Technique or Treatment
To understand the applications of visual acuity testing, it is important to understand the different testing modalities used. The simplest method to evaluate distance visual acuity is a Snellen chart.[10][15] Care should be taken to have the patient stand at an appropriate distance from the chart in question and to test both eyes simultaneously as well as each eye individually. The visual acuity should be recorded as uncorrected (without glasses or contact lenses) and corrected (with glasses or contact lenses) visual acuity.
Methods of Assessing Visual Acuity
The results of visual acuity tests are usually noted with V, VA, or Va. Distance visual acuity is recorded as UCVA (uncorrected visual acuity) or BCVA (best-corrected visual acuity). BCVA is the best visual acuity achieved with refraction. Near vision may be identified by NV. Usually, distance visual acuity is evaluated first. By convention, the visual acuity of the right eye is recorded, followed by the left eye, and then the binocular vision is recorded.
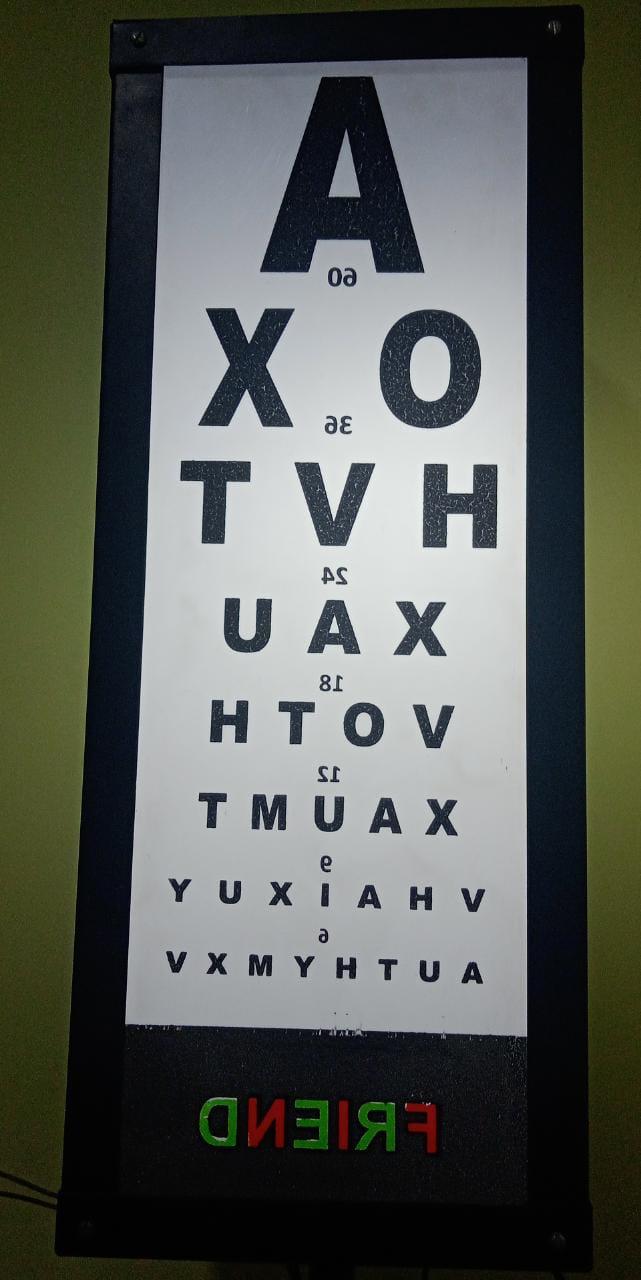
There are many visual acuity testing charts available. These charts can be printed, displayed on a computer or other screen, projected, or used with the help of a mirror. For testing at a distance of 6 meters in smaller examination rooms, a mirror can be placed at a 3-meter distance on the wall opposite the patient seat. The chart is placed on the wall behind the patient, just above their head. This chart is mirrored (horizontally inverted), and the letters become straight when viewed through the mirror (Figure 3). The image of the chart is formed behind the mirror at a distance of 6 meters from the patient.
Küchler Chart
The Küchler chart, believed to be the oldest known eye chart, was invented by German ophthalmologist Heinrich Georg Küchler in the 1830s or 1840s. The original chart included images of birds, guns, farm equipment, frogs, and others. Küchler later published another chart with 12 rows of letters.
Snellen Chart
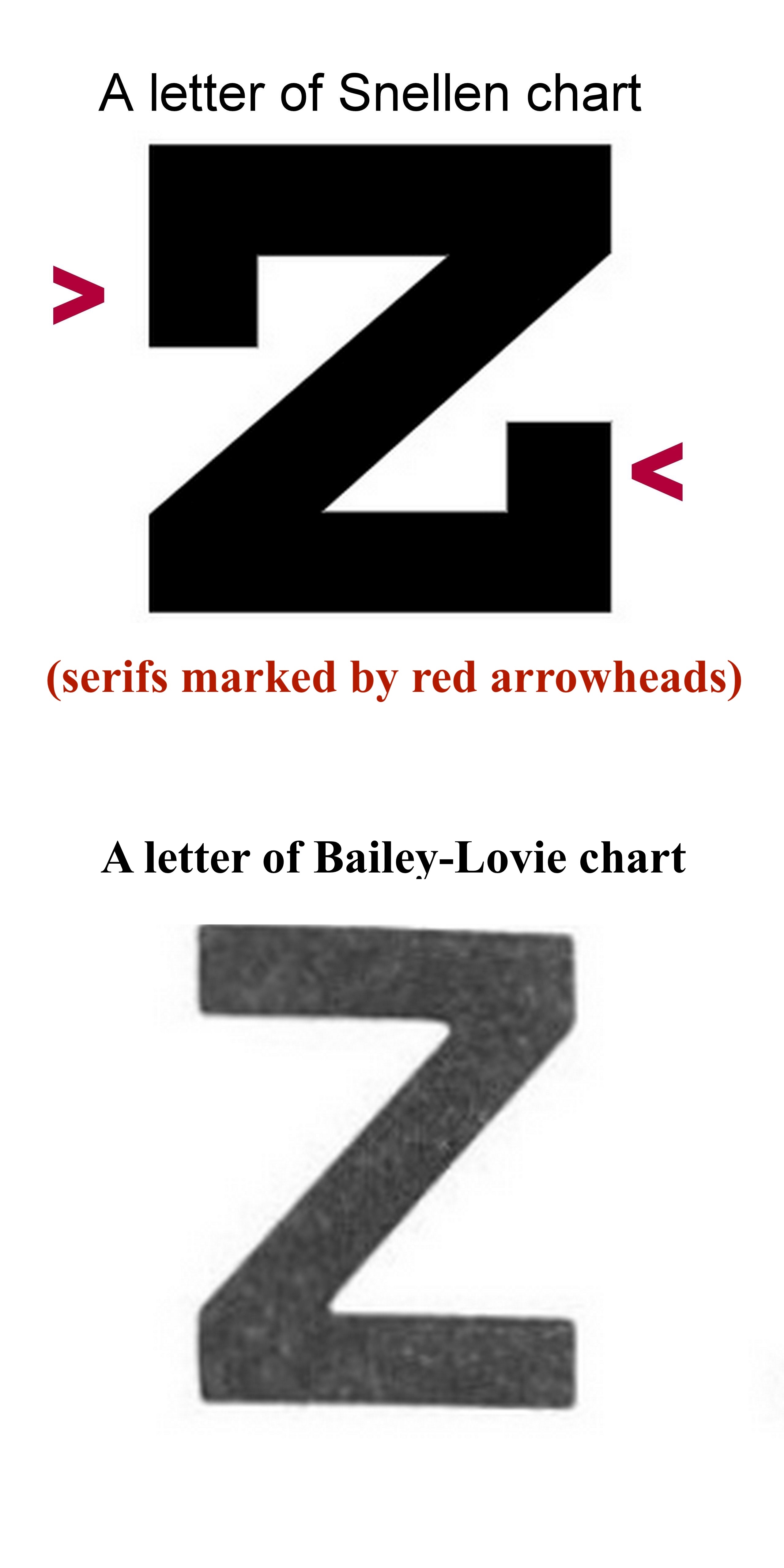
The Snellen chart was described in 1862 by Herman Snellen, a Dutch ophthalmologist.[15] This chart is very commonly used. The standard distance used for this chart is 20 feet or 6 meters. At this distance, the rays are almost parallel, and the patient usually does not accommodate to see at this distance. Chart luminance should be 80 to 320 cd/m2.[16] The usual luminance is 160 cd/m2. The Snellen chart has fewer letters in the upper part of the chart, and the number of letters increases as the visual acuity tested becomes finer toward the lower part of the chart. The spacing between horizontal letters varies between lines. The letters use serifs. Snellen called the targets used in the chart 'optotypes.'
The vertical height of a 6/6 (20/20) letter casts 5 minutes of arc at the nodal point of the eye when seen from 6 meters. The vertical height of each arm of E at 6/6 (20/20) line casts an angle of 1 minute of arc; in other words, the thickness of each stroke of the letter is 1 minute of arc. The height and width of the articles are the same (each is 5 times the stroke width). Thus, the height-to-width ratio is 5:5.
The height of a letter at the 6/6 (20/20) line is derived by the formula:
Tan (5min)= height of the letter in meters/6
Or, the height of the letter in meters = 6*tan 5 minute = 6*0.0015 meters = 0.009 meters = 9 mm
Similarly, the height of a letter in any line = 6 meters* tan (5x MAR)
The procedure to calculate MAR in minutes is described later.
In each of these charts, the black letters and white backgrounds have high contrast. The contrast is usually higher for a printed chart than for a projector-based chart. Therefore, the projector-based chart should be used in a dark room.
The size of a 6/36 letter is 60% of the 6/60 (20/200) letter. On the other hand, the size of a 6/6 (20/20) letter is 66% of a 6/9 (20/30) letter. Thus, the size change from one line to another is not uniform. Another issue with the Snellen chart is that finer visual acuity has more letters, which makes it difficult to read smaller letters due to the crowding phenomenon. This is especially true in patients with amblyopia. The letters used may not have similar legibility.[15] Reportedly, errors were more common with certain letters (S, F, C, B) than others (A, L, T, Z).[17]
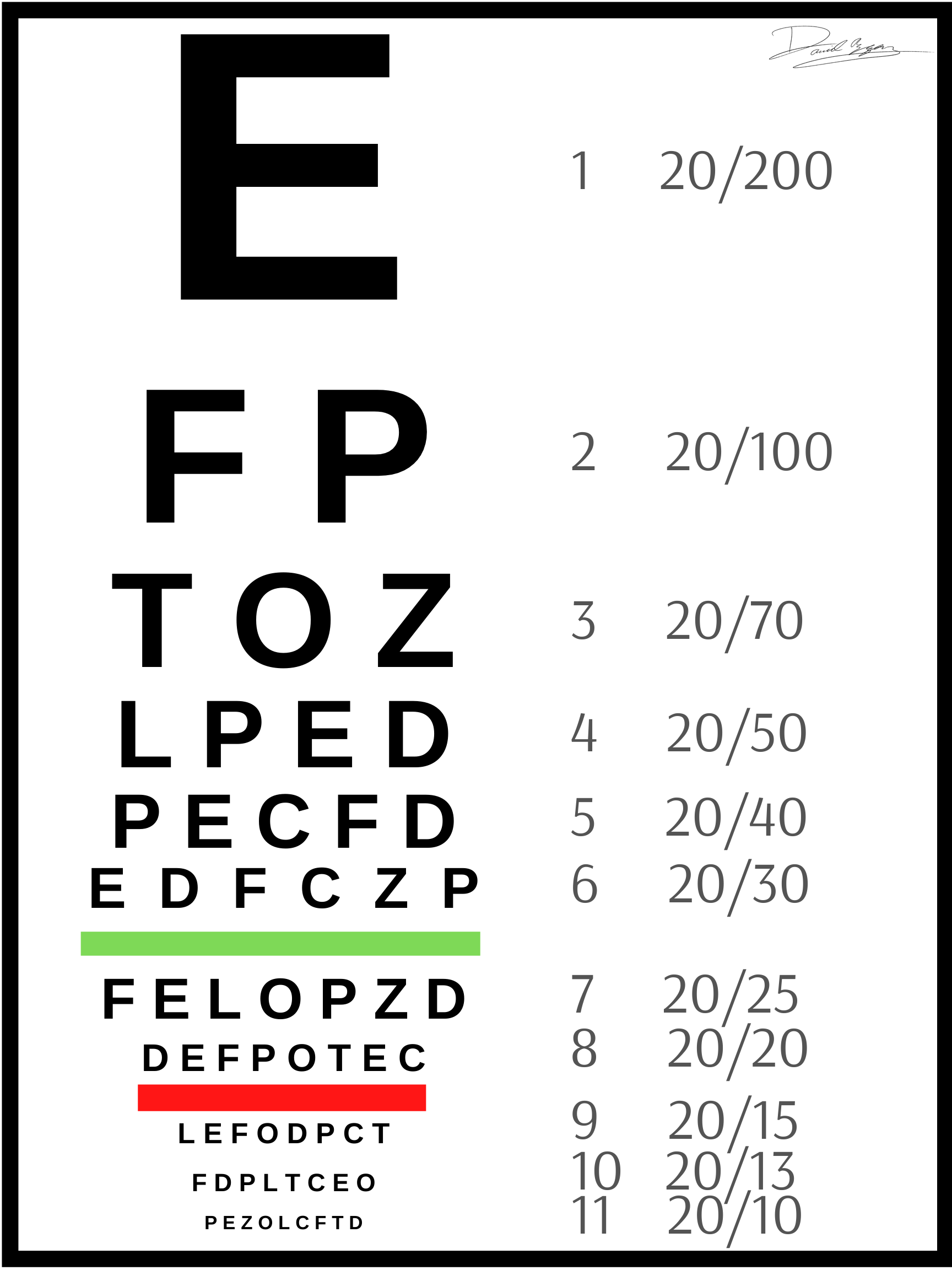
There are 7 lines in the Snellen chart (Figure 1). However, variations of this exist (Figure 3). The usually denoted visual acuity in each line is as follows, from the uppermost to the lowermost line:
- 6/60 (20/200) (contains one letter)
- 6/36 (20/120) (two letters)
- 6/24 (20/80) (three letters)
- 6/18 (20/60) (four letters)
- 6/12 (20/40) (five letters)
- 6/9 (20/30) (six letters)
- 6/6 (20/20) (seven letters)
As the lower rows have more letters, the chart has an A-shaped appearance from a distance.
The John Green chart from 1868 used sans-serif letters (Figure 2) and had up to 11 letters in each row. The spacing between letters was proportionate, and there was a geometric progression of the letter size in different rows.
The LogMAR Chart
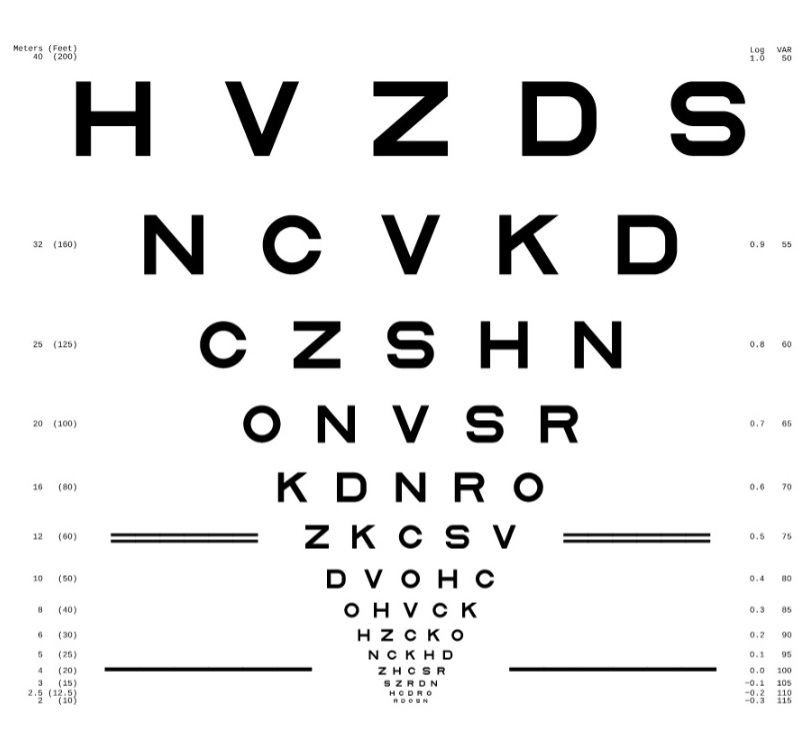
To overcome the limitations of the Snellen chart, the logMAR chart was introduced by Bailey and Lovie in 1976.[18] Such charts may provide higher sensitivity and reliability in the measurement of visual acuity.
LogMAR is the abbreviation of log (base 10) of the MAR (expressed in minutes). For statistical analysis, logMAR visual acuity is the best option.[19]
The features of the Bailey-Lovie logMAR chart are:
- The letters (optotypes) have equal recognition legibility and difficulty. This chart uses 10 sans-serif letters from the British Standard test charts for checking visual acuity as advocated by the British Standard Institution in 1968.
- There are five letters on every line.
- The height of a letter is 5 times the stroke width. The width of a letter is 4 times the stroke width. Thus, the ratio of height to width for each letter is 5:4.
- The distance between each letter in a single line is equal to the width of the letters (uniform inter-letter spacing). This creates a similar contour interaction in each line and possibly casts a similar crowding effect in each line.
- The distance between 2 rows is the height of the letters in the lower row (uniform inter-line or inter-row spacing).
- The ratio of the size of each letter in one line to the adjacent line is constant (geometric progression or progression in logarithmic steps). Weber Fechner's law states that the perceived intensity of a stimulus is proportional to the logarithm of the intensity of the stimulus. Therefore, the fixed difference between adjacent lines is 0.1 Log unit (the lower line has less value than the upper line). This translates to a size change of around 1.25 times or the 10th root of 10 (upper line letters being larger).
- Each letter has a logMAR value of 0.02 in each line.
- The Snellen notation [eg, 6/60 (20/200), 6/48 (20/160), etc) and logMAR values (1, 0.9, 0.8, etc) are given on either side of each row when seen from a 6-meter distance.
- For nonstandard testing distance, the distance may be changed in a logarithmic scale at 0.1 log unit steps. The possible distances are taken in geometric progression (multiplication by 0.8) and include 6, 4.8, 3.8, 3 meters, and so on. Notably, these distances can be remembered by dividing the denominator of the Snellen notations of different rows (like 6/60, 6/48, 6/38, 6/30, and more) of this chart by 10. Depending on the distance used, a correction factor is added to the logMAR value noted in the chart. For 4.8 meters distance, the correction factor is 0.1; for 3.8 meters, it is 0.2; for 3 meters, it is 0.3, and so on. The correct logMAR value of VA at a distance is the sum of the logMAR value of the lowest row seen plus the correction factor for the distance. For example, if a person sees the row of 6/30 (logMAR 0.7) at 4.8 meters (correction factor 0.1), the corrected visual acuity in logMAR is 0.7+0.1=0.8. For a distance of 7.5 meters, the correction factor is -0.1 (minus point one). Nonstandard testing distances may be needed in
- nonstandard design of the examination room
- patients with low visual acuity
- malingering
- validation of visual acuity scores
- The chart size is 80 cm (height) x 70 cm (width)
- Chart appearance is V-like when seen from a distance
Disadvantages of the chart include more time required for the examination, and the chart itself is much larger.
The most commonly used logMAR charts are the Bailey-Lovie and ETDRS charts (Figure 4).
ETDRS Chart
The ETDRS chart was described by Ferris and colleagues at the National Eye Institute, United States.[20] The ETDRS chart uses a luminance of 160 cd/m2.[16] Each optotype (Sloan letter, see below) has the same height and width; the ratio is 5:5. Thus, these letters are wider than the letters of the Bailey-Lovie chart. The ETDRS chart was designed to be read at a distance of 4 meters instead of 6 meters. The ETDRS chart may therefore be used to check visual acuity in smaller examination rooms.
The Snellen fraction at 4 meters may be converted to conventional American notation by multiplying the numerator and the denominator by 5. Thus, 4/5 is equivalent to 20/25. At 4 meters, the visual acuity is maximum, and the dispersion of visual acuity is minimum.[21] Refraction for infinity can be calculated by deducting 0.25 diopter from the refraction at 4 meters. Nonstandard distances used with the ETDRS chart are taken in a geometrical progression (3.2 m, 2.5 m, 2 m, 1.6 m, etc). The height and width of the chart are 60.3 cm and 63.5 cm, respectively. The reading of a single letter is allowed once only.
Other Visual Acuity Testing Charts
Other tests to evaluate visual acuity include the Golovin–Sivtsev table, Freiburg Visual Acuity Test (FrACT, automated self-administered computerized test), and the Waterloo, Rosebaum, Monoyer, and Regan charts.[22]
The Waterloo chart has letters in a column. It may result in lower visual acuity due to the psychophysiological phenomenon that visual acuity is better when recognizing letters in rows than in columns.[23] In the Monoyer chart, the lowest line has the largest letters, and the name Monoyer is spelled out when reading the leftmost letters upwards. This chart is another of the oldest available vision charts.
Optotypes
The standardized letters and shapes used to test visual acuity are called optotypes. Various optotypes used for testing visual acuity include:
- Landolt C chart - There are 4 configurations of the letter C, with the opening facing up, down, right, or left. Each configuration has similar legibility. Therefore, the chance of randomly guessing the correct response is 25% (1 in 4).
- Illiterate E chart - There are 4 configurations of the letter E, with the opening facing up, down, right, or left. Therefore, the chance of randomly guessing the correct response is 25% (1 in 4).
- Letters
- When all letters are used, the chance of randomly guessing the correct letter is low (1/26 or around 4%).
- The ETDRS chart uses Sloan letters, named after Louise Sloan, of which there are 10. Thus, the guess rate is 1/10, or 10%. The Sloan letters include C, D, H, K, N, O, R, S, V, and Z. The characteristics of the Sloan letter include equal difficulty in recognition of each letter when compared with the Landolt C chart.
- The Bailey-Lovie chart used the British set of 10 letters, and the guess rate is 10%. These letters are D, E, F, H, N, P, R, U, V, and Z.
- Numbers
- Other optotypes, primarily used for children, include Allen pictures and symbols.
Procedure for Checking Visual Acuity
Visual acuity is denoted by the smallest recognized optotype. It is documented in at least one of the following notations: the British or American Snellen fraction (6/6 or 20/20, respectively), the decimal acuity, or the logMAR.
For the Snellen chart, the patient is 6 meters away from the chart. Standard room illumination is used except for projector-based vision charts, where a darkened or dim room is preferred. The usual contrast of the visual acuity charts is at least 80%. If the person reads only the top letter of the Snellen chart, visual acuity is documented as 6/60; the top letter, which should be read at 60 m, is being read at 6 m. The same visual acuity is written as 0.1 on the decimal scale and 20/200 per the American standard for the Snellen fraction. Visual acuity of 6/60 is equivalent to +1.00 on the logMAR scale.
Similarly, if the line that should be read at 36 m is being read at 6 m, this should be documented as 6/36, 0.16 on the decimal scale, or 20/120. Visual acuity of 6/36 is equivalent to +0.78 on the logMAR scale. This progression can continue to the seventh line, documented as 6/6, 1.0 on the decimal scale, +0.00 on the logMAR scale, or 20/20 as the Snellen equivalent.
The distance is gradually reduced if the patient cannot read 6/60 at 6 m. If the top letter is seen at a distance of 5 meters, this is documented as 5/60. If it is seen at 4 meters, it is documented as 4/60. If the top letter cannot be seen at 1 meter, the patient is asked to count fingers; the examiner holds a certain number of fingers close to the patient's face. Finger counting at 6 meters is usually considered equivalent to 6/60, as the size of the 6/60 letter is roughly similar to a finger. Similarly, finger counting at 5 meters is around 5/60, and so on. Finger counting can be utilized to check visual acuity at the bedside if a vision chart is unavailable. Hand movement or hand motion (HM) is tested in a patient who cannot count fingers close to the face.
For HM visual acuity, one eye is closed. A light is shone from behind the patient over a hand kept 60 cm in front of the eye. The patient is asked to indicate whether the hand is not moving, moving up-down, or moving right-left. If the patient gives a correct response, including the direction of movement, at least 4 of the 5 times they are tested, then HM visual acuity is documented as present.[24]
The projection of rays (PR) is checked by closing the unaffected eye and asking the patient if they can correctly detect the direction from which the light from an indirect ophthalmoscope is projected over the eye (superior, inferior, nasal, or temporal). The responses of PR are recorded as + (present) or - (absent) in these quadrants. Light Perception (PL) is checked when the patient cannot appreciate hand movements. The light of an indirect ophthalmoscope set at maximum illumination is shone over the eye from the front at a distance of 90 cm. The patient is asked if the presence of light is appreciated or not.[24] Testing light perception with the potentially unaffected eye before checking the affected eye may help the patient cooperate and better comprehend the test. PL vision and no PL vision may not be quantifiable for statistical analysis.[19]
Testing Near and Intermediate Vision
The distance used for near vision testing may vary according to the work or occupation of the patient. Testing distances of 25, 30, 33, 35, or 40 cm are commonly used; 33 cm is most common. Charts for testing near vision include the Snellen, Times New Roman, or Jaeger near vision charts. In addition, charts for evaluating intermediate vision are available; testing usually is done at a distance of 66 cm or 80 cm.
Representation and Documentation of Visual Acuity
As aforementioned, many different nomenclatures are available to represent or document the results of visual acuity testing. British (test distance of 6 meters) and American (test distance of 20 feet) Snellen fractions are commonly used and described above.
The decimal fraction value is obtained by dividing the numerator of the Snellen fraction by the denominator. For example, for the Snellen fraction 6/60, 6 divided by 60 equals 0.1; this is the decimal fraction value.
The minimum angle of resolution (MAR) is the angle created at the nodal point of the eye documented in minutes. It is derived by dividing the denominator of the Snellen fraction by the numerator. Thus, for the Snellen fraction 6/60, 60 divided by 6 equals 10; this value, expressed in minutes, is the MAR.
The logMAR is the logarithm of MAR in minutes; the base is 10. For a Snellen fraction of 6/60, the MAR is 10, and the logMAR would be 1. For a Snellen fraction of 6/6, the MAR is 1, and the logMAR is 0.
Spatial frequency is expressed as cycles per degree (cpd). Spatial frequency is calculated by multiplying the decimal fraction value by 30. For example, for a Snellen fraction of 6/60, the decimal fraction is 0.1, equivalent to a spatial frequency of 3 cpd.
Louise Sloan introduced the M-unit (M) notation for the size of the optotype by converting the Snellen system to the metric system and using the formula decimal fraction value = test distance in meters (m)/letter size (M). According to the SI system, a patient with a visual acuity of 20/20 will be able to recognize a letter of 1M size at 1 meter. Similarly, a normal eye will be able to see a letter with a 20M size from 20 meters.