living in the Blue Mountains area, west of Sydney, Australia, participated in the study from 1992 to 1994. The mean age was 65 years. The incidence of ERM’s in the first eye was 5.3%, and the progression of early ERM to an advanced stage of ERM of 9.3%. Five-year cumulative incidence rates of PMF and CMR were 1.5% and 3.8 %, respectively. Of these, 13.9% developed ERM in their second eye after five years.
Pathophysiology
A fibrocellular proliferation over the internal limiting membrane (ILM) characterizes the epiretinal membrane (ERM). The initiating event in an idiopathic ERM is the posterior vitreous detachment (PVD). Aging vitreous liquefies and detaches from its posterior attachments leading to posterior vitreous detachment. PVD causes dehiscence in the internal limiting membrane, which allows the microglial cells to migrate to the preretinal surface where they interact with the hyalocytes and laminocytes of the vitreous cellular membrane. These cells later transdifferentiate into fibroblast-like cells to form a cellophane thin epiretinal membrane.[4] PVD causes 95% of cases of idiopathic ERM.[5] Retinal folds from ERM contracts to create a macular pucker. Retinal glial cells, hyalocytes, fibroblasts, and myofibroblasts are predominantly seen in idiopathic ERM. Retinal pigment epithelial cells, macrophages, T, and B cells are seen in secondary ERM as inflammation is the triggering event. A prerequisite for the formation of ERM is dehiscence in the ILM most commonly caused by posterior vitreous detachment. The following are the theories hypothesized for the ERM formation:
- Microglial cells migrate to the retinal surface over micro leaks produced by PVD. These cells later differentiate to form the fibroblasts.[6]
- Following PVD, segments of cellular vitreous remain on the surface. These segments contain hyalocytes that transdifferentiate into myofibroblasts from ERM.[7]
- PVD induced ILM avulsion in the posterior paravascular retina upregulates the cytokines to form the ERM.
History and Physical
Most often, patients with epiretinal membrane (ERM) are asymptomatic clinically and are frequently diagnosed during a routine clinical examination. In some patients, ERM progresses to cause metamorphopsia, micropsia or macropsia, photopsia, decreased visual acuity, diplopia, and loss of central vision. Metamorphopsia especially interferes with the quality of life affecting reading, writing, and most of the regular day-to-day activities of living. All asymptomatic patients should be trained to do self-monitoring periodically with Amsler grid charting. History taking should include previous ocular trauma or episodes of floaters or flashes of light, diabetes, hypertension, and hypercholesteremia. ERM causes retinal striae, which progresses in some patients to retinal folds, progressive contracture, and macular pseudohole. Rarely spontaneous separation of the membrane occurs, causing premacular floaters.
Evaluation
Idiopathic epiretinal membrane (IERM) is commonly seen in the elderly beyond 60 years with no sex predilection. Visual acuity, Amsler grid charting, and dilated fundus examination with scleral depression is mandatory in all patients with visual distortion. Watzke Allen test is an ophthalmoscopic test done to differentiate the full-thickness macular hole from a pseudohole. On the slit-lamp fundus examination, the epiretinal membrane (ERM) appears as an abnormal reflectivity of the macular area with loss of normal convex contour and fine wrinkling of the surface. ERM is classified as an early milder form called cellophane macular reflex and a severe late form called preretinal macular fibrosis.[4]
Cellophane macular reflex is seen as a thin transparent membrane overlying the macula with no distortion or impairment of vision. Fundoscopy shows a glistening watery silky light reflex over the macula. Preretinal macular fibrosis occurs in some cases where a cellophane membrane thickens, contracts causing retinal folds and traction lines resulting in impairment of vision and metamorphopsia. Fundoscopy of preretinal macular fibrosis reveals a semi-translucent membrane obscuring the underlying retinal details with retinal fold, traction lines, and vascular tortuosity. Severe cases might show retinal hemorrhages, exudates, macular edema, macula hole, and pseudohole. A defect in the ERM appears as a pseudohole.
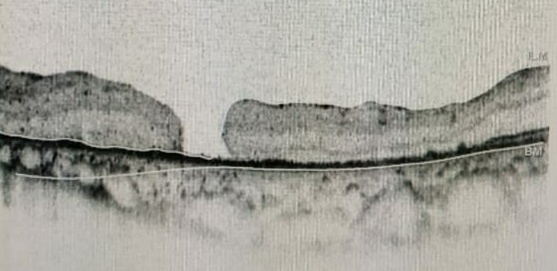
Optical coherence tomography (OCT) is a highly sensitive routinely done investigation for retinal disorders and is the investigation of choice to diagnose epiretinal membrane and vitreomacular traction (VMT). On OCT, an ERM appears as a hyperreflective layer often irregular over the inner surface of the retina. It appears corrugated with peg-like attachments to the retina. Elevation of the foveal depression is seen due to traction from ERM. In severe cases, the inner retina shows folds with thickening of macula along with cystoid spaces. Both ERM and VMT often occur together. Andrea Govetto et al. have studied 194 eyes of 172 patients with ERM with clinical charts and spectral-domain OCT imaging. They found 63 out of 194 eyes showed the presence of continuous ectopic inner foveal layers and is associated with lower visual acuity.[8] They proposed the OCT-based grading system of ERMs as below:
- Stage 1: ERMs were mild and thin. Foveal depression is present.
- Stage 2: ERMs with a widening of the outer nuclear layer and loss of the foveal depression.
- Stage 3: ERMs with continuous ectopic inner foveal layers crossing the entire foveal area.
- Stage 4: ERMs were thick with continuous ectopic inner foveal layers and disrupted retinal layers.
In stages 1, 2, and 3, all retinal layers were clearly defined on OCT. Visual acuity progressively declined from stage 1 through stage 4. Hwang classified idiopathic ERM based on spectral-domain OCT.[9]
Group 1: Fovea-involving ERM
- 1a: Outer retinal thickening and minimal inner retinal change
- 1b: Outer retinal inward projection and inner retinal thickening
- 1c: Prominent thickening of the inner retinal layer
Group 2: Fovea-sparing ERM
- 2a: Formation of a macular pseudohole
- 2b: Schisis-like intraretinal splitting
Dr. Altaweel et al. recently proposed a detailed staging based on OCT observations.[10]
- Stage IA: Foveal splitting with a pseudocyst
- Stage IB: Pseudocyst enlargement and extension to the outer retina with roof intact.
- Stage IIA: Full-thickness macular hole (diameter <400 microns) with posterior hyaloid face remaining attached to the roof of the pseudocyst.
- Stage IIB: Full-thickness macular hole (diameter <400 microns) with an operculum.
- Stage III: Full-thickness macular hole (diameter >400 microns) with surrounding thickened retina, including intraretinal cystoid spaces. The perifoveal and prefoveal hyaloid is separated from the macular retina.
- Stage IV: A stage III hole with a complete posterior vitreous detachment. OCT often cannot visualize the posterior hyaloid because it is too anterior.
A fundus fluorescein angiography or an optical coherence angiography (OCT-A) will help in detecting the retinal pathologies causing secondary ERM such as diabetic retinopathy, choroidal neovascular membrane, retinal telangiectasias, retinal vein occlusions, etc.
Treatment / Management
Most patients with epiretinal membrane (ERM) do not require treatment if it doesn’t affect vision or cause significant metamorphopsia. Blue Mountains study [3] involving 3654 subjects showed that only 20% of epiretinal membranes progressed over five years, 26% regressed, and 39% remained the same. Only 20% of eyes with cellophane maculopathy progressed over a while. The primary treatment for ERM apart from observation is surgical. Surgery for ERM has a reasonable success rate, and most patients show improvement in visual acuity and a decrease in metamorphopsia. Hence the aim of treatment for ERM should be to preserve or improve vision, minimize symptoms like metamorphopsia, diplopia, etc. and enhance the quality of life. Factors that affect the visual outcome include the duration of the condition, the degree of vitreomacular traction, and the cause for ERM. Idiopathic ERM has a better prognosis than ERM secondary to ocular pathology.
Non-surgical management includes the use of vitreopharmacolysis with ocriplasmin. Ocriplasmin is a recombinant proteolytic enzyme approved by the FDA for intravitreal injection for the treatment of symptomatic VMT. Ocriplasmin can relieve the VMT associated with ERM, which might provide relief from the associated metamorphopsia. It does not affect ERM. Its use in patients with both ERM and VMT is controversial. In patients unfit for lengthy retinal surgical procedures, intravitreal ocriplasmin can treat visual disturbances induced by VTM.
Surgical management involves pars-plana vitrectomy (PPV) with ERM and ILM peeling. PPV with membrane peeling has been used successfully for many decades, with an excellent visual outcome and a reduced recurrence rate. ILM is thought to provide a platform for the proliferation of fibroblasts, glial cells, and astrocytes for the retina to form ERM.[11] ILM peeling along with membrane peeling has become a standard procedure following the advent of staining dyes like trypan blue, indocyanine green (ICG), and brilliant blue G (BBG).[12] Triamcinolone is used to stain the vitreous and the membrane. Triamcinolone staining helps to induce posterior vitreous detachment and to ensure an excellent subtotal vitrectomy. Accelerated nuclear sclerosis or a worsening of cataract is the most common complication of vitrectomy. If a cataract is present, the procedure should be combined with a cataract removal to ensure better visualization of the surgical procedure and also to prevent a subsequent second surgery.
Dye assisted ILM peeling has resulted in better visual outcomes, fewer recurrence rates, and reduced retinal striae.[13] Although ILM peeling is beneficial, it is also believed that it might cause damage to muller cells as ILM is the basal lamina which is connected to the endfeet of muller cells.[14][15][16] Due to this uncertainty of the effectiveness versus the damage caused by ILM peeling in idiopathic ERM, many studies have been conducted comparing single peeling (only ERM) and double peeling (ERM and ILM peeling). Vitrectomy with ILM peeling results in visual improvement in long-term follow-ups and lower ERM recurrence rates. While vitrectomy with only ERM peeling is more efficacious in the reduction of a central retinal thickness (CRT) than with vitrectomy with ILM peeling.[17]
Differential Diagnosis
The clinical appearance of the epiretinal membrane (ERM) is clearly remarkable. However, some conditions mimic an epiretinal membrane during their early stages:
- Fine vessel tortuosity: Combined hamartoma of retina and RPE
- Membrane over the retina: Proliferative vitreoretinopathy and tractional retinal detachment.
Prognosis
Epiretinal membrane (ERM) is asymptomatic in its early stage with a good prognosis. Blue Mountains study reveals 39% of the membranes to be non-progressive. Progressive ERM reduces vision and causes annoying metamorphopsia. For worsening ERM, pars plana vitrectomy with membrane and ILM peeling has an excellent prognosis both by improving visual acuity and reducing metamorphopsia. The recurrence of ERM ranges from 1%[18] to 21%.[13]
The recurrence and incomplete recovery of final visual acuity are due to incomplete removal of the membrane. Additional peeling of ILM removes the platform for cellular proliferation. One study has suggested that photoreceptor disruption detected by OCT and P1 implicit time delay on multifocal electroretinogram as significant predictors for poor visual recovery after ERM surgery.[19] To date, the most determining risk factor, which predicts the post-operative visual recovery, is the duration of the ERM.
Complications
Epiretinal membrane (ERM) can cause various ocular complications, and these include:
- Accelerated nuclear sclerosis or cataract formation
- Retinal breaks or detachment
- Macular toxicity (trauma/light)
- Endophthalmitis
- Macular hole
- Vitreous hemorrhage
- Retinal petechiae/hemorrhage
- The dissociated optic nerve fiber layer
Deterrence and Patient Education
Patients should be informed that most epiretinal membranes which do not affect the vision or cause metamorphopsia are best left alone. Periodic self-assessment with Amsler grid charts would help one to assess the beginning or progression of metamorphopsia. Besides, self-monitoring monocular vision also helps to detect early central vision changes. Patients should also be made aware that surgical procedures for epiretinal membrane (ERM) are very successful in addressing visual acuity symptoms and improve quality of life. Patient education and appropriate counseling will help patients to have realistic expectations.
Enhancing Healthcare Team Outcomes
Diagnosis and management of the epiretinal membrane (ERM) require appropriate diagnostic and surgical skills in addition to the availability of special equipment. Even though the diagnostic procedures are done by trained personnel, interpretation and diagnosis are made by a trained ophthalmologist. Hence appropriate referral to an ophthalmologist is mandatory for patients who present to primary eye care with decreased visual acuity and metamorphopsia unresolved by refractory correction. Surgical management needs intervention from a retinal surgeon, and hence a liaison between a general ophthalmologist or optometrist is mandatory in the care of patients with epiretinal membranes.