Continuing Education Activity
This activity reviews the different types of thyroiditis, their presentation, evaluation, diagnosis and treatment and highlights the role of the interprofessional team to work closely with endocrinology in recognizing the correct type of thyroiditis and instituting appropriate timely management of patients with this disease.
Objectives:
- Identify the etiology of different kinds of thyroiditis.
- Review the appropriate evaluation of a patient presenting with signs and symptoms of thyroiditis.
- Outline the management options available for various types of thyroiditis.
- Discuss interprofessional team strategies for improving care coordination and communication to manage thyroiditis and improve patient outcomes.
Introduction
The term thyroiditis reflects inflammation of the thyroid gland. Thyroiditis can be classified based on the onset of symptoms, underlying etiology, and clinical symptoms. The most common cause of thyroiditis is an autoimmune disease. In the United States, Hashimoto thyroiditis is the most common cause of hypothyroidism.[1] Thyroiditis can cause transient or permanent hypo and hyperthyroidism.
Etiology
Thyroiditis can occur due to autoimmune disease (Hashimoto thyroiditis, Graves disease, postpartum thyroiditis or painless sporadic thyroiditis), infection (painful subacute thyroiditis or suppurative thyroiditis), drugs (amiodarone, lithium, interferons and interleukin-2; and checkpoint inhibitors) or fibrosis (Riedel thyroiditis)
Painful thyroiditis encompasses infectious, subacute thyroiditis, traumatic or radiation-induced thyroiditis, and painless thyroiditis encompass autoimmune, postpartum, and drug-induced thyroiditis.
It can be classified into acute, subacute, and chronic thyroiditis.
Acute thyroiditis is caused by bacterial infection of the gland.
Subacute, also known as granulomatous thyroiditis, is caused by viruses.
Chronic includes autoimmune thyroiditis, Hashimoto thyroiditis, postpartum thyroiditis, and other painless thyroiditis, including iatrogenic and drug-induced thyroiditis.
Acute Thyroiditis
Infectious thyroiditis: Infection of the thyroid gland is rare as it is encapsulated with rich blood supply and extensive lymphatic drainage. This is usually seen in the elderly, chronically ill and immunocompromised patients.[2] It is most commonly caused by gram-positive bacteria like Staphylococcus or Streptococcus. Sometimes mycobacteria and fungi, including pneumocystis, can be the culprit in immunocompromised patients. Source of infection is usually hematogenous or congenital abnormalities like pyriform sinus usually seen in children.
Radiation-induced thyroiditis: Radiation treatment of neck cancer can cause thyroiditis, followed by hypothyroidism. Patients who receive radioactive iodine for ablation of Graves disease occasionally develop severe thyroid pain 7 to 10 days after therapy. It is rare, and the incidence is about 1%.
Subacute Thyroiditis
It is usually preceded by upper respiratory tract infections and is presumed to be due to a viral illness, though definite evidence is lacking.[3] There is also a strong association with HLA -35.[4]
Chronic Thyroiditis
Autoimmune thyroiditis: It includes Hashimoto thyroiditis and postpartum thyroiditis and its association with HLA-DR3, HLA-DR4, HLA-DR5 has been reported in Whites.[5][6][7] Hashimoto thyroiditis is the most common cause of hypothyroidism in the United States. It is presumed to be due to a viral infection, with the viral structure being similar to thyroid protein leading to the production of antibodies against the thyroid gland. Approximately 10% of the general population in the US has a high concentration of these antibodies, but the majority of them have normal thyroid function tests.[8] However, there is a risk of progression to overt hypothyroidism in such individuals.
Postpartum thyroiditis: It is an autoimmune phenomenon where antibodies formed against fetal thyroid cells accumulate in the mother's thyroid gland.[9] It occurs in postpartum women within one year of childbirth. The maternal presence of positive thyroid peroxidase antibody or other autoimmune diseases is a risk factor.
Drug-induced thyroiditis: The most common drugs causing thyroid dysfunction are amiodarone, lithium, and tyrosine kinase inhibitors.
Amiodarone can cause both hyper and hypothyroidism. In euthyroid individuals, amiodarone can cause transient changes in thyroid function tests (TFT), followed by normalization. In patients who have underlying Hashimoto, or pregnant are at risk of developing worsening hypothyroidism. It is thought to be secondary to the antithyroid effect of the iodine in amiodarone. Amiodarone can induce hyperthyroidism in two ways. In type 1, there is increased synthesis and release of thyroid hormone, whereas, in type 2, there is destructive thyroiditis leading to the release of preformed T4 and T3 from the damaged thyroid gland.
Checkpoint inhibitors are a type of immunotherapy with anti-neoplastic properties and include drugs like nivolumab, ipilimumab, pembrolizumab, and atezolizumab. They are associated with endocrinopathies especially, hypothyroidism secondary to destructive thyroiditis.[10] Patients usually present with vague symptoms of hypothyroidism like fatigue, weight gain. It should be distinguished from secondary hypothyroidism as these drugs also cause hypophysitis. Hyperthyroidism though very rare, is also seen.
Lithium is known to cause hypothyroidism by decreasing the secretion of thyroid hormones. This causes a rise in TSH and eventually enlargement of the thyroid gland and goiter. About 15% of patients on interferon alfa therapy can develop thyroid dysfunction.[11] Thyroid abnormalities, including both hyper and hypothyroidism, can be seen in patients on tyrosine kinase inhibitors, especially sunitinib and lenvatinib.
Riedel thyroiditis: Reidel thyroiditis is a rare condition characterized by progressive fibrosis of the thyroid gland. The exact etiology is unclear, but recent data indicate that it is closely related to IgG-4 related sclerosing disease. The fibrosis of the thyroid gland may or may not be associated with progressive fibrosis of other organs.[12]
Epidemiology
Hashimoto thyroiditis is the most common cause of hypothyroidism, while Graves disease is the most common cause of autoimmune hyperthyroidism in the United States. High intake of iodine can increase the incidence of Graves disease, whereas iodine insufficiency can be protective against autoimmune thyroiditis.[13]
Pathophysiology
Acute Thyroiditis
Infectious thyroiditis is caused by gram-positive bacteria like streptococcus, staphylococcus, or fungi, mycoparasitic infection.[2]
The destruction of thyroid parenchyma causes radiation-induced thyroiditis after exposure to radioactive iodine for treatment of Graves disease or thyroid cancer and high dose radiation to the neck for the lymphoma and other head and neck cancers.
Subacute Thyroiditis
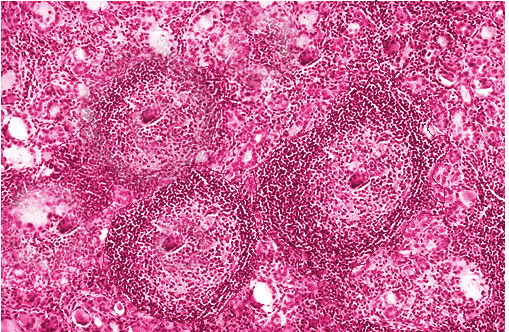
This is caused by viruses like coxsackie A, B, echovirus. Granulomas are formed in the thyroid gland, which becomes fibrotic but can return to normal after treatment.
Chronic Thyroiditis
Hashimoto thyroiditis is an autoimmune phenomenon characterized by lymphocytic infiltration of the gland presumed to be due to similarities between thyroid protein and the viral structure resulting in cross-reacting antibodies. Anti-TPO antibodies that are present in 90% of patients with Hashimoto thyroiditis fix complement and are hence capable of inducing antibody-dependent cell-mediated cytotoxicity, causing the death of thyrocytes.[14]
Postpartum thyroiditis is a destructive thyroiditis characterized by lymphocytic infiltration of the thyroid gland. Fetal cells that migrate to the maternal thyroid gland tend to survive the immunocompromised pregnancy state, and when the maternal immune system rebounds postpartum, it activates the autoimmune phenomenon and causes postpartum thyroiditis.[15][16]
Drug-induced thyroiditis causing hyperthyroidism is usually caused by either an increase in the release and synthesis of thyroid hormone or by destructive thyroiditis caused by the release of preformed hormones. Whereas hypothyroidism is caused by a decrease in the synthesis and release of thyroid hormone or from hypophysitis causing secondary hypothyroidism. The iodine content of the drugs also causes thyroid dysfunction.
Reidel’s thyroiditis: Pathophysiology is not completely understood, but chronic inflammation by the mononuclear cells seems to play a role. It has also been claimed as IgG4 thyroid disease, which includes Reidel thyroiditis, autoimmune pancreatitis, interstitial pneumonia, and orbital pseudotumors.[12]
History and Physical
Acute and Subacute Thyroiditis
Symptoms of upper respiratory tract infection could indicate subacute thyroiditis, and other infective symptoms like fever and neck pain could indicate acute infectious thyroiditis. History of recent radiation to the neck or radioactive iodine treatment could indicate radiation-induced thyroiditis.[17]
On physical exam, most acute thyroiditis patients have a tender and inflamed thyroid gland.
Chronic Thyroiditis
For chronic thyroiditis, a detailed history is paramount to narrowing the etiology. Medication history is important to diagnose underlying drug-induced thyroiditis. Personal history and family history of autoimmune disease can help discover any increased risk of autoimmune thyroid disease. Symptoms related to local compressive symptoms in the neck, including difficulty swallowing or choking sensation or hoarseness of the voice, could indicate underlying large goiter or large thyroid nodule or Riedel thyroiditis. Patients with Riedel thyroiditis usually present with dysphagia, odynophagia, respiratory distress due to the compression of the trachea, esophagus, and also because of the extension of the fibrosis.[18]
Physical exam should include a detailed thyroid exam to evaluate any enlargement, tenderness on palpation, any abnormality in the texture, or any palpable nodules.
Drug-induced thyroiditis can be clinically benign on the exam. Symptoms of hypothyroidism like weight gain, fatigue, constipation, dry skin in patients on amiodarone should raise the suspicion of drug-induced thyroiditis. Amiodarone can also cause hyperthyroidism, and clinical manifestations may be masked initially because amiodarone has beta-adrenergic blocking activity. Check-point inhibitor immunotherapy: Patients usually present with vague symptoms of hypothyroidism like fatigue, weight gain. It should be distinguished from secondary hypothyroidism as these drugs also cause hypophysitis.[19]
Autoimmune thyroiditis and Hashimoto thyroiditis usually present with a painless goiter.
Postpartum thyroiditis usually presents with symptoms of thyrotoxicosis like tachycardia, nervousness, and diarrhea with a history of recent childbirth.[20]
Patients with Riedel thyroiditis can have a fixed, hard, painless goiter on physical exam. Most of the patients are euthyroid but can develop hypothyroidism.[18]
Evaluation
Thyroid-stimulating hormone (TSH) should be checked to see if the patient has hyperthyroidism or hypothyroidism. Thyroid microsomal antibodies and thyroid receptor antibodies can be checked for confirmation of autoimmune thyroid disease. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are significantly elevated in infectious thyroiditis (bacterial).[2]
Thyroid ultrasound is the most important and most commonly used imaging modality for evaluation of the thyroid gland. Heterogenous thyroid parenchyma indicates inflammation of the thyroid gland, but it does not differentiate between production versus destruction thyroiditis. Thyroid ultrasound can also detect nodules in the thyroid gland. The characteristics of nodules can help to differentiate between benign or malignant nodules.
A thyroid uptake and scan can be done to differentiate production thyroiditis or destruction thyroiditis in patients who present with thyrotoxicosis characterized by low TSH with or without elevated T4 and T3. Low uptake on thyroid scan would indicate destruction thyroiditis (Hashimoto thyroiditis, infectious thyroiditis), while increased or normal uptake indicates production thyroiditis (Graves disease).[14] A thyroid scan can help to further differentiate production thyroiditis into Graves disease, which will show increased uptake throughout the thyroid gland or toxic adenoma, which will show increased uptake in the nodule (hot nodule) with suppression of rest of the thyroid gland.
Fine-needle aspiration is done to evaluate suspicious thyroid nodules to rule out malignancy. In general, any thyroid nodule, which is less than 10 mm, can be monitored without fine-needle aspiration.
Acute Thyroiditis
Thyroid ultrasound, blood cultures, fine needle aspiration with gram stain should be obtained when the clinical presentation is suspicious of infectious thyroiditis. Thyroid function tests are usually normal, but in rare cases, hypo or hyperthyroidism may be present. In cases of radiation thyroiditis, there is a preceding history of radiation exposure or treatment with radioactive iodine for likely Graves disease, which will guide in the diagnosis.
Subacute Thyroiditis
There is a strong association with HLA-35. ESR and CRP are markedly elevated, and so is leucocyte count. T4, T3, and TSH can vary depending on the hyperthyroid or hypothyroid phase. The iodine uptake is low, distinguishing the thyrotoxic phase from Graves disease.[21]
Chronic Thyroiditis
Diagnostic tests for autoimmune/Hashimoto thyroiditis include thyroid peroxidase antibody, which is present in 90% of the patients and thyroglobulin antibody, which is present in 20% to 50%. Thyroid function tests show a hypothyroid picture with high TSH and low T3 and T4. It is associated with HLA-DR3, HLA-DR4, HLA-DR5 in Whites.[14][21]
In patients who are on drugs like amiodarone, lithium, interferon, interleukin 2, and checkpoint inhibitors should have baseline TSH at the commencement of treatment.[19][22] TSH, free T4, free T3 should be obtained in case of the development of symptoms of thyroid dysfunction. Thyroid ultrasound with an iodine uptake scan can be obtained to distinguish drug-induced destructive inflammatory thyroiditis from Graves disease. Uptake is low in drug-induced inflammatory thyroiditis and high in Graves disease.
Postpartum thyroiditis presents with symptoms of hyperthyroidism and history of recent pregnancy and should be evaluated with TSH, free T4, free T3. It can be distinguished from Graves disease by 24-hour iodine uptake scan, and the uptake is low in postpartum thyroiditis.[20]
Riedel thyroiditis: Biopsy is necessary for definitive diagnosis. FNA may not be sufficient for diagnosis and may require an open biopsy for definitive diagnosis of this disease.[23][18]
Treatment / Management
Acute Thyroiditis
Infectious thyroiditis: Patients with suppurative thyroiditis can be managed with nonsurgical management. Antibiotics are used to control infection. NSAIDs are used to control severe neck pain and inflammation. Surgical intervention, like abscess drainage, can be done if clinically indicated.[2]
Radiation-induced thyroiditis: Treatment is symptomatic with NSAIDs or prednisone in severe cases. These patients are increased risk of hypothyroidism and should be followed with a thyroid function test.[24]
Subacute Thyroiditis
It is usually self-limiting, and symptomatic management is all that is needed. NSAIDs are preferred for pain control. In case of severe pain and severe symptoms of thyrotoxicosis, corticosteroids, and beta-blockers can be used for the treatment of inflammation and tachycardia due to thyrotoxicosis. The hypothyroid phase is usually mild and does not require treatment.[25]
Chronic Thyroiditis
Autoimmune thyroiditis: Hashimoto thyroiditis with normal thyroid function can be monitored without treatment with levothyroxine.[14] Hyperthyroidism or Graves disease can be treated with methimazole or propylthiouracil. Methimazole is the drug of choice, but propylthiouracil is preferred during the first trimester of pregnancy and for treatment of the thyroid storm. Permanent treatment of Graves disease included radioactive iodine treatment and thyroidectomy.[26]
Postpartum thyroiditis: It is usually transient, and 80% of patients eventually become euthyroid. Hypothyroid patients can be treated with levothyroxine and monitored with regular thyroid function.[20]
Amiodarone induced thyroiditis: It can cause both hypothyroidism and hyperthyroidism.[27]
Hypothyroidism- Once diagnosed, amiodarone is usually continued along with levothyroxine replacement. If amiodarone is stopped for a different reason, individuals without previous thyroid dysfunction usually progress to euthyroid state with the withdrawal of amiodarone.[27]
Hyperthyroidism - Treatment of type I hyperthyroidism is done with beta-blockers and methimazole. For type 2 thyroiditis, the use of glucocorticoids is recommended to alleviate the hyperthyroid symptoms.
Lithium: Treatment is to continue lithium and start treatment with levothyroxine. It can also cause hyperthyroidism and Graves disease secondary to goiter formation.[11]
Riedel thyroiditis: Treatment is surgical.[23]
Differential Diagnosis
Differential diagnosis of symptomatic thyroiditis includes acute hemorrhage into thyroid cyst, thyroid nodule, thyroid cancer, tonsillitis, and acute pharyngitis.
Prognosis
Thyroiditis with or without thyroid dysfunction has a good prognosis, but long-standing hypothyroidism can predispose to myxedema come, which is more common in the elderly population and has a high mortality rate. Many patients with hypothyroid may have ongoing symptoms even with treatment, which may affect the quality of life.
Complications
Myxedema coma: It is a medical emergency and is characterized by severe hypothyroidism with clinical features of hypothermia, hyponatremia, bradycardia. It is mostly seen in older patients. Treatment should be initiated on clinical suspicion without awaiting lab results. Steroids are given first followed by thyroxine replacement to prevent an adrenal crisis in the scenario of underlying adrenal insufficiency.[28][29]
Thyroid storm is a life-threatening endocrine emergency often triggered by a metabolically stressful event in a patient with long-standing hyperthyroidism like Graves disease. It can present with hyperpyrexia, tachycardia, agitation, and psychosis with laboratory evidence of low TSH, high free T4, and T3. Prompt recognition and treatment of the condition are necessary as this condition is associated with high mortality. The Burch-Wartofsky diagnostic criteria can help with the timely detection of thyroid storm.[30] The standard of care is immediate initiation of beta-blockers, thionamides, and glucocorticoids. Additionally, iodine and cholestyramine can also be used.[31]
Infectious thyroiditis can lead to an abscess and septicemia if not treated promptly.[2]
Patients with Hashimoto thyroiditis are at risk of developing thyroid lymphoma and carcinoma; thus, a rapidly progressing thyroid nodule enlargement or development of new nodules should raise the suspicion.
Deterrence and Patient Education
Thyroiditis is a condition that occurs when the thyroid gland gets inflamed. The thyroid gland is responsible for making a hormone called thyroxine, which controls the human body's metabolism and energy utilization. When the gland is inflamed, due to any cause, it could make insufficient or excessive hormone, which causes symptoms like fatigue, weight gain, depression or palpitations, weight loss, and anxiety, to name a few.
Consult with your doctor to discuss the right treatment as the management varies depending on the type of thyroiditis, and the physician needs to investigate and follow up with laboratory tests to ensure continued management of the thyroiditis.
Enhancing Healthcare Team Outcomes
Thyroiditis comprises of a group of diseases that can present with strikingly similar symptoms. This frequently poses a diagnostic dilemma to uncover the exact etiology. These patients may present with hyper or hypothyroid symptoms with subtle differences depending on the etiology. A thorough history and physical examination is the key to uncover these subtle differences. It is also important to consult with an endocrinologist to investigate the exact etiology of thyroiditis as well as to help institute the correct treatment and reduce patient morbidity.
The current guidelines for management have been developed with expert recommendations and literature from peer-reviewed journals to determine the appropriateness of laboratory testing and imaging, as well as the formulation of and treatment strategies.