Continuing Education Activity
Thymic hyperplasia could be true thymic or lymphoid hyperplasia. It is usually found incidentally or could present with compressive symptoms or systemic symptoms due to autoimmune disease like myasthenia gravis. The diagnosis is made through a chest CT or MRI. Treatment for symptomatic patients is mostly thymectomy. This activity describes pathophysiology, evaluation, and management of thymic hyperplasia and highlights the role of the interprofessional team in the evaluation and treatment of patients with thymic hyperplasia.
Objectives:
- Describe the etiology of thymic hyperplasia.
- Review the evaluation of a patient with thymic hyperplasia.
- Outline the treatment of a patient with thymic hyperplasia.
Introduction
The thymus got its role in T-cell differentiation discovered a few decades ago before the 1960s it was considered vestigial. Though largely known as a lymphoid organ and for its role in T-cell differentiation, thymus also has an endocrine role that includes manufacturing thymosin that regulates T-cell differentiation and other humoral factors that regulate cell growth, maturation and guide the process of mineralization.[1] The thymus is the principal location for T-cell lymphopoiesis. The production of functional T-cell is choreographed by thymic epithelial cells that guide them in proliferation, maturation, and survival. The thymic epithelial cells are compartmentalized into two main populations medullary thymic epithelial cells and cortical thymic epithelial cells. These populations are further segregated into distinct subpopulations having specific molecular and functional roles.[2]
Thymic hyperplasia alludes to an increase in the size of thymus due to an increase in the number of cells. Thymus achieves its peak size around puberty and then atrophies slowly. Thymic hyperplasia is not always pathological, but the growth of the thymus to a certain degree not anticipated for a patient’s age raises the alarm and should lead to further investigation.
Etiology
There are two major etiologies of thymic hyperplasia. It could be congenital or acquired. The congenital thymic hyperplasia can be hypo functioning or hyperfunctioning and is found to be the result of neuroendocrine disturbances, usually within the hypothalamic-hypophyseal system. Thymic hyperplasia with hypo functioning thymus would lead to immune deficiency. Hyperfunctioning thymic hyperplasia could lead to autoimmune diseases, most commonly myasthenia gravis, but the relationship has also been found with graves' disease and collagen vascular disorders. Acquired thymic hyperplasia can also result in hypo functioning or hyperfunctioning thymus.[3][4]
Acquired thymic hyperplasia is usually a rebound phenomenon in patients who have undergone chemotherapy, have had thermal burns, cardiac surgery, or after discontinuation of oral steroids as the thymus is susceptible to fluctuations in corticosteroids.
Epidemiology
Thymic masses are the most common abnormal growths in the anterior mediastinum. Among the pediatric population, thymic hyperplasia is the most common benign tumor of the anterior mediastinum. In adults, the incidence is increased between the ‘40s and ‘50s; it is similar in men and women. An increased incidence among Asians has been reported compared to other races. Thymic hyperplasia is mostly discovered incidentally in about 50% to 70% of patients with myasthenia gravis. 75% of the patients with myasthenia gravis have thymic disease. Out of 75 %, 85% have thymic hyperplasia, and 10% to 15% have thymoma.
Pathophysiology
There are two morphological forms of thymic hyperplasia:
True thymic hyperplasia: It is characterized by an increase in the size and weight of thymus due to an increase in the number of thymic epithelial cells. The normal histology of the thymic cells is preserved. This form of thymic hyperplasia is more prevalent among children and young male patients. It is not associated with autoimmune diseases. The most common presentation of this type is usually respiratory distress or peripheral blood lymphocytosis.[5]
Lymphofollicular hyperplasia: It is caused due to hyperplastic lymph follicles within the thymus. The follicles stem in the medulla and interlobular septal space that shifts the parenchyma of the thymus.[6] These reactive lymphoid follicles are similar to normal follicles. Histologically these lymphoid follicles have numerous diverse lymphoid cells supplemented with germinal center cells of different sizes and macrophages containing cellular debris. Thus, the main characteristic of lymphofollicular thymic hyperplasia is the development of ectopic germinal centers and neo-angiogenesis. This form of thymic hyperplasia is associated with autoimmune diseases like myasthenia gravis or graves' disease.[7]
History and Physical
A comprehensive history and a detailed physical examination are necessary to evaluate patients with thymic hyperplasia, focusing on its signs and symptoms. Thymic hyperplasia is usually discovered incidentally after imaging is performed for an unrelated chest complaint. The thymus is located in the anterior mediastinum closely related to airways and major blood vessels. Thymic hyperplasia can compress these structures, causing the following symptoms:
- Shortness of breath
- Dysphagia
- Cough
- Loss of appetite
- Weight loss
- Chest pain
The thymus is located near the superior vena cava, and a massive true thymic hyperplasia could compress it, leading to superior vena cava syndrome.[8] The superior vena cava syndrome would present as:
- Swelling of face, neck, and upper chest
- Cyanosis
- Headaches
- Dizziness
- Lightheadedness
- Dyspnea
- Venous dilatation over the trunk
- Facial Flushing
- Stridor
- Neurologic signs
The lymphofollicular thymic hyperplasia is associated with autoimmune diseases like myasthenia gravis, Graves disease, or collagen vascular disorders. Patients with these autoimmune disorders can present with varying signs and symptoms depending upon the underlying disorder.
- Myasthenia gravis: It is a neurological autoimmune disease caused by autoimmunity against the acetylcholine receptor component of the neuromuscular junction. The lymphofollicular form of thymic hyperplasia is evidently involved in the pathogenesis of myasthenia gravis with anti-acetylcholine receptor antibodies.[7] It is characterized by a fluctuating degree and varying amalgamation of weakness in an ocular, bulbar, limb, and respiratory muscles. T-cell dependent autoantibodies attack the acetylcholine receptors on the postsynaptic membrane leading to muscular weakness.
- Graves disease: The relation between thymic hyperplasia and Graves' disease was first described in 1912. Patients with Graves' disease should undergo a thorough evaluation of thymus. There seems to be a complex hormonal and immunological mechanism involved, but the exact pathogenesis is unclear.[9] Most patients with Graves disease can be diagnosed with thymic hyperplasia by undergoing clinical evaluation and radiological studies. The treatment of hyperthyroidism due to Graves disease leads to the rapid resolution of thymic hyperplasia.[10]
Evaluation
Laboratory studies: Acetylcholine receptor antibodies may be positive in some patients with thymic hyperplasia, pointing towards the presence of myasthenia gravis.
Imaging: The thymic hyperplasia is usually discovered incidentally on radiographical imaging for pre-op of some elective surgery or unrelated chest complaints. The findings of a chest radiograph can range from subtle mediastinal findings to large mass or widened mediastinum.[11]
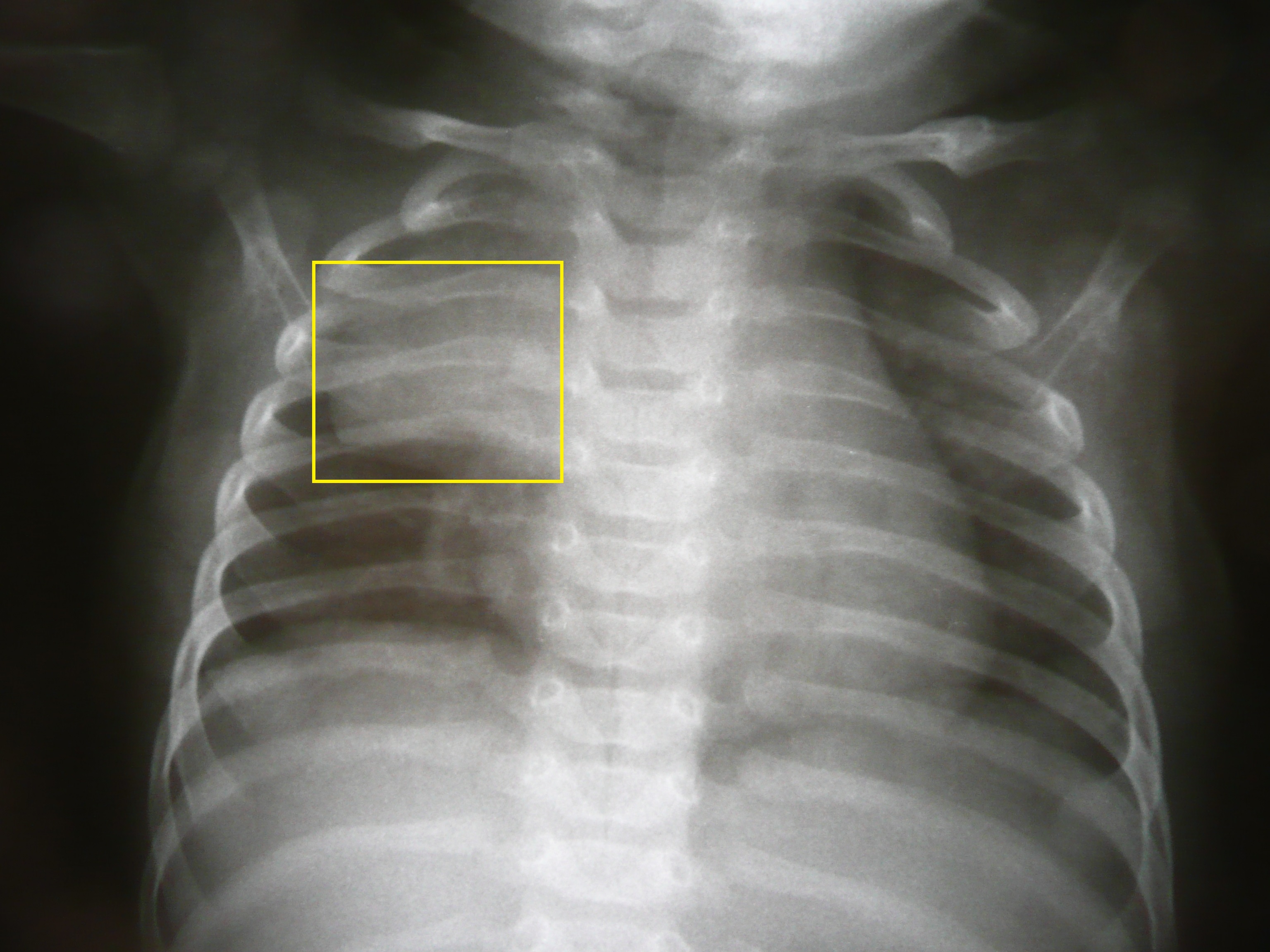
Chest X-Ray: A frontal chest X-ray of infants and young children show a strikingly large thymus and a sail sign can be seen. The thymus normally remains visible on the radiograph till the age of 3 years. On conventional radiography, thymic hyperplasia usually appears normal.
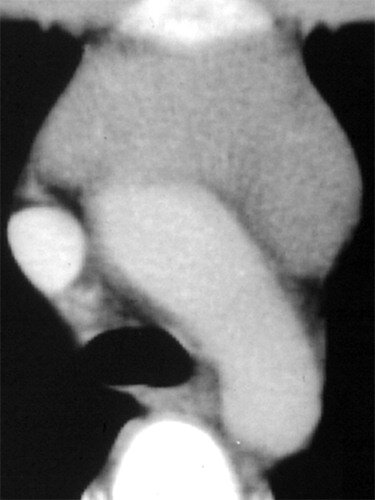
Chest CT-scan: Contrast-enhanced computed tomography is typically used for thymic abnormalities not detected on conventional radiography. In most cases, chest CT-scan is diagnostic. Chest CT-scan can provide comprehensive information about mediastinal abnormality, inclusive of its location, size, relation to surrounding structures, and it can also give you information about the presence of fluid, fat, or calcifications within the tissue. CT-scan of a hyperplastic thymus exhibits diffuse enlargement, preserved contour, normal blood vessels, and a mixture of lymphoid tissue and fat. This precise information is important, especially involvement or compression of related structures in order to plan treatment or resection in severe cases.[12]
PET-CT: A hyperplastic thymus demonstrates only mild uptake of fluorodeoxyglucose as compared to marked uptake in case of malignancy.
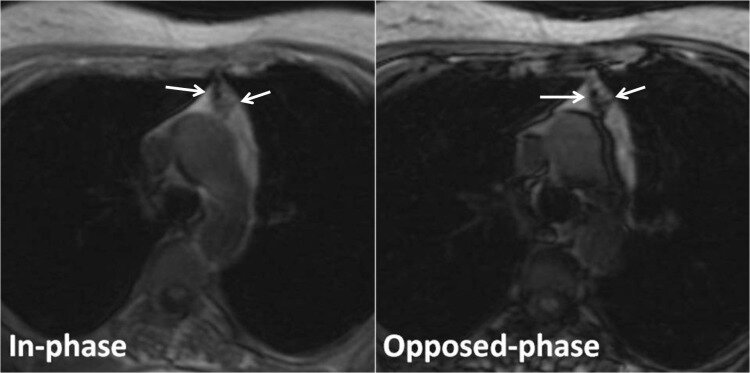
Chest MRI: Chemical shift MRI usually demonstrates chemical shift artifact between in-phase and out of phase images and can help differentiate thymic hyperplasia from thymic neoplasia. It can be challenging to differentiate between normal and hyperplastic thymus; so following guidelines should be used to identify a normal thymus:
- Soft tissue mass should not be greater than 7mm.
- The contour of thymus should not be convex in a young adult.
- Soft tissue must not be ovulated.
- Symptoms of diseases related to thymic hyperplasias such as myasthenia gravis or graves' disease should not be present.[13]
- Biopsy: In the case of true thymic hyperplasia, the cortex and medulla are normal. Thymic cells are normal on FNA. Lymphofollicular hyperplasia has normal lymphoid follicles with additional germinal centers, dispersed thymic cells, and a few macrophages.
Treatment / Management
Massive thymic hyperplasia: Asymptomatic patients with diffusely enlarged thymus glands can be followed up expectantly because they have a negligible incidence of significant thymic disease. The major treatment of massive thymic hyperplasia is surgical resection.[14]
Lymphofollicular hyperplasia: The management of lymphofollicular type of thymic hyperplasia depends on how it manifests. Depending upon the signs and symptoms, it could have the following approaches towards treatment.
Myasthenia gravis: Acetylcholinesterase inhibitors such as physostigmine or pyridostigmine could be used for the symptomatic treatment of myasthenia gravis resulting from thymic hyperplasia. These agents act by inhibiting hydrolysis of acetylcholine in synaptic cleft leading to the availability of more acetylcholine to interact with remaining acetylcholine receptors not yet effected by autoantibodies. Corticosteroids can help improve the symptoms of myasthenia gravis, especially in the case of myasthenic crisis. However, the exact mechanism by which steroids act to help with symptoms has not been well understood.[15] Plasma exchange therapy could also help improve symptoms of myasthenia gravis, and it is relatively less costly.[16] Thymectomy is the surgical removal of the thymus gland. There is evidence that thymectomy leads to remission and decreased drug dependency.
Graves disease: Thymic hyperplasia due to Graves' disease usually resolves as the hyperthyroidism is treated and is under control.[10][17]
Differential Diagnosis
- Thymolipoma: This accounts for almost 10% of thymic masses, especially in young adults.
- Thymoma: Accounts for 50% of anterior mediastinal masses and 20% of mediastinal tumors.
- Thymic cysts: Identified in 3% of patients with an anterior mediastinal mass
- Malignant thymoma
- Thymic carcinoid: It is a rare disorder found in some patients with MEN 1 syndrome.
- Thymic germ cell tumor: Accounts for 15% of anterior mediastinal masses usually seen in young adults.
Prognosis
- Thymectomy has been proven to achieve complete stable remission in patients having myasthenia gravis due to thymic hyperplasia.[18]
- Thymic hyperplasia related to Graves' disease resolves rapidly as the hyperthyroidism gets treated.[10]
- Overall, thymic hyperplasia has a good prognosis.
Complications
- Superior vena cava syndrome: It is a group of symptoms arising from decreased blood flow from superior vena cava to right atrium leading to swelling of neck, face, and upper limb, dyspnea, cough, headaches, dizziness, lightheadedness. The treatment depends on the etiology of obstruction, which in the case of thymic hyperplasia is thymectomy.
- Myasthenia gravis
- Respiratory distress
Consultations
Following consultations should be obtained:
- Radiologist
- Thoracic surgeon
- Neurologist
- Endocrinologist
- Pathologist
Deterrence and Patient Education
Patients with thymic hyperplasia can present differently. The patient could present with compressive symptoms such as dyspnea, dysphagia, cough, horner syndrome, superior vena cava syndrome, or systemic symptoms like weakness and blurry vision due to autoimmune disease like myasthenia gravis. But usually, the thymic hyperplasia is an incidental finding. The newly diagnosed patient should be given emotional support and detailed information about the condition, its treatment, prognosis, and effects on everyday life.
- Asymptomatic patient: If the thymic hyperplasia is asymptomatic, the patient should be guided about follow up, and observation until the condition remains asymptomatic and steps that will be taken if somehow the condition starts showing symptoms in the future.
- Compressive symptoms: The patients presenting with compressive symptoms should be informed about the cause of symptoms and the possibility of surgery, i.e., thymectomy, to relieve the symptoms.
- Myasthenia gravis: Myasthenia gravis patients should be informed about possible associated between thymic hyperplasia and their condition and the possible need for surgery, i.e., thymectomy in the future to improve their symptoms if the medications and plasma exchange therapy fail to improve the symptoms.
- Thymic hyperplasia and Graves disease: In the case of thymic hyperplasia associated with hyperthyroidism due to grave disease, the patient should be guided that the hyperplasia will subside if hyperthyroidism is controlled.
The patient should be provided with educational material about the disease. Flow charts, diagrams, and videos should be used to explain each and every aspect of the disease, treatment, and lifestyle changes. Until the patient fully understands everything and is satisfied with the provision of care.
Pearls and Other Issues
Here are a few important points to take note:
- The thymus has a major role in T-cell differentiation and maturation.
- Thymic hyperplasia is the increase in the size of the thymus due to an increase in the number of cells.
- Thymic hyperplasia could be congenital or acquired, leading to hypo functioning or hyperfunctioning thymus.
- Thymic hyperplasia could be due to an increase in the number of thymic epithelial cells or hyperplastic lymphoid follicles.
- Hyperplastic thymus can cause local symptoms like cyanosis, dyspnea, superior vena cava syndrome due to compression of local structures.
- It can also cause systemic symptoms due to autoimmune diseases like myasthenia gravis.
- CT-scan or MRI of the chest is used for diagnosis.
- The best treatment is usually thymectomy.
- Thymic hyperplasia usually has a good prognosis.
Enhancing Healthcare Team Outcomes
It is the responsibility of healthcare professionals that the patient has a good understanding of the disease and the appropriate treatment available for the disease. Thymic hyperplasia is usually an incidental finding and can cause significant anxiety among patients. It is vital for healthcare providers to provide emotional support to the newly diagnosed patient. The approach to hyperplastic thymus should be multidisciplinary, including primary care physician, physician assistant, nurse practitioner, radiologist, pathologist, thoracic surgeon, neurologist, and an endocrinologist in order to establish a definitive diagnosis and provide appropriate treatment.
If the diagnosis of thymic mass is an incidental finding, a biopsy should be performed to differentiate thymic hyperplasia from thymoma or other malignancies and make a definitive diagnosis. Patients who are asymptomatic and have no local or systemic manifestations can be closely monitored by primary care providers. Patients with serious manifestations such as superior vena cava syndrome or myasthenia gravis should be referred to a thoracic surgeon for thymectomy.