Continuing Education Activity
Madelung deformity is a developmental or acquired deficiency of the volar-ulnar aspect of the distal radius. This condition can lead to a cosmetic or functional wrist deformity. The classic congenital form of the deformity is proposed to be due to an abnormal Vickers ligament, leading to restricted distal radius growth at the volar-ulnar corner. Consequently, radial inclination and volar tilt increase, causing lunate subsidence and altering carpal kinematics.
A similar deformity, referred to as "Madelung-like deformity," is associated with other conditions, including posttraumatic injuries, multiple hereditary exostoses, Ollier disease, and gymnast's wrist. Patients usually present with wrist pain, decreased grip strength, and progressive wrist range-of-motion loss. Management of patients with symptomatic Madelung deformity is primarily operative, with surgical options depending on the timing of diagnosis.
This overview highlights the evaluation and management of Madelung deformity and reviews the role of the interprofessional team in managing patients with this condition.
Objectives:
Identify physical manifestations and clinical features indicative of Madelung deformity, distinguishing it from other wrist pathologies..
Differentiate between different stages and types of Madelung deformity, assessing severity and functional impact.
Implement appropriate treatment plans considering conservative measures or surgical interventions for Madelung deformity.
Collaborate with the interprofessional team to educate, treat, and monitor patients with Madelung deformity and improve patient outcomes.
Introduction
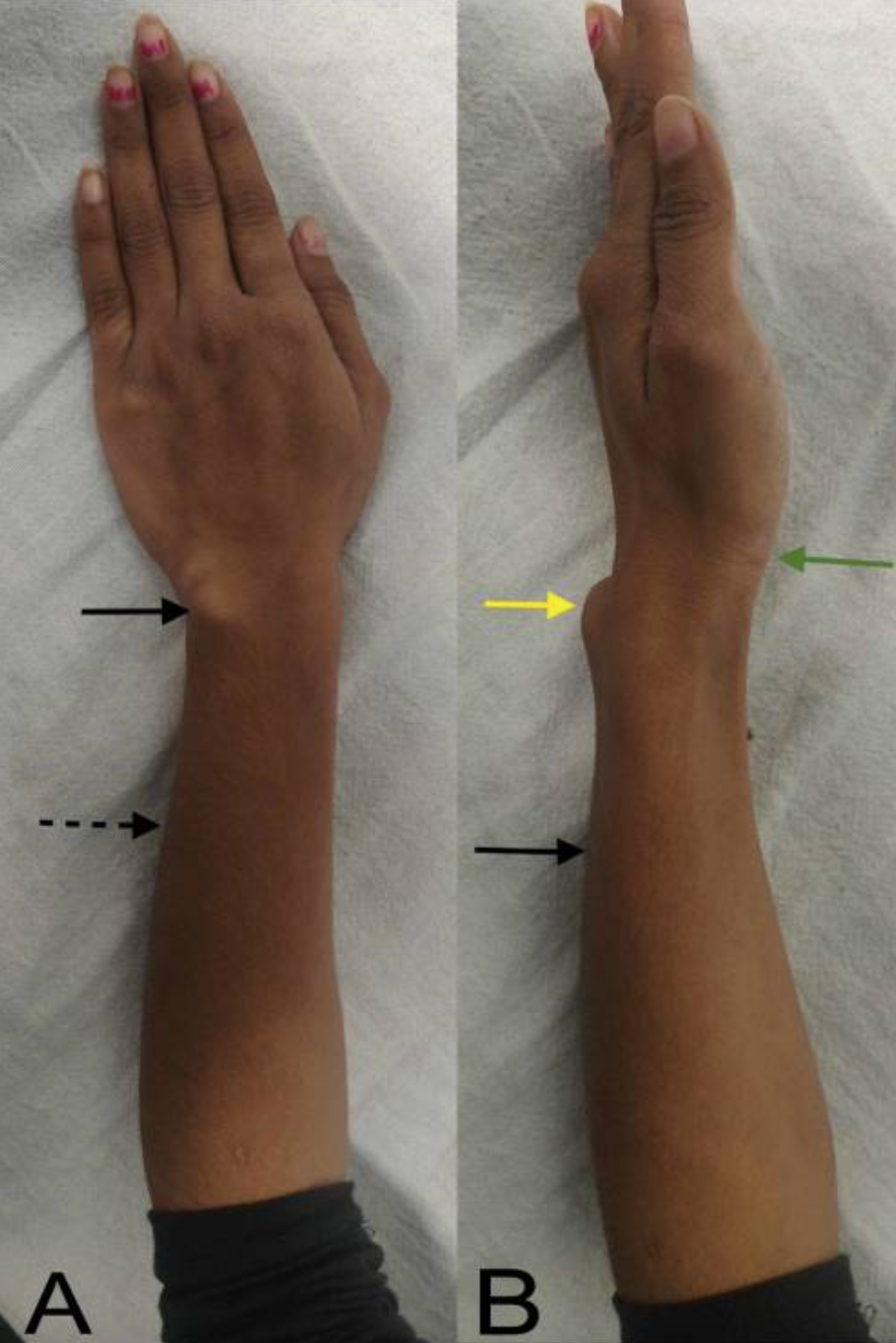
Madelung deformity is a distal radius condition producing a deficiency in the volar ulnar corner that frequently causes wrist pain and cosmetic deformity (see Image. Left Madelung Deformity). The proposed mechanism of the classic congenital form of this deformity involves the anomalous development of the Vickers ligament, restricting distal radial growth in the volar ulnar area.[1]
Various options are available for treating this condition, which is determined based on the severity, symptoms, and the patient's skeletal maturity at the time of diagnosis. Surgical procedures for correcting Madelung deformity can be divided into radial lengthening, ulnar shortening, or a combination of both. Wrist pain is the primary indication for surgical intervention in most patients with this condition.[2]
Etiology
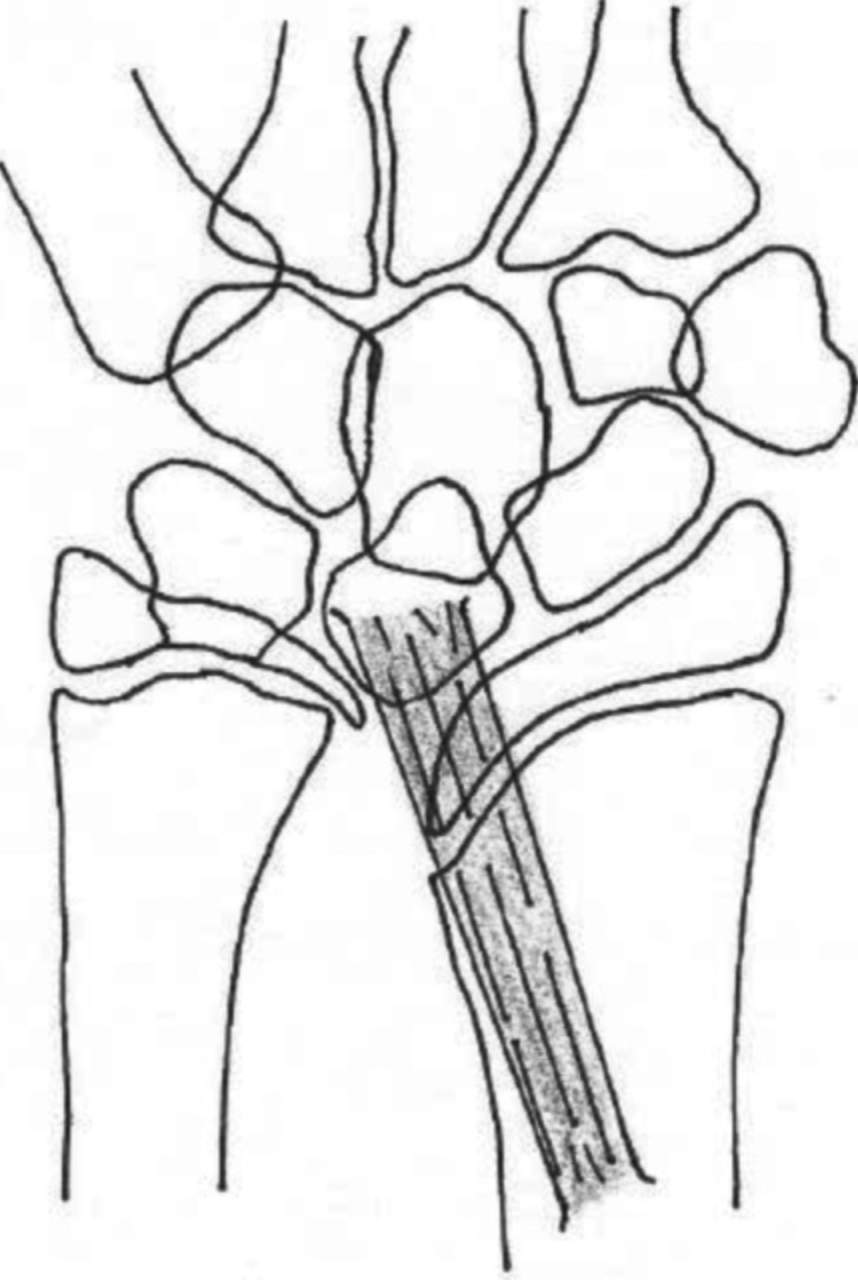
Madelung deformity arises from developmental or traumatic origins. The exact cause of the classic or congenital form is unclear. However, it is thought to be due to a shortened and thickened radiolunate or radiotriquetral ligament, forming the anomalous Vickers ligament (see Image. Vickers ligament). This structure originates from the radial metaphysis rather than the epiphysis, thereby tethering and restricting the growth of the distal radial volar-ulnar physis. A retrospective study revealed that an anomalous radiotriquetral ligament is a constant and distinguishing finding in classic Madelung deformity.[3][4][5]
The aberrant bone growth increases radial inclination and volar tilt, causing lunate subsidence and altering carpal kinematics. A biomechanical study of wrists with a Madelung deformity using 4-dimensional CT imaging reported that the mobility of the lunate and triquetrum bones is reduced in Madelung deformity.[6] Leri-Weill dyschondrosis is a form of mesomelic dwarfism presenting with the triad of Madelung deformity, short stature, and mesomelic disproportion (upper and lower limbs are shortened medially). This syndrome is associated with short-stature homeobox-containing gene (SHOX) mutation.[7] Madelung deformity is also common in patients with Turner syndrome.[8]
A Madelung-like deformity may arise from damage to the volar ulnar distal radius physis. One example is gymnast's wrist, which forms from repetitive microtrauma to the distal radial physis. Other conditions presenting with Madelung-like deformities include traumatic injuries, multiple hereditary exostoses, and Ollier disease. The presence of the Vickers ligament differentiates true Madelung deformity from Madelung-like conditions.
Epidemiology
Madelung deformity is 4 times more common in women than men. The classic congenital form is mostly associated with Leri-Weill dyschondrosis, presenting bilaterally and symmetrically in patients with this syndrome.
The age of diagnosis of Madelung deformity is typically between 8 and 14 years. The deformity increases with growth due to growth-plate tethering in young bones, then remains stable at skeletal maturity. Pediatric hand deformities occur in 1 to 2% of the general population.
Madelung deformity is relatively rare, comprising less than 2% of pediatric hand deformities. This condition has a prevalence of 0.03% in the general population.[9] Less than 10% of patients with Turner syndrome have Madelung deformity.
History and Physical
Individuals with classic Madelung deformity typically present at age 8 years or older. Meanwhile, traumatic Madelung-like deformities may arise at any age. Patients with the congenital type may have family members with the same condition. These individuals often consult primarily due to cosmetic instead of functional limitations. However, wrist pain, decreased grip strength, and progressive wrist range-of-motion loss may be present in these individuals. Wrist pain may be radial or ulnar and is more common when weight-bearing on an extended wrist. Limited wrist extension is typically due to the ulnar head's dorsal displacement, though this does not commonly restrict forearm rotation.
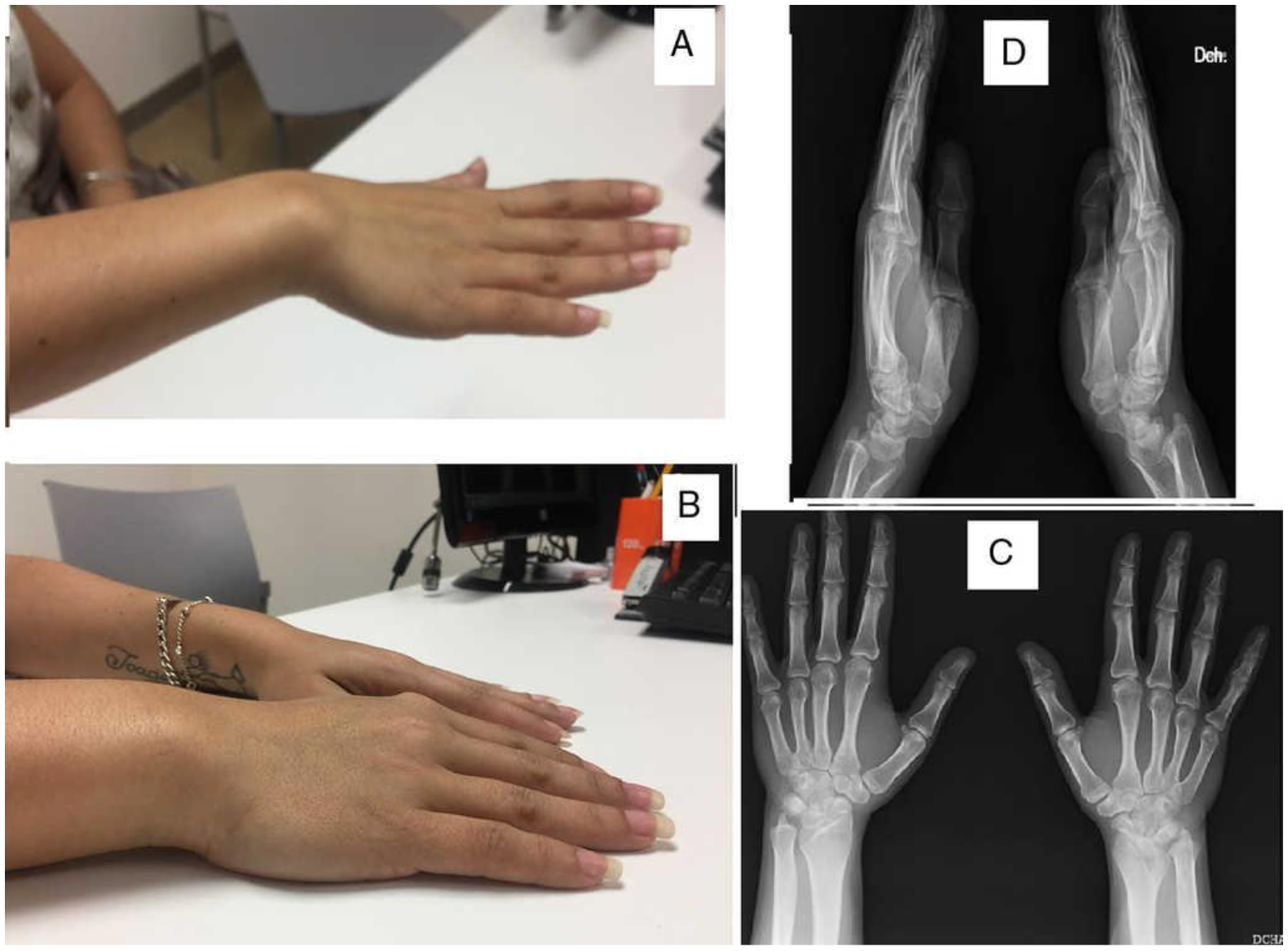
The distal ulna is dorsally prominent at the wrist due to greater ulnar than radial growth (see Image. Right Madelung Deformity). Madelung deformity variants may also involve the entire radius or present with a radius more prominent than the ulna (reverse Madelung deformity). Involvement of the entire radius is often associated with Leri-Weill dyschondrosis, presenting with radial bowing and severe deformity (see Image. Radial Bowing in Madelung Deformity). The reverse Madelung deformity results in dorsal carpal subluxation.[8]
Evaluation
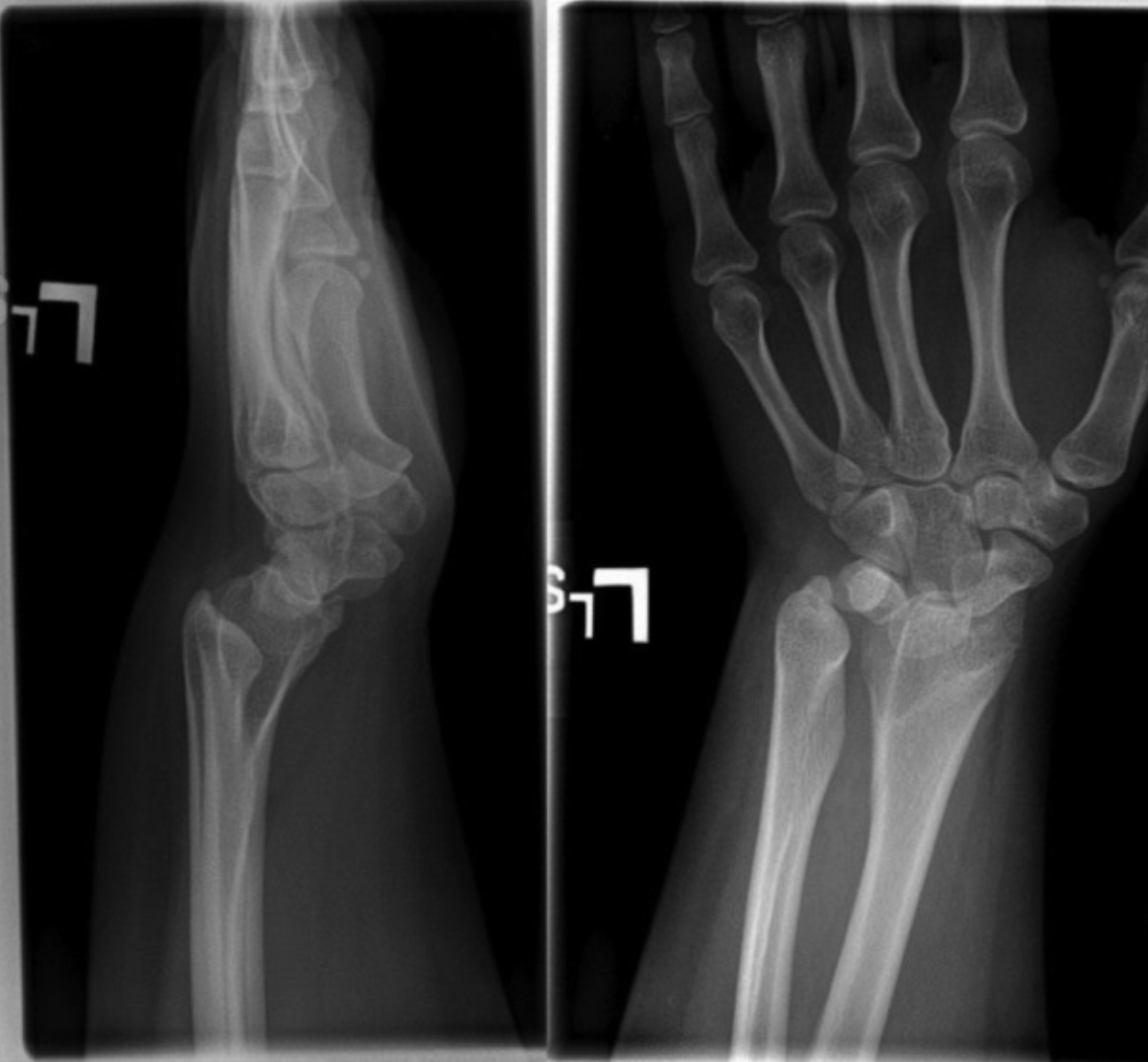
Madelung deformity workup may start with wrist and forearm radiography (see Image. Madelung Deformity Lateral and Anteroposterior Radiographs). Anteroposterior (AP) radiographs may show increased radial inclination, lunate subsidence into the lunate fossa, and a characteristic V-shaped carpus. On lateral radiographs, increased volar tilt and a relative volar carpal subluxation may be observed. Dorsal ulnar displacement may be seen on X-ray due to the increased distal volar radial tilt. The distal ulna may appear spiculated and irregular if the deformity is severe and long-standing.
The distal radioulnar joint commonly remains reduced in classic Madelung deformity involving the entire radius. Consequently, forearm and elbow radiographs may demonstrate the radial head pulling away from the capitellum, with the radiocapitellar distance increased by more than 4 mm. Radial bowing may also be present on forearm radiographs.
Various radiographic thresholds have been reported to detect Madelung deformity accurately. These thresholds include a minimum of 33° of ulnar tilt, 4 mm lunate subsidence, at least 20 mm of palmar carpal displacement, and a lunate fossa angle of at least 40°.[10]
Wrist MRI is not routinely recommended in Madelung deformity, although it is the best imaging modality to identify the Vickers ligament. The MRI can identify this ligament in approximately 85% of cases.[11] This modality is not recommended for routine screening in patients with a strong family history of Madelung deformity, even for prophylactic treatment.[12]
The MRI may also identify an oblique triangulofibrocartilage complex as the deformity worsens. There may be a bony physeal bar across the volar ulnar physis, although this may also appear on radiographs.[13]
X-rays and MRI may reveal a flame-shaped distal radial notch at the origin of the Vickers ligament, which is pathognomonic for Madelung deformity, and a distal radial metaphyseal flare. Acquired Madelung deformity will not demonstrate the Vickers ligament on MRI, although paraphyseal edema and physeal bridging may appear in traumatic cases.
A retrospective multicenter study found that the Vickers ligament was present in 83% of patients with Madelung deformity intraoperatively, which nearly equals the 85% MRI detection rate for this structure. Additionally, the presence of a whole-radial-bone Madelung deformity type and a distal radial notch were found to be important predictors for the presence of the Vickers ligament.[11]
Treatment / Management
Treatment of Madelung deformity depends on the severity and cause of the deformity and the timing of diagnosis. In patients with no to mild symptoms, conservative management often suffices. Conservative management consists of oral nonsteroidal anti-inflammatory drugs, activity modification, and wrist splinting.[14]
Patients undergoing conservative treatment must be evaluated with serial radiographs every 6 months until skeletal maturity. If the deformity continues to worsen in a skeletally immature patient, prophylactic surgery may be performed to prevent further progression. However, the timing of the intervention remains controversial.
Several techniques are available for the surgical correction of symptomatic Madelung deformity. The first is Vickers ligament resections performed in skeletally immature patients with congenital Madelung deformity. Physeal bar excision with adipose tissue interposition may be performed if a physeal bar with remaining growth potential is present. Some reports suggest waiting for any intervention until skeletal maturity if the deformity is insignificant, as most pain symptoms may resolve with time.[15]
A classic treatment of Madelung deformity in skeletally immature patients is the Langenskiold procedure, where the radial physis is ablated (radial epiphysiodesis), the Vickers ligament is resected, and fat is interposed on the area.
Gradual correction by guided growth combined with a distal ulnar or radial epiphysiodesis evens the distal radio-ulnar joint. A dome osteotomy may allow for deformity correction in multiple planes in a skeletally mature patient. Ulnar shortening osteotomy or ulnar head resection (Darrach procedure) may correct a symptomatic, prominent ulnar head.
Distal radioulnar joint arthroplasty is not widely studied as a treatment option.[16] Carvalho et al reported that distal radial-dome osteotomy and Vickers ligament resection results in good functional outcomes in patients with Madelung deformity.[17] Isolated or combined radioulnar osteotomy performed in individuals with this condition had been found to produce satisfactory clinical and radiographic results after a mean follow-up of 8.1 years.[18]
Madelung deformity remains a surgical challenge, as it requires multiplanar correction. However, developing customized osteotomy cutting guides may enhance surgical outcomes. Recently, Kodama et al reported that the preoperative simulation of combined radial and ulnar osteotomies accurately corrected Madelung deformity.[19] A retrospective study by Bachy et al reported that 3-dimensional planning helps in predictable deformity correction across most, but not all, outcome parameters.[20]
Differential Diagnosis
The differential diagnosis for wrist pain with loss of range of motion includes the following:
- Fracture
- Arthritis
- Tendinopathy
- Tumors
The Madelung-type deformity may arise from trauma or tumors. This condition must be distinguished from a true Madelung deformity, which is managed differently and has a dissimilar natural history.
Prognosis
The natural history of Madelung deformity is variable and poorly understood. This condition is likely to progress throughout adolescence until skeletal maturity is reached. Most patients obtain some degree of pain relief after Vickers ligament release and volar dome osteotomy, although some may require a secondary ulnar shortening osteotomy.[21]
Vickers ligament release combined with dome osteotomy has been shown to provide radiographic improvement of Madelung deformity.[22] Due to the rare nature of this condition and the wide range of treatment options, treatment results are poorly understood, as large-scale, long-term follow-up studies are lacking.
Complications
Patients with severe deformities who do not undergo surgery have a higher risk of extensor tendon attritional rupture with increasing deformity duration. The ulnar extensors are more commonly involved. Wrist pain may persist with or without surgical intervention due to ulnar impaction. Wrist arthritis may also develop in neglected Madelung deformity.[23]
Postoperative and Rehabilitation Care
A short-arm orthosis is recommended for 3 to 4 weeks after a Vickers ligament release and physeal bar excision, followed by progressive range-of-motion and weight-bearing exercises. Meanwhile, ulnar shortening and dome osteotomy require 2 weeks of long-arm immobilization followed by 4 weeks of short-arm immobilization. After 6 weeks of immobilization, active range-of-motion exercises are allowed, with progression to weight-bearing in the 3rd month after surgery.
Consultations
A genetics consultation is warranted if an associated genetic syndrome, such as Leri-Weill dyschondrosis, Turner syndrome, and multiple hereditary exostoses, is suspected to cause a Madelung deformity. Additionally, a referral to an adult or pediatric hand surgeon may be necessary due to the rarity of this condition.
Deterrence and Patient Education
Madelung deformity is a rare, congenital condition. Preventing its occurrence is challenging due to the lack of well-established anticipatory measures. Nevertheless, several actions can help reduce the impact of this condition. First is genetic counseling. Geneticists and genetic counselors can provide information about the condition, assess familial risks, and offer guidance on potential genetic testing or family planning considerations.
Second is regular pediatric care. The pediatrician can help monitor changes in the patient's musculoskeletal system. Early identification of bone development or wrist structure abnormalities can prompt appropriate medical attention and management. Third is ensuring proper nutrition and overall health. Vitamin deficiencies can precipitate or aggravate abnormal musculoskeletal development.
Meanwhile, patients predisposed to Madelung-type deformities may be advised to avoid repetitive wrist stress or trauma during childhood and adolescence and condition the body properly when engaging in sports activities.
While these measures may help prevent the occurrence of the condition, evidence that supports their effectiveness is limited due to the condition's complexity and rarity.
Enhancing Healthcare Team Outcomes
Madelung deformity is relatively rare and thus may not always be encountered in general medical training. Patients may present first to a primary care provider or directly to a hand or orthopedic surgeon for evaluation. Therefore, pediatricians and primary care providers must be aware of this progressive genetic condition.
Referral to the appropriate surgeon for evaluation is necessary to reduce treatment delays. Genetic counseling may be necessary and should be discussed with the patient and their family. The radiologist's role is crucial in radiographic and MRI diagnosis, particularly in mild cases.
Physical and occupational therapists are paramount in nonoperative and postoperative management. Interprofessional management of patients with Madelung deformity allows for improved patient outcomes.[24]