Continuing Education Activity
Hypercalcemia is a serum calcium (Ca) level over two standard deviations above the average mean values. That equates to a total serum calcium level greater than 10.5 mg/dl or an ionized calcium level greater than 5.3 mg/dl. Resistant hypercalcemia mainly occurs in diseased states with severely elevated serum calcium levels. It is predominantly reported in Malignancy-associated hypercalcemia and primary hyperparathyroidism and can sometimes be life-threatening. Early recognition and prompt diagnosis are essential to decrease mortality associated with this condition. This activity reviews the evaluation and management of resistant hypercalcemia and highlights the role of the healthcare team in managing patients with this condition.
Objectives:
- Outline the etiology of resistant hypercalcemia.
- Describe the pathophysiology of resistant hypercalcemia.
- Review the clinical presentation of resistant hypercalcemia.
- Summarize the management strategies taken by the interprofessional team available for resistant hypercalcemia.
Introduction
Hypercalcemia is a serum calcium (Ca) level over two standard deviations above the average mean values. That equates to a total serum calcium level greater than 10.5 mg/dl or an ionized calcium level greater than 5.3 mg/dl.[1] Normal serum calcium levels often range from 9.0 to 10.5 mg/dl. However, values may vary across laboratories. Only about 45% of serum calcium is in the free or ionized state; almost half of the serum concentration is bound to albumin, and about 10% is partially bound to small ions, including phosphate and citrate.[2]
Any state of dehydration or the process of hemoconcentration that occurs during venipuncture can falsely elevate total serum albumin levels and falsely account for elevated total serum calcium levels, whereas ionized calcium may remain normal. Changes in blood pressure can also alter serum albumin–calcium-binding. That is, alkalosis enhances binding, whereas acidosis decreases binding. Also, factors that cause low serum albumin levels, such as malnutrition and liver cirrhosis, will lead to falsely low reported serum calcium levels. Therefore, calcium levels must be corrected for abnormal serum albumin levels before the diagnosis of hypercalcemia can be established. This can be calculated as the measured total serum calcium (Mg/dL) + [4.0 - serum albumin (g/dL) X 0.8] or measured total serum + [40 - serum albumin (g/L) X 0.02].[3]
Hypercalcemia can be grouped based on serum calcium levels as follows:
- Mild hypercalcemia, which is total serum calcium ranging between 10.5 mg/dL and 11.9 mg/dL.
- Moderate hypercalcemia, which is a total serum calcium level ranging between 12 mg/dL and 13.9 mg/dL.
- Hypercalcemic crisis which is total serum calcium above 14 mg/dL.
Resistant hypercalcemia can be defined as persistently elevated calcium levels despite multiple therapy modalities or if re-administration is required within two weeks of initial therapy.[4]
Etiology
Etiologies of hypercalcemia can be grouped into the following categories: Endocrine disorders, malignancies, inflammatory diseases, medication-induced, and immobilization. Resistant hypercalcemia is caused by primary hyperparathyroidism and malignancy-associated hypercalcemia from various conditions. The following describes the multiple etiologies of hypercalcemia.[3]
Hypercalcemia due to endocrine disorders can be divided into two categories.
The first category includes endocrine disorders with the overproduction of parathyroid hormones (PTH), such as:
- Primary sporadic hyperparathyroidism (parathyroid adenoma, parathyroid hyperplasia, parathyroid carcinoma)
- Primary familial hyperparathyroidism or syndromic hyperparathyroidism (multiple endocrine neoplasia (MEN), type I and II, jaw tumor syndrome)
- Familial hypocalciuric hypercalcemia (FHH), including both the heterozygotes and homozygotes (neonatal severe primary hyperparathyroidism)
- Familial isolated hyperparathyroidism (non-syndromic hyperparathyroidism)
- Tertiary hyperparathyroidism, including chronic kidney disease and hypercalcemia related to phosphate treatment of hypophosphatemia crickets or osteomalacia
The second category includes endocrine disorders without overproduction of parathyroid hormones, such as:
- Hypothyroidism
- Pheochromocytoma
- Hypoadrenalism,
- VIPoma
- Jansen metaphyseal chondrodysplasia
Malignancy-related hypercalcemia (MHCM) constitutes about 90% of in-hospital hypercalcemia cases. It can be further classified according to parathyroid hormone levels. MHCM with elevated parathyroid hormone usually involves solid cancers, including breast, lung, kidney, and hematologic cancers, i.e., lymphoma and some leukemias. MHCM with normal parathyroid hormone levels includes lung cancers, ovarian cancers, and thyroid cancers. Various medications have been implicated in raising serum calcium levels, including lithium, aluminum intoxication, aminophylline/theophylline, tamoxifen, vitamin A, vitamin D, thiazide diuretics, and acid suppressants.
Infectious/inflammatory disorders, primarily granulomatous diseases, cause hypercalcemia secondary to extrarenal 1,25-hydroxyvitamin D production. These include:
- Sarcoidosis
- Wegener's granulomatosis
- Histoplasmosis
- Tuberculosis
- Cytomegalovirus infections
- Human immunodeficiency virus [HIV] infections
Pediatric syndromes such as Idiopathic infantile hypercalcemia and Williams syndrome are also etiologies of hypercalcemia. Immobilization occurs mainly in children or adults with restricted mobility due to spinal injury or other debilitating disorders. There is increased osteoclastic bone resorption, leading to elevated serum calcium levels.
Epidemiology
Hypercalcemia is a relatively common disease, especially among older women [about 3% of cases above age 60].[5] Malignancy-related hypercalcemia and hyperparathyroidism account for about 90% of cases. MHCM occurs mostly among hospitalized patients, and hyperparathyroidism-related hypercalcemia occurs mainly in the outpatient setting. Of the four types of MHCM, the most common is humoral hypercalcemia of malignancy, accounting for roughly 80% of cases.[4][6]
Pathophysiology
Various hormonal systems regulate calcium absorption and metabolism.[7] The most common players involved in directly or indirectly regulating serum calcium are PTH and Vitamin D.[8] Serum calcium levels rise due to three main processes, elevated intestinal calcium absorption, increased calcium mobilization from bone, and amplified calcium absorption from the kidneys. Hypercalcemia often results from the increased release of calcium from the bone by activating RANK (Receptor activator of nuclear factor-kappa B) receptors by RANK-Ligand (RANK-L), which are located on the surface of the osteoclasts.[9]
The primary mechanisms responsible for malignancy-related hypercalcemia include the overproduction of PTHrP by the tumor, osteolytic metastatic disease, and the ectopic activity of 1-alpha hydroxylase leading to overproduction of 1,25-dihydroxy cholecalciferol; ectopic PTH production by parathyroid and extra parathyroid malignancies; and excess serum calcium secondary to paraprotein binding.[4] PTH and PTHrP act on the same receptors, and their actions overlap.[10] PTHrP enhances calcitriol production, stimulates osteoclastic activity, facilitates renal calcium reabsorption, and decreases renal phosphate reabsorption.
Mutations/Loss of function of the CYP2481 enzyme [24-hydroxylase], responsible for inactivating 25-hydroxyvitamin D and 1,25-hydroxyvitamin D, can result in inappropriately elevated levels of 1,25-hydroxyvitamin D, leading to Renal failure, hypercalcemia, and hypercalciuria while suppressing PTH.[11]
The response of the parathyroid cells, thyroid c-cells, and renal tubular epithelial cells to changes in the extracellular fluid calcium levels is regulated by a G-protein coupled receptor called the calcium-sensing receptor (Ca-SR). This receptor also closely regulates calcitonin secretion and renal tubular calcium absorption. Abnormalities of the Ca-SR gene result in three rare disorders: familial benign hypocalciuric hypercalcemia, severe neonatal hyperparathyroidism, and autosomal dominant hypocalcemia with hypercalciuria.
History and Physical
It is essential to approach hypercalcemia history and physical examination by focusing on the signs and symptoms relevant to the disease and the underlying causative disorder. Symptoms can easily be remembered by using the mnemonic: bone (refers to bone pain, pathological fractures), groans (gastrointestinal symptoms including nausea, vomiting), stones (often kidney stones), moans (malaise, generalized weakness/ fatigue), and psychiatric overtones (i.e., confusion, depression).
Clinical manifestations can be summarized as follows, depending on the severity of hypercalcemia and the chronicity of the disease. Renal manifestations include polyuria, polydipsia, dehydration, nephrolithiasis, nephrocalcinosis, and renal failure. Gastrointestinal manifestations include anorexia, abdominal pain, nausea, vomiting, dyspepsia, peptic ulcer disease, constipation, and pancreatitis. Neuromuscular manifestations include depression, lethargy, cognitive dysfunction, coma, and fatigue. Cardiac manifestations include short QTC, Heart blocks, bradyarrhythmia, and hypertension.
Evaluation
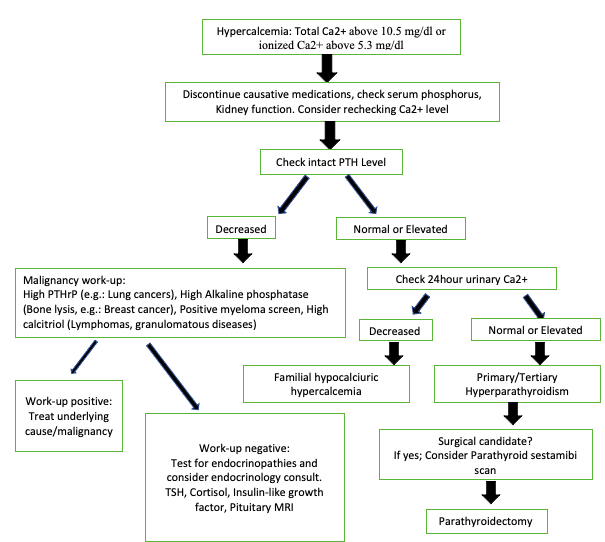
The first step in diagnosing hypercalcemia is to confirm elevated calcium levels by repeating the test. It is also essential to correct measured total serum calcium with albumin levels [conditions leading to low protein, e.g., nephrotic syndrome, malnutrition, and protein-losing enteropathies, can lead to low albumin levels, and therefore low laboratory-reported total serum levels]. It is also essential to differentiate between true hypercalcemia and pseudo hypercalcemia by obtaining ionized calcium levels and corrected calcium levels [for albumin]. However, it is prudent to initiate intravenous fluid resuscitation in severe hypercalcemia cases while awaiting repeat calcium measurements.[12]
Clinically, most cases of hypercalcemia are secondary to hyperparathyroidism and hypercalcemia of malignancy.[13] Mildly elevated calcium levels ongoing for months or years are mainly unrelated to malignancy. Hypercalcemia from malignancy is usually rapidly progressive leading to severely elevated calcium levels. However, if hypercalcemia has been ongoing for an unknown duration, patients should be promptly screened for possible cancers, such as kidney, lung, breast cancer, multiple myeloma, lymphoma, and leukemia.
After confirming the diagnosis of hypercalcemia, the next step is to differentiate between PTH-dependent and PTH-independent hypercalcemia, which can be achieved by measuring both PTH and PTHrP levels. In the case of malignancy-related hypercalcemia, PTH levels will be low or normal. Hypercalcemia with concurrent mid-to-upper normal or high PTH levels should suggest primary hyperparathyroidism.[14] Of note, some cancers may produce PTH ectopically.[15] Therefore imaging studies to evaluate the parathyroid glands for hyper functionality should be performed in exceptional cases. PTHrp levels are often elevated in patients with humoral hypercalcemia of malignancy. If PTHrP levels are found to be low, 1,25 dihydroxy- vitamin D levels should be measured to screen for vitamin D-mediated hypercalcemia.1,25-dihydroxy vitamin D could be elevated due to direct intake and granulomatous diseases or lymphoma. In addition, vitamin D intoxication can cause elevated 25-hydroxyvitamin D levels. However, if both PTHrP levels and vitamin D levels are low, then another source of hypercalcemia should be considered. Additional diagnostic workup should be considered for possible multiple myeloma ( serum and urine protein electrophoresis and serum free light chain assay), thyrotoxicosis (TSH), vitamin A toxicity, and osteolytic metastases (bone radiographs). Of note, various mechanisms of malignancy-related hypercalcemia may manifest in any particular patient.
Further evaluation should include a thorough medication list to review, and medications implicated in raising calcium levels should be discontinued. These can be restarted later if they are confirmed not to be the etiology for hypercalcemia. Diagnosing hypercalcemia in Neonates and infants who are also found to have dysmorphic features warrants quick evaluation for Williams or Murk Jansen syndrome.[14]
EKG features of hypercalcemia often include PR interval and QRS prolongation, ST elevation, T wave inversion, and a J wave. It is crucial to perform imaging studies to evaluate for possible malignancies. Surgical exploration of the neck should be performed in all resistant hypercalcemia cases, especially when other localizing investigations have proven futile and the etiology remains uncertain.
Treatment / Management
Hypercalcemia of malignancy is usually associated with severely elevated calcium levels and often presents as an oncologic emergency.[7] In cases of hypercalcemia with serum calcium less than 12 mg/dL (3 mM), management should be targeted toward the underlying condition, while severe or resistant hypercalcemia requires aggressive treatment.
Adequate hydration and fluid resuscitation are essential in every patient presenting with severe hypercalcemia. Due to diabetes insipidus induced by hypercalcemia, extracellular volume loss requires judicious fluid resuscitation with about 3 to 4 L of 0.9% sodium chloride within 48 hours. Hydration improves urinary calcium excretion and decreases tubular reabsorption of sodium and calcium.[16] The patient's cardiac and renal function should always be considered when initiating therapy. After adequate rehydration, a loop diuretic, such as furosemide 10 to 20 mg, can be administered intravenously to induce renal calcium excretion in cases of PTH or PTHrP-induced hypercalcemia.[8] Strict intake and output should be monitored.
Antiresorptive agents have proven to be effective in the management of resistant hypercalcemia. Severe hypercalcemia occurs from the increased mobilization of calcium from bone, regardless of the etiology. Bisphosphonates act to prevent osteoclastic action directly. Intravenous (IV) administration of zoledronic acid, 4 mg/5 ml, over 15 min or IV pamidronate, 90 mg in 500 ml/0.9% saline or 5% dextrose in water administered (D5W) over 4 hours.[17]
Renal function should be closely monitored during therapy. Another significant side effect of bisphosphonates is osteonecrosis of the jaw. Calcitonin is used for its rapid onset of action and safety in acute settings.[18] It works by inhibiting osteoclastic resorption and enhancing calcium elimination.[19] It can be administered at 4 to 8 IU/Kg intramuscularly (IM) or subcutaneously every 6 to 12 hours. Its effect peaks in about 2 to 6 hours. It can be used in combination with bisphosphonates or denosumab in cases of severe hypercalcemia. Rapid desensitization to increasing doses of the medication can occur after 24 to 48 hours. Denosumab is a monoclonal antibody to RANKL that decreases osteoclast action and bone resorption.[20] It is highly effective in hypercalcemia refractory to bisphosphonates.[21] The typical dose is 120 mg subcutaneous injection, which should not be repeated earlier than one week after initial administration.[22] This medication is not cleared by the kidney and can be used in patients with chronic kidney disease.
Gallium nitrate is used for the management of MHCM. It reduces osteoclast activity and bone remodeling.[23] It is very efficacious in decreasing calcium levels. However, it should be avoided in patients with renal failure as it can worsen renal function. Adequate fluid resuscitation and monitoring of electrolytes are essential before and during therapy.
Hydrocortisone 200 to 300 mg IV with a duration of 3 to 5 days may be administered for resistant hypercalcemia often related to hematologic malignancies such as lymphoma, myeloma, or in cases of vitamin D intoxication and granulomatous diseases.[24][25] Hemodialysis is reserved for critically elevated calcium levels resistant to other therapies, such as those listed above, and patients with renal disease.[26]
Calcimimetics such as cinacalcet can be used for the emergent treatment of severely elevated calcium levels. Cinacalcet acts on the calcium-sensing receptors, hence decreasing PTH secretion.[27] The initial dose of 30 mg twice daily, with a maximum dose of 90 mg 3 times daily, can be used in cases of hypercalcemia secondary to severe primary hyperparathyroidism, especially those caused by parathyroid carcinoma.[3] In a hypercalcemic crisis or resistant hypercalcemia, an urgent parathyroidectomy is potentially curative.[28] Elective parathyroidectomy is often done for parathyroid adenomas.
Criteria for surgery in primary hyperparathyroidism:[29]
|
Measurement
|
Total Serum calcium
|
Skeletal
|
Renal
|
Age
|
|
Criteria
|
1.0 mg/dL above the upper limit of normal (0.25 mmol/L)
|
-BMD: T-score <–2.5 at the lumbar spine, total hip, femoral neck, or distal 1/3 radius
-Vertebral fracture confirmed on Imaging.
|
-Creatinine clearance <60 mL/min
-24-hour urine calcium >400 mg/day and increased risk of nephrolithiasis
-Presence of stone formation or calcifications on radiograph, ultrasound, or CT
|
<50 years
|
|
Patients only need to meet one of these criteria to be recommended for parathyroid surgery. They do not have to meet more than one.
BMD: Bone mineral density; DXA: Dual Energy X-ray Absorptiometry; CT: computer tomography
|
Differential Diagnosis
The following abnormalities can present with symptoms similar to hypercalcemia manifestations.[30] These include the following:
- Azotemia
- Hypernatremia
- Hypermagnesemia
- Hyperphosphatemia
- Hyperkalemia
- Hyperparathyroidism
Prognosis
The prognosis of hypercalcemia mostly depends on the cause. Hypercalcemia caused by a benign disorder often has a good prognosis. Hyperparathyroidism-induced hypercalcemia is often less severe and of prolonged course. Cases of mild hypercalcemia rarely lead to death if appropriately treated. Cancer-related hypercalcemia often occurs in the later stages of the disease and poses a bleak prognosis with multiple ER visits and frequent hospitalizations.[31]
Hypercalcemia often leads to death in patients with ectopic PTHrP production. These patients rarely survive more than a few weeks or months. Osteolytic metastases tend to cause death from nerve compression and other orthopedic complications.[32][33]
Complications
Complications of Hypercalcemia can be related to the disease process itself or due to the side effects of therapies. Severely elevated hypercalcemia is an endocrine emergency and requires prompt management to avoid serious complications, which include severe volume contraction and cardiac and neurological consequences.[34] Complications from untreated hypercalcemia include the induction of abnormal heart rhythms. The electrocardiogram often shows T-wave flattening, mild prolongation of QRS and PR intervals, and the presence of Q-wave.
Chronically high serum calcium can precipitate to form crystals and eventually form calcium stones in the kidneys. Hypercalcemia inhibits renal autoregulation, induces diabetes insipidus, and causes increased serum osmolality and other metabolic disturbances leading to prerenal kidney injury with decreased glomerular filtration and renal excretion capacity. Osteoporosis occurs as a result of hypercalcemia bone resorption. In the case of persistent osteoclastic activity, bone thinning develops, with complications of fractures and loss of height. Severe hypercalcemia can result in delirium, confusion, dementia, and coma, which is often fatal.
Deterrence and Patient Education
Patient education becomes paramount regarding the etiology of their disease, especially for those with malignancy-related hypercalcemia. An interdisciplinary team involving oncology, nephrology, and endocrinology is often required to ensure adequate and well-coordinated care. Patients should be made aware of the mortality associated with severe hypercalcemia. Also, all available treatment options, including hemodialysis or parathyroidectomy, should be discussed, especially in cases of persistent/ resistant hypercalcemia.
Enhancing Healthcare Team Outcomes
Resistant hypercalcemia is associated with persistent, severely elevated calcium levels, leading to morbid complications, including death, if not promptly and properly managed. The pattern of multiple ER visits due to symptomatic hypercalcemia should prompt care providers to further evaluate possible causes of persistent hypercalcemia. Management should focus on the rapid reduction of serum calcium levels through calciuresis, decreased intestinal absorption of calcium, and reduced bone resorption. The mainstays of therapy include volume resuscitation, bisphosphonates, and calcitonin. However, despite preliminary treatment, denosumab has been proven to be an excellent choice of therapy in resistant hypercalcemia cases. Patients who do not respond to this therapy would require hemodialysis and, ultimately, surgical intervention in select patients.
The importance of the interprofessional approach cannot be under-emphasized. Early identification of symptomatic hypercalcemia by the emergency medicine physician is essential to initiate immediate hydration. The nephrology and hemodialysis team played a vital role in resistant hypercalcemia, requiring hemodialysis to normalize calcium levels. The endocrinologists will primarily coordinate the patient's care and determine treatment strategies. They will also decide which patients would benefit from denosumab versus other modes of therapy or when surgery becomes appropriate. Surgeons become significant members of the treatment team, mainly in parathyroid cancers and some other malignancy-related hypercalcemia, in which surgery becomes the last resort to normalize calcium levels. Nurses play significant roles in critical care and closely monitoring patient vitals and hemodynamics. Pharmacists can verify dosing, check for interactions, and consult with clinicians regarding adverse effects. All interprofessional team members should utilize open communication with the rest of the care team, particularly to communicate areas of concern and also maintain accurate and updated patient records so all caregivers have the data from which to base decisions. These examples of interprofessional interplay show how this approach will drive better patient results in hypercalcemia cases. [Level 5]