Continuing Education Activity
Pythium is a parasitic aquatic oomycete that causes vision-threatening keratitis. Clinically, morphologically and histopathologically, it closely mimics fungal keratitis. Prompt diagnosis, meticulous management, and regular follow-up are vital to get a good outcome. This activity describes the etiology, risk factors, clinical features, investigations, treatment options, differential diagnosis, and complications of Pythium keratitis.
Objectives:
- Describe the clinical features that distinguish Pythium from fungal keratitis.
- Outline the evaluation of Pythium keratitis.
- Explain the appropriate microbiological investigations in a suspected case of Pythium keratitis.
- Review the management options available for the interprofessional team to treat Pythium keratitis.
Introduction
Pythium is a parasitic aquatic oomycete belonging to phylum Straminipila, order Pythiales, class oomycetes, and family Pythiaceae. It closely resembles fungal keratitis hence also labeled as “parafungus” or “fungus-like organism.”[1] The first case of systemic Pythiosis was reported way back in 1884 by British veterinarians.[2]
It is known to infect animals and humans, where it causes systemic and ocular infections. The organism is usually seen in aquatic habitats with a high prevalence in tropical, subtropical, and temperate conditions. It is more common in males, particularly field workers.[3] The clinical features closely resemble fungal keratitis like dry-looking stromal infiltrate, feathery margins, satellite lesions, endothelial plaque, hypopyon, and corneal perforation.[1]
The morphological and microbiological profile also closely mimics fungus. Hence the organism is usually diagnosed by zoospore formation on culture media. The medical management options available are antifungals, antibacterials, and cyanoacrylate glue.[2][3][4] The antibacterials in the form of linezolid and azithromycin have shown higher in-vitro efficacy against the organism. Hence they are considered first-line drugs for Pythium keratitis. Hence, antibacterials are the drug of choice in today’s era.[3]
Early therapeutic keratoplasty is warranted in non-resolving progressive cases.[2] Due to rapid proliferation, high virulence, lack of diagnostic modalities at all centers, limited efficacy of the currently available medications, and higher recurrence rates, it is still a diagnostic dilemma and management challenge for many ophthalmologists.
Etiology
Pythium belongs to the genus of parasitic oomycetes.[5] Earlier, they were classified as fungi. The majority of species are plant parasites, but Pythium insidiosum is an important pathogen in humans and animals, causing ocular and systemic pythiosis. More than 120 species of Pythium have been reported worldwide. Pythium insidiosum causes sight-threatening keratitis in humans. The various forms of Pythium reported in humans are ocular, cutaneous/subcutaneous, vascular, and disseminated. The systemic involvement is reported in the form of ulcerative lesions and granulomas over the skin, face, limbs, and subcutaneous tissues. The vascular manifestation includes aneurysm, thrombosis, and vasculitis.[6] The various systemic associations include
- Thalassemia/hemoglobinopathy syndrome
- Paroxysmal nocturnal hemoglobinuria (PNH)
- Aplastic anemia
- Chronic arterial insufficiency syndrome
- Cavernous sinus thrombophlebitis
The majority of the previous studies have reported risk factors in the form of mud or grass injury, soil injury, clay injury, stick injury in the eye, and occupations requiring work in aquatic fields.[1]
Epidemiology
The first case of systemic pythiosis was reported way back in 1884 by British veterinarians in horses. However, sight-threatening ocular infection in the form of keratitis has been primarily reported from Thailand, the United States of America, China, Israel, Australia, and India.[5][7][8][9][10]
The first case of systemic pythiosis in a human was reported in Thailand in 1985.[11] However, the first case of Pythium keratitis was reported in 1988, and since then, large-scale studies from all over the globe. In animals, it occurs in tropical, subtropical, and temperate climates, and cases have been reported from Australia, Argentina, Brazil, Costa Rica, India, and Indonesia.[6] Studies quoting the incidence and prevalence of Pythium keratitis are scarce in literature due to the rarity of the organism. Pythium exists in all age groups with a higher incidence in students and software professionals.[1] In the elderly age group, the majority are males and outdoor workers.
Pathophysiology
Austwick and Copland stimulated the production of zoospore and proposed that zoospore plays an important role in pathogenesis.[12] Mendoza et al., in their analysis, showed that zoospore had a special inclination towards animal wounds, hairs, damaged skin, and mucosa of the intestine.[13]
These zoospores encyst on wounded tissues and secrete glycoproteins which facilitate adhesion on the surface. The host body temperature further acts as a stimulus for these zoospores. As a result, hyphae are formed, which extend on the infected tissue and penetrate the blood vessels. The high incidence of Pythium keratitis in thalassemia patients is probably due to iron overload, and hemochromatosis can be another major predisposing factor. The phagocytic action of TNF-a, IFN-c, macrophages, and neutrophil production is also inhibited due to iron overload.
Udnaen et al. showed that IFN-c production is lowered by monocytes and macrophages in these patients in response to zoospore exposure. This indicates that T helper 1 (Th1) cell response is inhibited, which is responsible for the increased susceptibility of infection in these patients. It has also been postulated that Pythium induces T helper 2 (Th2) cells, and antigen immunotherapy stimulates the immune modulation from Th 2 to Th1 response, which is thought to be curative in thalassemia patients. Another hypothesis is that Pythium has a gene encoding ferrochelatase which is thought to be responsible for high virulence in these patients.[14]
Histopathology
There are a variety of histopathological diagnostic techniques available for Pythium insidiosum keratitis. On 10% KOH wet mount and Gram stain, it is seen as slender long septate or aseptate hyaline hyphae with perpendicular lateral branches which mimic the hyphae of fungi. Hence they are difficult to diagnose on wet mount alone. But in contrast, numerous vesicles are often present in the hyphae of the Pythium.
On blood agar and sabouraud dextrose agar flat, feathery colonies are observed along with zoospore formation. The zoospore presence is confirmed on culture by the leaf incarnation method. Another method of identifying hyphae is staining by iodine potassium iodide (IKI) and sulfuric acid stain (IKI-H2SO4). The Pythium hyphae change color to blue/ bluish-black, which is labeled as positive, and yellow/ yellowish brown is reported as negative. Additionally, trypan blue has also been a useful indicator in the early identification of aseptate and septate hyphae of Pythium, especially in a rural setup where other diagnostic modalities are scarce.
The next method of identification is the use of periodic acid-Schiff (PAS). The slides of Pythium can be treated with 0.5% and 1% periodic acid for 0.5, 2, 3, and 5 minutes and Schiff’s reagent can be used without modification for 10 minutes. When the filaments turn pink, it is considered positive staining, and when it doesn’t stain, it is labeled as negative. The filaments of Pythium also appear pale pinkish to ghost-like structures on hematoxylin & eosin (H&E) stains. On Gomori methamine silver (GMS) stain, Pythium filament appears brown, and the stroma turns greenish. These filaments on GMS appear as septate or aseptate, broad or narrow, long or short, and may or may not have obtuse to perpendicular branching. The intervening filaments may also have swollen hyphae and can also exist in varied morphologies like twisted, folded collapsed, or hollow tubes.[15]
Difference of Staining Between Pythium and Fungus
The filaments of fungi stain with PAS as bright magenta color, but Pythium filaments stain variably from pink to pale magenta or sometimes may not stain. This difference in staining is due to the presence of cellulose in the Pythium cell wall, which gives a weaker acid reaction with pectin and chitin. The duration, as well as concentration of PA, shows a difference in staining.[15]
History and Physical
Patients with Pythium keratitis usually present with a history of pain, redness, photophobia, blurring of vision, irritation, watering, and sometimes discharge.[5] There may be an antecedent history of stick injury, mud injury, dust fall, clay injury, or contact lens use.[1][16] In sporadic cases, there is no history of trauma.[1]
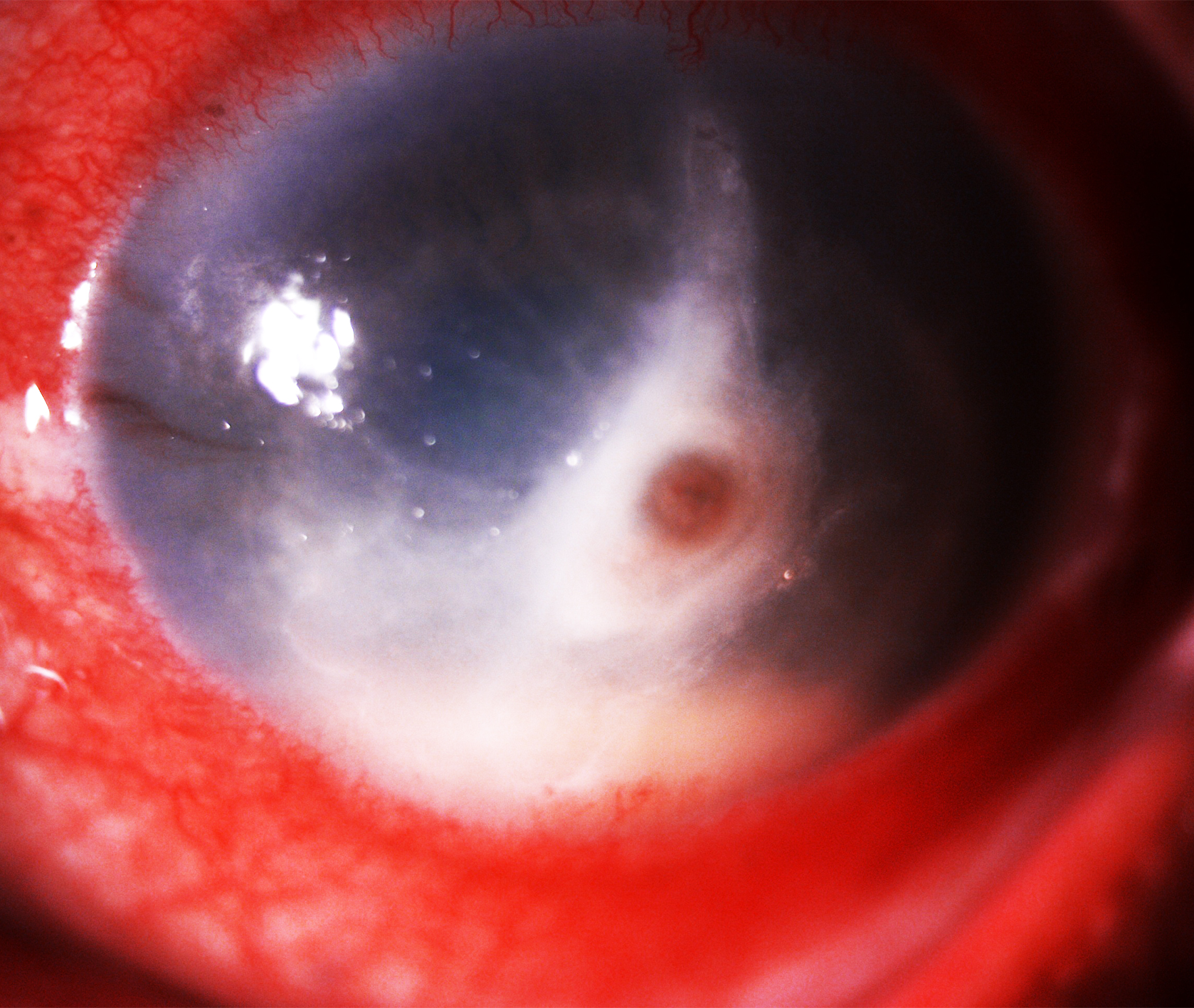
The anterior segment findings are the same as that of the fungal corneal ulcer, including lid edema, blepharospasm, conjunctival congestion, discharge, epithelial defect, stromal infiltrate, feathery margins, satellite lesions, and stromal edema. Other closely mimicking features may include corneal melt, descemetocele, endothelial plaque, hypopyon, anterior chamber exudates, ring infiltrate, Wesseley’s immune ring, and corneal perforation (Figure 1).[17] The classical clinical features which separate Pythium from other infective keratitis are stromal infiltrate with hyphenated edges, multifocal lesion, tentacular projections, peripheral furrowing with thinning, guttering, and an early tendency to spread towards the limbus.[1][7]
The rare clinical features which resemble Acanthamoeba keratitis are radial keratoneuritis with stromal infiltrates.[18] This usually occurs in mixed infection with Acanthamoeba and Pythium infection, particularly with a history of contact lens use. A few clinical features can also mimic atypical Mycobacteria in the form of epithelial breach, greyish white stromal infiltrate, which is dry looking, cracked windshield appearance of the infiltrates, stromal edema, and Descemet membrane folds.[19]
Evaluation
Laboratory evaluation of Pythium keratitis begins with appropriate sample collection. The samples are collected in the form of corneal scrapings under 5% proparacaine topical anesthesia with either Kimura spatula, number 15 Bard-Parker blade, 26 gauge needle, hypodermic needle, or platinum spatula. The corneal scrapings are subjected to wet mount direct microscopic examination using 10% potassium hydroxide (KOH), potassium calcofluor white, and Gram stain.[2]
The septate or aseptate hyphae with perpendicular or obtuse lateral branching are seen. The scraping material is also used for culture analysis using blood agar, chocolate agar, Sabourad dextrose agar, or any nutritional agar where Pythium appears as white-colored creamy colonies along with zoospore formation. The zoospore also contains numerous vesicles.[1] Further, the zoospore growth is confirmed using the leaf incarnation method. The histopathological analysis is assisted using iodine potassium iodide (IKI) and sulfuric acid stain (IKI-H2SO4), H&E, PAS stains, or Gomori methenamine silver (GMS) stain.[15]
The serological analysis of P. insidiosum is based on antibodies detection in serum. The various tests are immunodiffusion, hemagglutination, immunochromatography, enzyme-linked immunosorbent assay (ELISA), and western blot. The reported sensitivity of immunodiffusion is 61%.[20][21][22] In contrast, the reported sensitivity and specificity of ELISA is 100%.[23]
The molecular diagnostic method for Pythium is polymerase chain reaction (PCR), based on the amplification of the internal transcribed spacer (ITS) region, ribosomal intergenic spacer region (IGS), and gene cytochrome oxidase (COX2).[24] This can pick Pythium species as isolated or from clinical specimens also. The PCR helps in the rapid diagnosis of Pythium by DNA sequencing. Another non-invasive diagnostic technique to diagnose Pythium is in-vivo confocal microscopy (IVCM). The Pythium hyphae appear as beaded branching hyperreflective structures or long slender, thin hyperreflective lines, which vary from 90 to 400 mm lengthwise and 1.5 to 7.5 mm in diameter. The branching angle of Pythium hyphae is reported to be 78.6 degrees.[25] Ultrasound B scan is useful in diagnosing retinal detachment, choroidal detachment, vitritis, and endophthalmitis post-therapeutic keratoplasty.[19]
Treatment / Management
Medical Treatment
Earlier, Pythium was grouped as fungal species; hence antifungals in the form of 5% natamycin suspension hourly, 1% voriconazole, or 1% itraconazole hourly were considered the first line of drugs. Hasika et al., in their analysis, highlighted that existing antifungals have no role in Pythium keratitis management. Since, before culture results, Pythium hyphae closely mimic fungal hyphae, and it is difficult to distinguish them clinically, antifungals still have a role to play in the initial management.[2]
Antibacterials
Currently, the approved medical treatment of choice is topical antibacterials in the form of linezolid, azithromycin, tigecycline, minocycline, tetracycline, doxycycline, mupirocin, clarithromycin, and chloramphenicol. The most commonly used are 0.2% linezolid and 1% azithromycin hourly due to the easy availability and limited toxicity. The dose is tapered based on clinical response. Bagga et al., in their in vitro analysis of culture isolates, proved that antibacterials are superior to antifungals in managing this entity. Continued use of anti-Pythium drug hourly for weeks may result in toxicity and promote corneal thinning. Hence care must be taken to taper the dosage based on clinical response.[3]
Surgical Management
Therapeutic Keratoplasty (TPK)
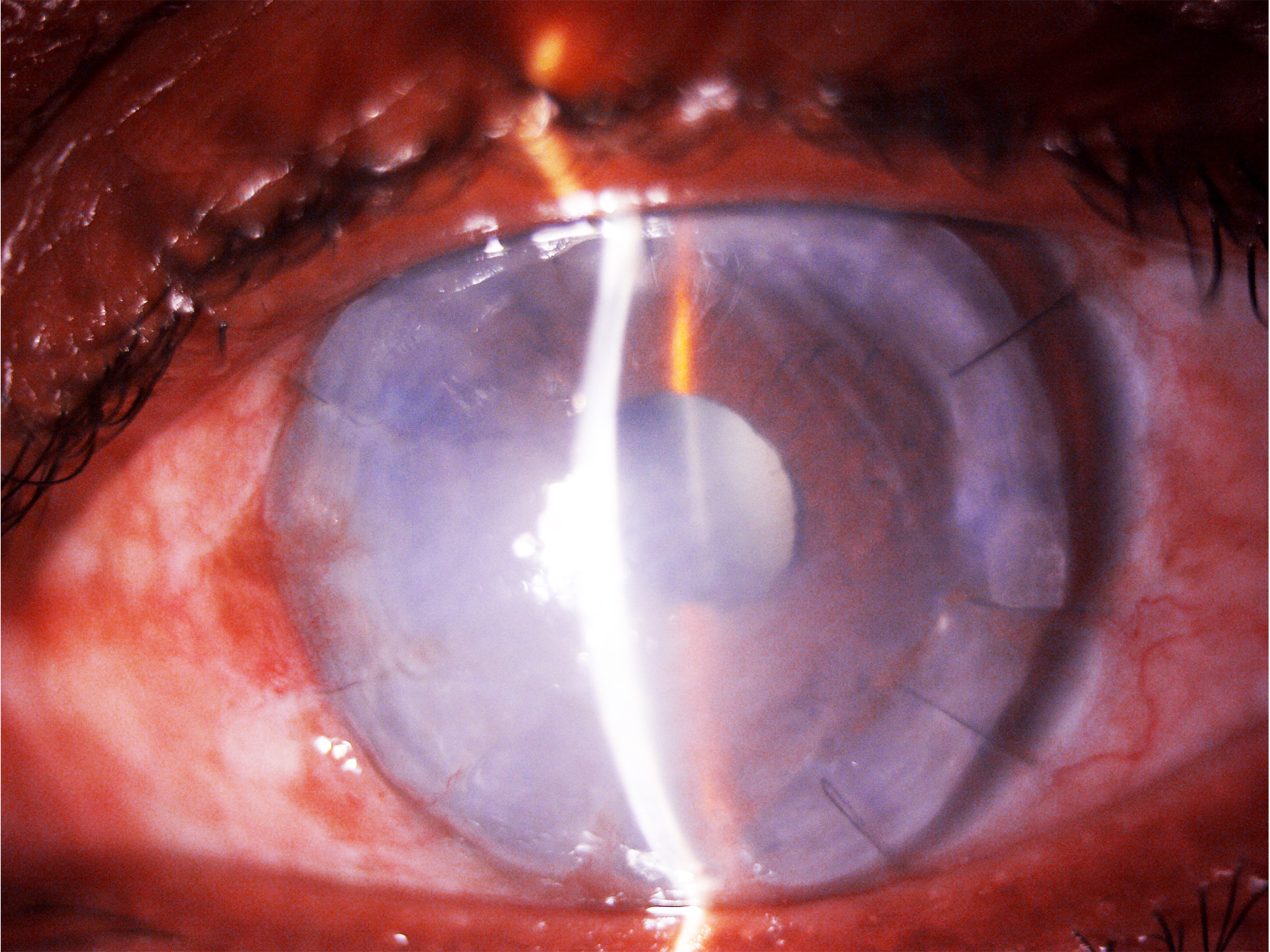
Due to the high virulence, the rapid proliferation of the microorganism, limited response to medical treatment, and high recurrence rate, early TPK is warranted in Pythium keratitis with a good 1 mm margin clearance (Figure 2). Hasika et al., in their retrospective study, showed that therapeutic keratoplasty (TPK) is the mainstay of treatment. The subjects not resolving maximal medical therapy for 10-14 days or developing endophthalmitis, scleritis, descematocoele, or corneal perforation should undergo early TPK.[1][2]
Evisceration and Enucleation
Due to the rapid proliferation, high virulence, and tendency to spread towards the limbus and deeper structures, complications like endophthalmitis and panophthalmitis are not uncommon in Pythium keratitis cases. The patients developing non- resolving endophthalmitis and panophthalmitis should undergo evisceration and enucleation, respectively.[1][3][5]
Other Options
Cryotherapy with Ethanol
Cryotherapy with ethanol as a treatment modality has also been utilized in managing Pythium keratitis. The proposed mechanism for cryotherapy is cellular destruction by ischemic infarction and dehydration and accumulation of toxic concentrates within the cell wall, which further destroys cells. Ethanol acts by decreasing cellular life by increasing cell lysis, reducing proliferation, and promoting apoptosis. Agrawal et al. used cryotherapy in 6 patients of Pythium with involvement of angle structures and sclera. They found that only one patient had a recurrence, thus proving it to be an effective treatment modality.[26]
Cyanoacrylate Glue with Bandage Contact Lens (BCL)
In patients with early stromal melt, descematocoele, and corneal perforation, cyanoacrylate glue, along with BCL, acts as a potential rescuer. Due to its antibacterial properties and linezolid and azithromycin, cyanoacrylate glue has synergistic actions and can prevent vision-threatening devastating sequelae. Gurnani et al., in their case report, highlighted the first case of successful management of pediatric Pythium keratitis using cyanoacrylate glue, azithromycin, and Linezolid with excellent visual outcomes.[4]
Differential Diagnosis
- Fungal keratitis
- Bacterial keratitis
- Atypical Mycobacterial keratitis
- Acanthamoeba keratitis
- Necrotizing viral keratitis
Prognosis
The prognosis depends on the size, depth, extent of the infiltrate, associated complications, the timing of treatment, and follow-up. The patients having early superficial stromal infiltrates not involving the visual axis, if treated promptly with close follow-up, have good visual outcomes. The patients having full thickness infiltrates, corneal perforation, and anterior chamber exudates need early keratoplasty to prevent posterior segment spread of the infection and irreversible sequelae like Phthisis bulbi.
The patients developing endophthalmitis, panophthalmitis, scleritis, choroidal or retinal detachment usually have a guarded prognosis. A good and timely done TPK will help to restore anatomical integrity and early corneal opacification, which can later be managed with optical penetrating keratoplasty for visual restoration.[2]
Complications
- Corneal melt
- Corneal Perforation
- Descematocoele
- Cataract
- Endophthalmitis
- Panophthalmitis
- Choroidal detachment
- Retinal detachment
- Scleritis
- Blindness
- Phthisis bulbi
Postoperative and Rehabilitation Care
After TPK, the patient should be managed initially with hourly topical 0.2% linezolid and 1% azithromycin 6 to 8 times per day and then slowly tapered based on the clinical response. The additional postoperative adjuvant topical drugs include 1% homatropine two times per day to reduce pain due to ciliary spasm, 0.5% timolol eye drops two times per day to prevent secondary glaucoma, and low dose topical antibiotics like 0.5% moxifloxacin or 0.5% gatifloxacin 4 times per day to prevent secondary bacterial infection for at least 2 weeks. If the patient is culture positive for Pythium and postoperatively button culture is also positive for Pythium, steroids can be started after 3 weeks of keratoplasty, making sure there are no residual Pythium hyphae.
Moreover, if the patient is culture-positive and button culture is negative, steroids can be started after 2 weeks of anti-Pythium drugs. The steroids in the form of 0.1% prednisolone or 0.1 % dexamethasone should be started 4 times per day for 2 months and then 3, 2, and 1 time for 3 months each. The steroid dose can be altered based on the clinical response. The vital part of rehabilitation is good postoperative counseling and regular follow-up. The patient should be told about the need for optical penetrating keratoplasty in the future once the eye is free of infection.[1][2]
Consultations
Since Pythium keratitis clinically, morphologically, and histopathologically mimics fungal keratitis, it requires a high index of suspicion and expertise to diagnose this entity. Hence, it is advisable to consult a Cornea and External disease specialist for targeted and meticulous treatment.[3]
Deterrence and Patient Education
The patients must be educated regarding proper hygienic measures to be followed while applying and using contact lens.[16] Agricultural work-related trauma is the major cause of Pythium keratitis. Hence the use of eyeshields and goggles must be emphasized while working in fields.[2] Additionally, the patient must be educated regarding the regular application of medications, follow up and need for early keratoplasty in non-resolving cases.
Pearls and Other Issues
To conclude, Pythium keratitis is a vision-threatening ocular condition which warrants a high index of suspicion to diagnose along with prompt and meticulous management for salvaging the vision. The classical clinical features are tentacular projections, peripheral furrowing, and early limbal spread.
It is difficult to distinguish Pythium hyphae from fungal hyphae on smearing alone. Hence culture is mandatory for zoospore identification. Antibacterials have shown better outcomes than antifungals; hence antibacterials should be resorted to as the first-line drugs. Early keratoplasty is required for good anatomical and functional outcomes.[1]
Enhancing Healthcare Team Outcomes
Any Pythium patient presenting to an emergency department with pain, redness, and photophobia must be urgently referred to an ophthalmologist, preferably a corneal disease expert. Prompt diagnosis and tailored therapy can prevent blindness in these patients.
Smear and culture are mandatory to diagnose Pythium keratitis, and the in-house microbiologist plays a critical role in rapid diagnosis. The patient must be treated with topical 0.2% linezolid and 1% azithromycin as the first-line drugs for at least 2 to 3 months. The ophthalmologist plays a critical role in patient education and counseling regarding general hygiene measured to be followed, meticulous use of contact lenses, and proper medication usage post-infection. Close follow-up is mandatory since the organism is highly virulent and can result in permanent blindness. The nursing team and the pharmacist also play a critical role in patient education.[1][2][5]