[1]
Ojumah N, Ramdhan RC, Wilson C, Loukas M, Oskouian RJ, Tubbs RS. Neurological Neonatal Birth Injuries: A Literature Review. Cureus. 2017 Dec 12:9(12):e1938. doi: 10.7759/cureus.1938. Epub 2017 Dec 12
[PubMed PMID: 29464145]
[2]
Abbas RA, Qadi YH, Bukhari R, Shams T. Maternal and Neonatal Complications Resulting From Vacuum-Assisted and Normal Vaginal Deliveries. Cureus. 2021 May 11:13(5):e14962. doi: 10.7759/cureus.14962. Epub 2021 May 11
[PubMed PMID: 34123659]
[3]
Ali UA, Norwitz ER. Vacuum-assisted vaginal delivery. Reviews in obstetrics & gynecology. 2009 Winter:2(1):5-17
[PubMed PMID: 19399290]
[4]
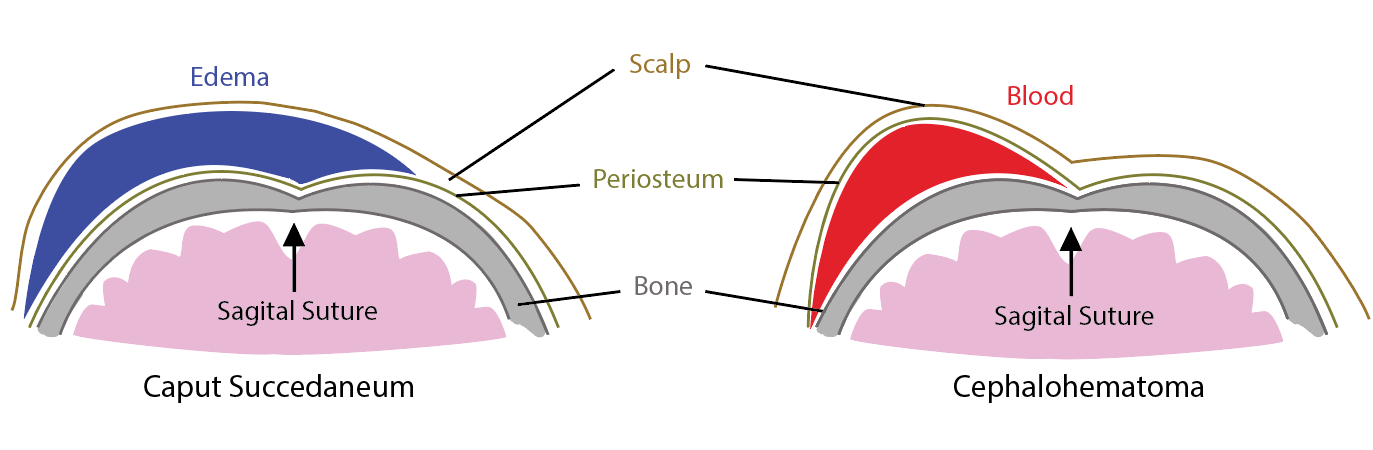
Nicholson L. Caput succedaneum and cephalohematoma: the cs that leave bumps on the head. Neonatal network : NN. 2007 Sep-Oct:26(5):277-81
[PubMed PMID: 17926657]
[5]
Gilboa Y, Kivilevitch Z, Kedem A, Spira M, Borkowski T, Moran O, Katorza E, Achiron R. Caput succedaneum thickness in prolonged second stage of labour: a clinical evaluation. The Australian & New Zealand journal of obstetrics & gynaecology. 2013 Oct:53(5):459-63. doi: 10.1111/ajo.12104. Epub 2013 Jun 26
[PubMed PMID: 23802621]
[6]
Usman S, Wilkinson M, Barton H, Lees CC. The feasibility and accuracy of ultrasound assessment in the labor room. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians. 2019 Oct:32(20):3442-3451. doi: 10.1080/14767058.2018.1465553. Epub 2018 Apr 30
[PubMed PMID: 29712501]
Level 2 (mid-level) evidence
[7]
Hassan WA, Eggebo TM, Salvesen KA, Lindtjorn E, Lees C. Intrapartum assessment of caput succedaneum by transperineal ultrasound: a two-centre pilot study. The Australian & New Zealand journal of obstetrics & gynaecology. 2015 Aug:55(4):401-3. doi: 10.1111/ajo.12342. Epub 2015 Jul 23
[PubMed PMID: 26201530]
Level 3 (low-level) evidence
[8]
Shah NA, Wusthoff CJ. Intracranial Hemorrhage in the Neonate. Neonatal network : NN. 2016:35(2):67-71. doi: 10.1891/0730-0832.35.2.67. Epub
[PubMed PMID: 27052980]
[9]
Levin G, Mankuta D, Eventov-Friedman S, Ezra Y, Koren A, Yagel S, Rottenstreich A. Factors associated with the severity of neonatal subgaleal haemorrhage following vacuum assisted delivery. European journal of obstetrics, gynecology, and reproductive biology. 2020 Feb:245():205-209. doi: 10.1016/j.ejogrb.2019.12.012. Epub 2019 Dec 28
[PubMed PMID: 31902544]
[10]
Colditz MJ, Lai MM, Cartwright DW, Colditz PB. Subgaleal haemorrhage in the newborn: A call for early diagnosis and aggressive management. Journal of paediatrics and child health. 2015 Feb:51(2):140-6. doi: 10.1111/jpc.12698. Epub 2014 Aug 11
[PubMed PMID: 25109786]
[11]
Shekhar S, Rana N, Jaswal RS. A prospective randomized study comparing maternal and fetal effects of forceps delivery and vacuum extraction. Journal of obstetrics and gynaecology of India. 2013 Apr:63(2):116-9. doi: 10.1007/s13224-012-0282-1. Epub 2012 Aug 28
[PubMed PMID: 24431617]
Level 1 (high-level) evidence
[12]
Jayawant S, Parr J. Outcome following subdural haemorrhages in infancy. Archives of disease in childhood. 2007 Apr:92(4):343-7
[PubMed PMID: 17376941]
[13]
Lykoudis EG, Spyropoulou GA, Lavasidis LG, Paschopoulos ME, Paraskevaidis EA. Alopecia associated with birth injury. Obstetrics and gynecology. 2007 Aug:110(2 Pt 2):487-90
[PubMed PMID: 17666638]
[14]
Martín JM, Jordá E, Alonso V, Villalón G, Montesinos E. Halo scalp ring in a premature newborn and review of the literature. Pediatric dermatology. 2009 Nov-Dec:26(6):706-8. doi: 10.1111/j.1525-1470.2009.01017.x. Epub
[PubMed PMID: 20199445]