Continuing Education Activity
Corneal lacerations are common in ocular trauma. Repair should occur within 24 hours to reduce the risk of infection, alleviate patient discomfort, and avoid further damage to the eye. The goal for repair is a watertight closure, restoration of normal anatomy, and prevention of high astigmatism or scarring. This activity reviews the evaluation and management of corneal lacerations and highlights the role of the interprofessional team in managing this condition.
Objectives:
Identify the initial steps for evaluation when evaluating a patient with an eye injury.
Describe the process for treatment of a corneal laceration.
Review surgical techniques for repairing a corneal laceration.
Summarize the postoperative complications that can occur after a corneal laceration repair.
Introduction
Ocular injury is common, with an estimated 24 million people in the United States suffering an eye injury.[1] Injuries to the eye vary in severity, from a small scratch to the cornea (corneal abrasion) to a split in the external structure (globe rupture). Globe rupture can occur in various parts of the eye; one example is a corneal laceration. In a review of 890 eye injuries in Iraq and Afghanistan from 2001 to 2011, 20.7% involved a corneal laceration.[2]
Corneal lacerations vary in size and shape, can be partial or full-thickness, and range from a simple linear pattern to a complex stellate formation. All lacerations require urgent repair to reduce the risk of infection, decrease tissue necrosis, and alleviate patient discomfort. The typical recommendation for a repair is within 24 hours.[3]
The repair of a corneal laceration often requires suturing; however, tissue adhesives or contact lenses can close lacerations less than 2 mm.[4]
The goal of any repair is a watertight closure, restoration of normal anatomy, and limiting the amount of post-operative corneal scarring and astigmatism.[5][6]
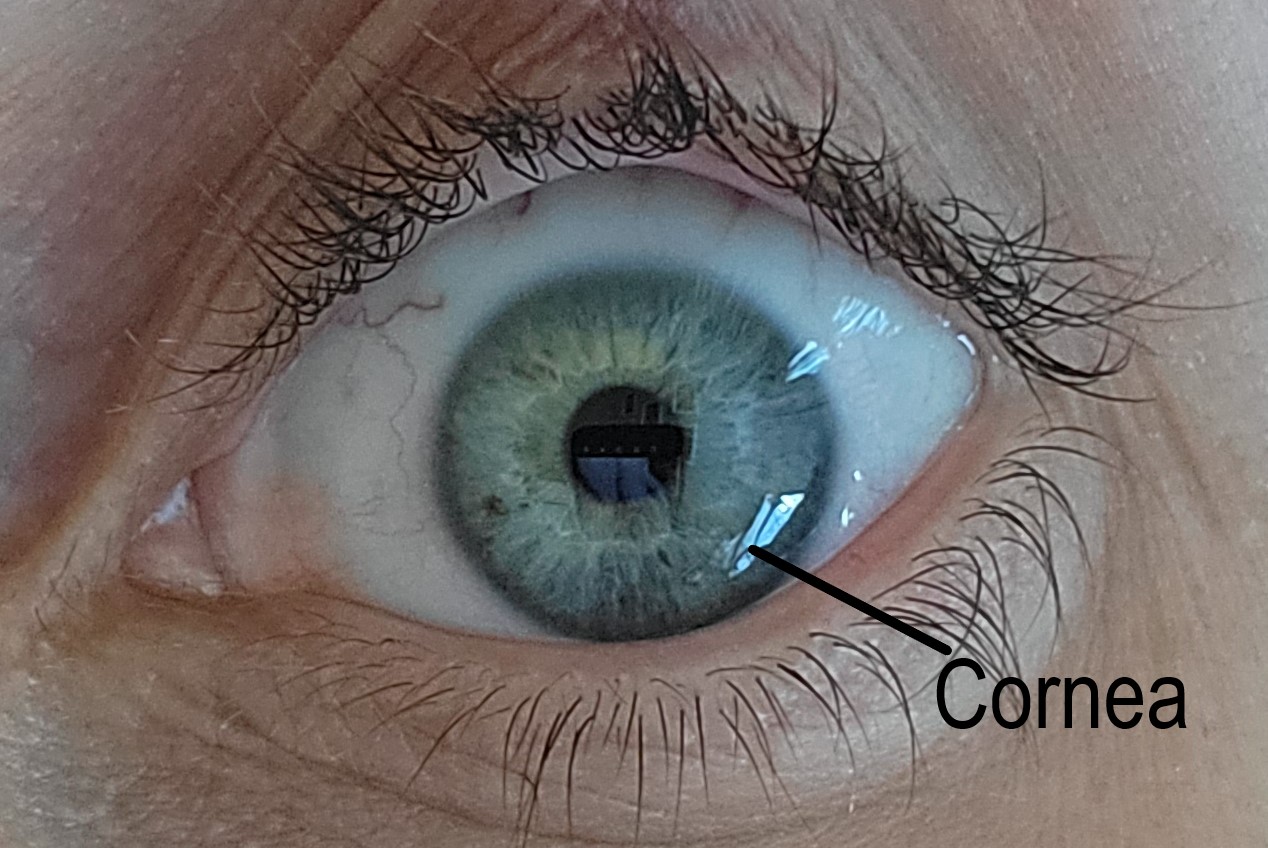
Anatomy and Physiology
A normal human cornea is transparent and avascular. It provides structural support to the eye and acts as a barrier to infections. The average adult cornea is 12 mm horizontally by 11 mm vertically and 0.5 mm in thickness.
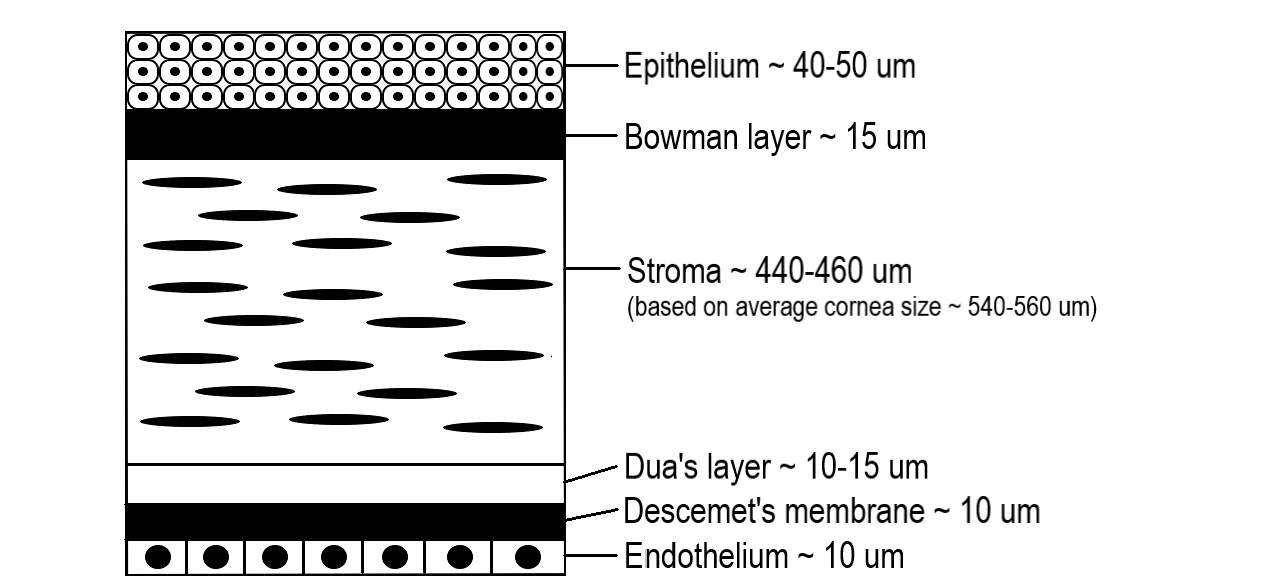
There are five distinct layers of the cornea starting from the outer surface: epithelium, Bowman membrane, stroma, Descemet membrane, and endothelium. In 2013, a 6th layer was reported, called Dua’s layer, situated between the stroma and Descemet membrane. About 80 to 85% of the cornea is the stroma which consists of Type I and V collagen fibers arranged in specific parallel patterns to maintain transparency. The endothelial layer is monocellular and responsible for the optical clarity of the cornea by keeping it dehydrated through a sodium-potassium pump.[7]
The corneal layers have different responses when injured. Injury to the epithelial layer leads to the destruction of the cells and a subsequent defect in the layer. This defect will heal by migrating epithelial cells created at the limbus. About an hour after the injury, the epithelial wound healing starts.[8] Until the defect has healed, the cornea is at significant risk of infection. If the depth of the injury did not violate the Bowman membrane, the cornea heals without scarring.
An injury to the stroma heals with fibrotic deposition, which seals a wound but interferes with normal function. Excess fibrotic tissue repair causes increased scarring and contracture, limiting the optical clarity.
Endothelial cells do not regenerate, and therefore when injured, the cornea may become edematous and cloudy due to the loss of the sodium-potassium pump function of the cells.
The cornea is a highly innervated and sensitive tissue, which receives sensation from the nasociliary branch of the ophthalmic division of the trigeminal nerve.[9] Due to the dense innervation, a patient can feel extreme pain from a corneal injury.
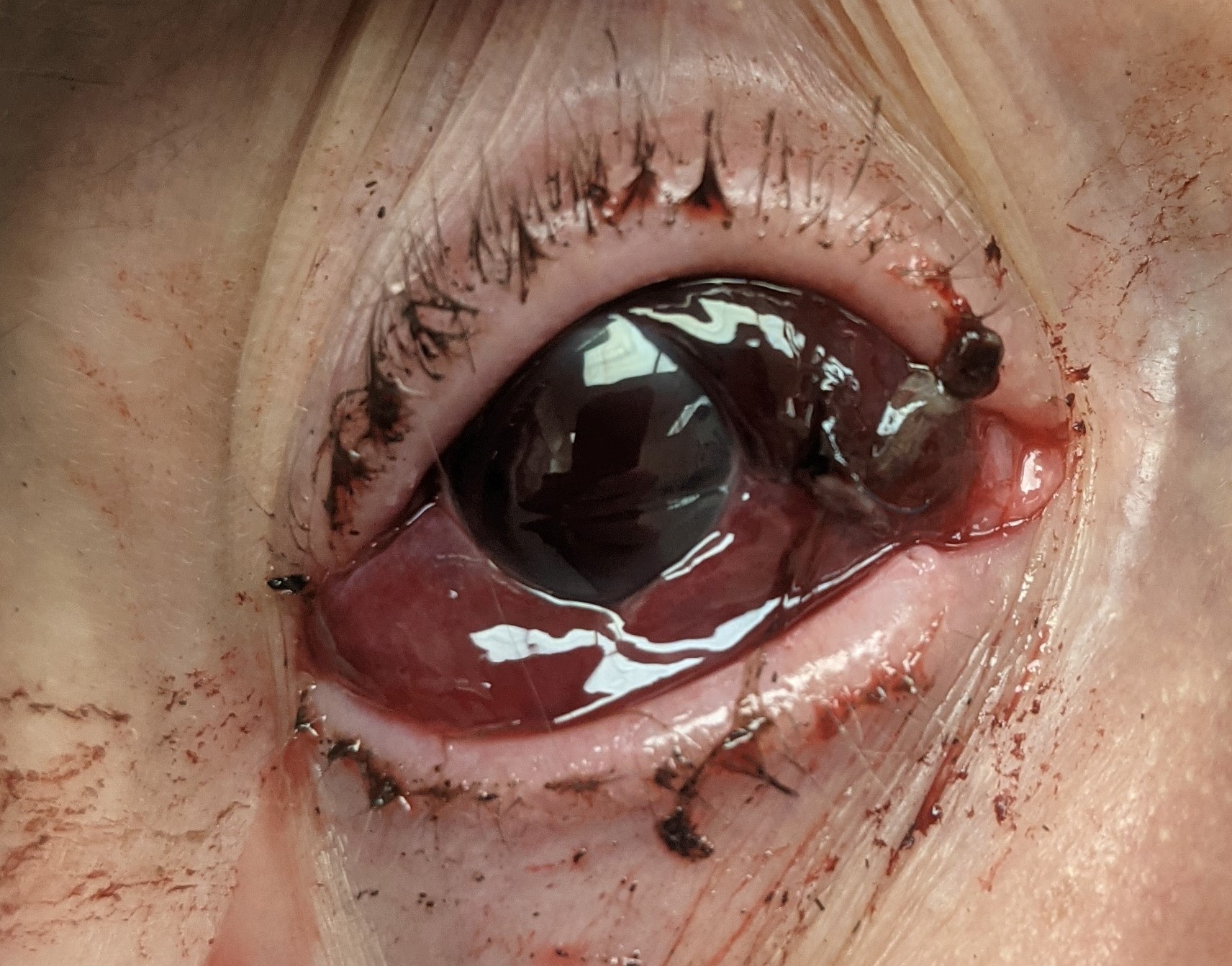
Indications
A diagnosis of corneal laceration by slit-lamp examination is an indication for repair. Signs and symptoms of a corneal laceration after trauma are decreased vision, ocular pain, a positive Seidel test, irregular pupil such as a peaked or teardrop pupil, intraocular foreign body, and prolapse of intraocular contents. If a corneal laceration is suspected, but the view on examination is limited due to an uncooperative patient or eyelid edema, the patient should go to the operating for an exam under anesthesia and globe exploration. A corneal laceration repair should occur urgently to reduce the risks of infection, tissue necrosis, peripheral anterior synechiae formation and alleviate patient discomfort. No specific time for repair is published in the literature, but the standard preferred practice is within 24 hours.
Contraindications
The patient must be hemodynamically stable before the repair. In the setting of polytrauma, the risk of general anesthesia may make a corneal laceration repair unsafe.[10]
Equipment
- Microscope or surgical loupes
- Surgical preparation kit (sponges, 5% povidone-iodine)
- Surgical eye drapes
- Suture: 10-0 nylon (if limbus or scleral involved: 9-0 and 8-0) ** Prime reverse cutting or spatulated needle **
- Eyelid speculum (Jaffe or Schott prevent pressure on the globe) **Eyelid sutures can be an alternative to the speculum **
- Needle holders
- 0.12 forceps (+/- Colibri Forceps)
- Surgical tying forceps
- Tenotomy and fine scissors
- Surgical blade (1.0 to 1.2 mm)
- Ophthalmic viscoelastic
- Balanced salt solution
- 3 mL syringe
- 27 or 30 gauge cannula
- Eye spears
- Cyclodialysis spatula (Used to displace iris from the corneal wound)
- Fluorescein strip
- Cyanoacrylate glue
- Bandage contact lens
- Irradiated corneal tissue or pericardium allograft (Needed if tissue is missing from trauma)
- Rigid eye shield
- Eye pads
- Post-operative antibiotics (intracameral, subconjunctival, or topical)
| Suture Size |
Part of the Eye |
| 10-0 |
Cornea |
| 9-0 |
Limbus |
| 8-0 |
Sclera |
The standard suture for a corneal laceration repair is 10-0 nylon with a fine spatulated needle. If a surgical needle has a high radius of curvature, it will lead to long passes, versus a smaller radius of curvature will lead to shorter passes.[3]
Personnel
- Ophthalmologist (surgeon)
- Surgical technician
- Operating room nurse
- Anesthesiologist/certified registered nurse anesthetist
Preparation
While the patient waits for a repair, cover the injured eye with a rigid eye shield.[11] Control pain and nausea with analgesics and antiemetics. Tell the patient to refrain from eating or drinking to be ready for surgery. Acquiring computed tomography(CT) of the face before the repair can identify foreign bodies, and is often the standard of care for ocular trauma at several institutions. Administer tetanus prophylaxis to the patient and start antibiotics early to prevent infection.[12][13]
Perform a basic eye exam cautiously to avoid worsening the injury or causing distress to the patient.[14] The exam can be challenging, but at minimum, perform a vision test with a Snellen chart or near vision card, pupil check, and a penlight or slit-lamp evaluation. Do not perform intraocular pressure if a full-thickness laceration is present or suspected. If unsure if the laceration is full-thickness, perform a Seidel test to confirm it.[15]
Before a corneal laceration repair, place a drop 5% povidone-iodine ophthalmic solution on the ocular surface as this is the most effective solution to reduce bacteria.[16] When performing the surgical preparation, ensure no pressure is applied to the eye to avoid protrusion of intraocular contents.
Technique or Treatment
The uniqueness of corneal lacerations for each patient leads to many ways to repair them. Each case is a puzzle, which the surgeon must complete. Some surgeons find joy in this, while others find it distressful. Despite your perspective and approach, the goal is to create a watertight closure by sealing the cornea without incorporating the intraocular contents, restoring the integrity of the globe, and preventing further damage to the cornea or other parts of the eye.[5] Following basic corneal suturing technique helps avoid excess postoperative corneal scarring and high residual astigmatism.
Anesthesia: Anesthesia management for corneal laceration repair varies from topical to general.[17] For a small laceration in the clinic, topical anesthesia or a peribulbar block may suffice. General anesthesia is ideal if the laceration is complex or tissue is protruding. General anesthesia is the preferred practice as it allows for a controlled repair and alleviates any patient anxiety or pain. A smooth induction is necessary for a full-thickness corneal laceration to prevent coughing, straining, or movement, which could cause prolapse of intraocular contents.[18]
Suspected corneal laceration: If unable to confirm a corneal laceration in the emergency room or clinic, transport the patient to the operating room for an exam under anesthesia and possible surgical repair.
Partial-thickness corneal laceration: Carefully debride partial-thickness lacerations. After debridement, perform a Seidel test to ensure that the laceration is still partial thickness. If the Seidel test is positive, it is a full-thickness laceration and follows the procedures below. If negative, use a contact lens or fibrin glue to help it heal and treat similar to a corneal abrasion.
Culture/Debride Laceration: Culture the wound carefully to avoid prolapsing intraocular tissue or pressure on the globe. The culture results can be beneficial if a patient develops an infection. Only the surgeon performing the repair should debride the tissue because improper debridement can further damage the eye. Excise necrotic tissue and reposit the remaining tissue into the eye. Remove any visible foreign bodies or debris.
Full-thickness corneal laceration less than 2 mm: Use cyanoacrylate or fibrin glue, amniotic membrane, or bandage contact lenses. However, if a watertight closure cannot be completed, suturing is required.[19][20][21] These techniques can often be completed in the clinic if the patient is cooperative. Many surgeons start with sutures for closure despite the size of the laceration. Sometimes it can be challenging to determine the size of the laceration on the bedside exam and is easier to evaluate in the operating room.
Full-thickness corneal laceration greater than 2 mm: This size of laceration usually requires sutures and should be repaired in the operating room.
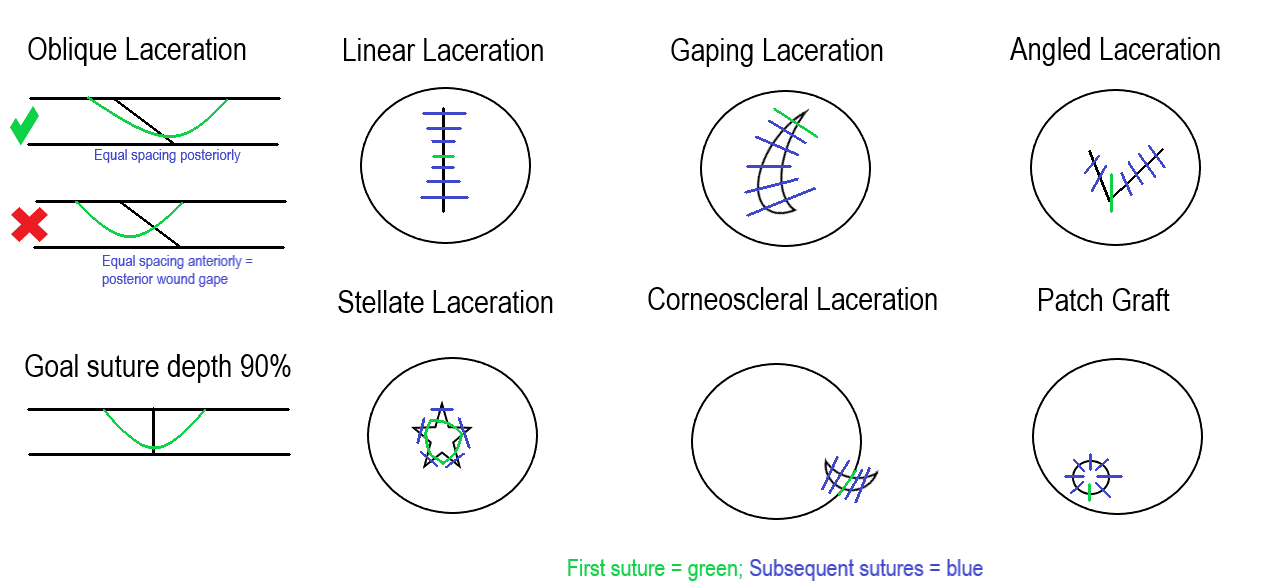
Evaluate the laceration and plan before passing a suture. Drawing out the repair organizes the surgical approach. Once a plan is in place, start suturing. The needle should enter the cornea perpendicular to the tissue when passing a suture. One method is to hold one side of the corneal wound at a 45-degree angle and enter the tissue at 45 degrees. Rotate the wrist following the needle curvature and come out the other side of the wound perpendicular to the tissue. Tie the suture with a slip knot, 2-1-1, or 3-1-1, and then cut the loose ends. The smaller the knot, the easier it is to bury.
Sutures should be passed at 90% depth in the stroma because too shallow can lead to posterior wound gape. Full-thickness passes can become a track for microorganisms to enter the eye.
When determining the placement of a second suture, remember the compression zones, which are triangular extensions from the suture, to ensure there are no gaps.[22]
Long sutures will have a large zone of compression compared to shorter sutures. Long sutures should be passed in the periphery to steepen the cornea centrally and seal the wound. Centrally the sutures are in the visual axis. Placing short sutures centrally with minimal suture tension will reduce astigmatism and prevent excess scarring.
Managing Tissue Prolapse
Following the pressure gradient, the iris and vitreous will prolapse through a corneal laceration until closure. It is important to avoid incorporating the tissue into the closure. There are several methods for managing prolapsed tissue. One strategy is to create a paracentesis away from the wound with a surgical blade and inject a viscoelastic. Use a cyclodialysis spatula to pull the iris back into the eye through a sweeping motion. Repositioning the intraocular tissue may be necessary throughout the suturing process. Accidental pressure on the globe when passing a suture or gaping the wound with instruments tends to protrude more tissue. If the patient is phakic, it is paramount to protect the lens and avoid violating the capsule.
The following are general guidelines for various scenarios—drawings depicted in the attached figure highlight each situation.
Oblique laceration: The suture will be an equal distance at the posterior part of the wound, but anteriorly will look displaced to one side. Avoid tension over the shallow side of the wound when tying the suture.
Linear laceration: Start suture placement in the center of the laceration and then bisect the halves until sealed.
Gaping laceration: Place the initial suture at the ends of the wound and then zip it up, keeping tissue out of the closure.
Angled laceration: The initial suture can be placed at the apex, then suture the sides as separate linear lacerations.
Stellate laceration: These closures can be challenging. A purse-string suture is placed centrally, either at the beginning or end of the closure, to help seal it. Interrupted sutures close the remaining aspects of the laceration.
Corneoscleral laceration: Place the initial suture at the limbus. This alignment is critical to repairing the cornea and scleral aspects. The limbus is usually the most identifiable tissue during the repair because of the contrast between the cornea and sclera. After closing the limbus, focus on the corneal aspect first and then the sclera to avoid tissue prolapse.
Tissue loss: When tissue is absent, a patch graft can create a watertight closure. There are various techniques for a patch graft that incorporate amniotic membrane, allograft tissue, or gamma-irradiated cornea.[23][24][25]
Finishing up
Once the corneal laceration repair is complete, test it for a leak with surgical spears or a fluorescein strip. If a leak is present, continue to suture or add adjuncts such as cyanoacrylate or fibrin glue, amniotic membrane, or contact lens. Ensure all knots are buried, ideally away from the visual axis.
A combination of intracameral, subconjunctival, topical, intravenous, and oral antibiotics decreases the risk of infections after the repair.
Patch the eye with surgical eye pads and cover it with a rigid eye shield.
Complications
Complications are avoidable with preoperative and postoperative antibiotics and proper intraoperative surgical technique.
Posttraumatic Endophthalmitis
Posttraumatic endophthalmitis is a devastating condition that occurs from 3.3% to 17% in penetrating trauma. The primary risk factors are a delay of primary surgical repair and violation of the lens capsule. The diagnosis can be difficult because the eye is already inflamed from the trauma and surgery.[26] Symptoms can be non-specific, including ocular pain, redness, eyelid swelling, discharge, decreased vision, and floaters. Treatment recommendations vary from a vitreous tap and injection with broad-spectrum antibiotics to a vitrectomy if vision is light perception or worse.[27]
Retained Intraocular Foreign Body
Intraocular foreign bodies in ocular trauma occur from 18 to 41%.[28] Ocular imaging prior to the surgical repair can identify foreign bodies. Sometimes foreign bodies can not be removed during a surgical repair, especially if located in the vitreous, so that further surgery may be necessary. Most foreign bodies are metallic and toxic to the eye; therefore, removal is recommended.[28]
Wound Leak
Evaluate the patient the day after the primary surgical repair with fluorescein to check for a wound leak. If a wound leak is present, a bandage contact lens or cyanoacrylate glue may seal it. If the leak is too brisk or large, more suturing is required to create a watertight closure. Wound leaks significantly increase the risk of infection.[29]
Suture Issues
Unburied knots and broken or loose sutures can cause the patient discomfort and serve as a track for microorganisms. All suture knots should be buried at the time of surgery; however, if recognized during the postoperative period, a knot can be rotated at the slit lamp. The timing of suture removal is variable depending on the patient's age, size of the laceration, and refractive anomaly induced by the suture.[30] However, remove broken or loose sutures immediately.
Iris Damage
The iris can tear or dislodge from its root through the initial trauma or during surgical repair. An abnormal iris can cause photophobia, visual disturbances, and an unpleasant aesthetic appearance.[31][32] Surgical techniques, corneal tattooing, contact lens, and artificial iris implants are available if the patient is symptomatic.[33][34]
Cataract
Cataracts can form from the initial trauma or during the operative repair if the lens capsule is violated. The majority of traumatic cataracts can safely be removed and replaced with a posterior or scleral-fixated lens to improve vision.[35]
Infectious Keratitis
Infectious keratitis can occur following trauma by various organisms.[36] Bacteria can build up on the sutures or form abscesses.[37] Treatment typically starts with fluoroquinolones, although fortified broad-spectrum antibiotics may be necessary for severe infections or resistant bacteria.
Retinal Detachment
Retinal detachments can occur during the trauma or subsequently in the postoperative period. Early intervention is key to preventing vision loss.
Posttraumatic Glaucoma
It is not uncommon for secondary glaucoma to occur from penetrating trauma due to various mechanisms.[38] Monitor the intraocular pressure during the postoperative period and counsel the patient about the long-term risk.
Sympathetic Ophthalmia
Sympathetic ophthalmia is an uncommon immune reaction that occurs in the non-traumatic eye after injuries or surgeries involving the uveal tissue.[39] Suspect this condition if inflammation occurs in the non-traumatic eye. The classic doctrine taught was to enucleate the traumatic eye within two weeks to prevent this condition; however, the current doctrine encourages leaving the traumatic eye in place if there is any vision still present.[40]
Vision Loss
Vision loss can occur from all of the complications discussed in this section. Traumatic damage to the optic nerve or other parts of the eye can also lead to vision loss. Corneal scarring, neovascularization, and irregular astigmatism are common reasons for decreased vision after a corneal laceration. Hard contact lenses can be helpful to determine if the visual complaint is related to the cornea versus other parts of the eye. A special fit contact lens can often improve vision significantly.[41] If the vision loss is related to corneal pathology and not improved with a contact lens, a corneal transplant may be beneficial once the eye has completely healed from the trauma.[42]
Clinical Significance
Visual acuity loss is detrimental to the quality of life.[43] The United States Eye Registry highlights at least a quarter of the patients with ocular trauma will have permanent vision loss.[44] Despite a perfect corneal laceration repair, vision loss may be present from corneal scarring, astigmatism, or damage to other parts of the eye.
Prevention with eye protection leads to the best vision outcomes and fewer injuries.[45][46][47] The mandate for eye protection in the U.S. military led to fewer and less severe ocular injuries.[48] In a patient with vision loss, eye protection is strongly recommended to protect the better-seeing eye. After ocular trauma, educating patients on protective eyewear should be incorporated into practice patterns.[49]
Enhancing Healthcare Team Outcomes
Improving outcomes for ocular trauma, including corneal lacerations, requires a team approach. Although the ophthalmologist performs the repair, many others help throughout the process. The initial step in the process is identifying a corneal laceration. Prompt recognition of an ocular injury by a bystander at the scene of the injury, paramedic, emergency room nurse, physician, or optometrist expedites the repair. After identifying the corneal laceration, cover the eye with a rigid eye shield to prevent further damage, and transfer the patient to an ophthalmologist. Occasionally, a patient is incorrectly diagnosed with a corneal abrasion which can delay the repair. In the ocular blast injuries from the Boston Marathon bombing and the West Texas fertilizer explosion, only 28% of the patients had ophthalmology consulted from the emergency room.[50]
The patient and family members almost always want to know if the patient’s vision will return to normal. Based on the United States Eye Registry, over 27% of the injuries involved permanent vision impairment. The Ocular Trauma Score is a tool for predicting the final vision of the injured eye and can be used by the team to educate the patient or their family.[51]
Nurses are vital members of the interprofessional group as they will monitor the patient’s vital signs, especially the pain level, pre-operatively and post-operatively. The radiologist has a role in identifying foreign bodies on facial computed tomography and can often confirm an open globe injury.[52] The pharmacist ensures the patient is on the correct analgesics, antiemetics, and antibiotics. If an infection is present or develops in the postoperative course, specialized fortified antibiotics may need to be compounded by the pharmacist.
The surgeon, surgical technician, operating nurse, and anesthesia provider all have roles in the outcome of the surgery. A well-organized surgical timeout that all members participate in improves patient safety. In the surgical repair, the surgical technician passes instruments to the surgeon, prevents needle stick injuries, and ensures correct needle counts. The anesthesia provider is vital to prevent the patient from moving during the surgical repair. Abrupt movements from the patient can lead to tissue protrusion and worsen the injury.
All team members educate the patient and family about postoperative care to include compliance with medications, signs of complications, activity limitations, and expected symptoms throughout the recovery process. Setting realistic expectations is important because many cases result in poor outcomes.[53]
A corneal laceration will change the refractive error of the patient. The patient may need a special contact lens fitting by an optometrist or an update in their prescription glasses to improve the visual outcome. The technological advances in contact lenses have improved patient visual outcomes after ocular trauma. A study of 214 patients with an open globe injury demonstrated a visual acuity improvement in 97% of the patients with a contact lens.
Nursing, Allied Health, and Interprofessional Team Interventions
The first person to recognize an eye injury should intervene and place a rigid eye shield over the eye. Nurses are vital in keeping the patient calm before the repair. Control of pain and nausea before and after the repair is necessary. Antibiotics should be administered at the onset of the injury and continued throughout the recovery period.
Any member of the care team should speak up if they notice anything unsafe or have any concerns.
Nursing, Allied Health, and Interprofessional Team Monitoring
Monitoring a patient's pain, nausea, and other vitals should occur before and after the repair. After the repair, the patient is either discharged home with a follow-up visit the next day in the clinic or kept overnight in the hospital for observation. During the postoperative period, especially the first week, all team members should monitor for signs of infection such as increased pain or decreased vision.
On the day of discharge, clear instructions from every team member to educate the patient about follow-up are paramount because many ocular trauma patients will not return.[54]