[1]
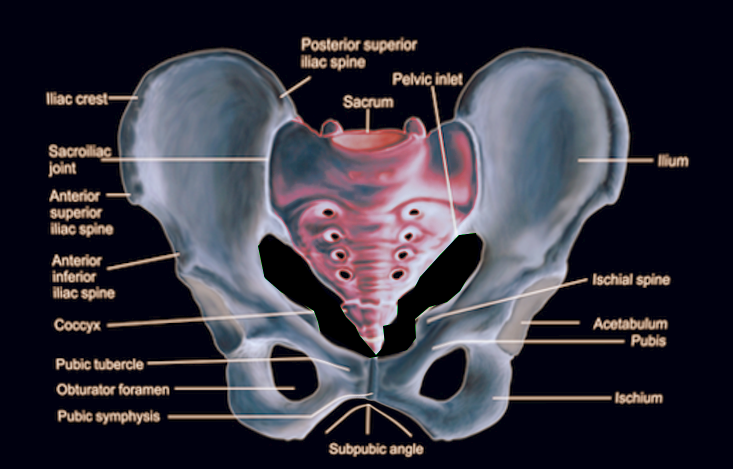
DeSilva JM, Rosenberg KR. Anatomy, Development, and Function of the Human Pelvis. Anatomical record (Hoboken, N.J. : 2007). 2017 Apr:300(4):628-632. doi: 10.1002/ar.23561. Epub
[PubMed PMID: 28297176]
[2]
Fritsch H, Lienemann A, Brenner E, Ludwikowski B. Clinical anatomy of the pelvic floor. Advances in anatomy, embryology, and cell biology. 2004:175():III-IX, 1-64
[PubMed PMID: 15152384]
Level 3 (low-level) evidence
[3]
Fritsch H, Hötzinger H. Tomographical anatomy of the pelvis, visceral pelvic connective tissue, and its compartments. Clinical anatomy (New York, N.Y.). 1995:8(1):17-24
[PubMed PMID: 7697508]
[4]
McGaugh JM, Brismée JM, Dedrick GS, Jones EA, Sizer PS. Comparing the anatomical consistency of the posterior superior iliac spine to the iliac crest as reference landmarks for the lumbopelvic spine: a retrospective radiological study. Clinical anatomy (New York, N.Y.). 2007 Oct:20(7):819-25
[PubMed PMID: 17729332]
Level 2 (mid-level) evidence
[5]
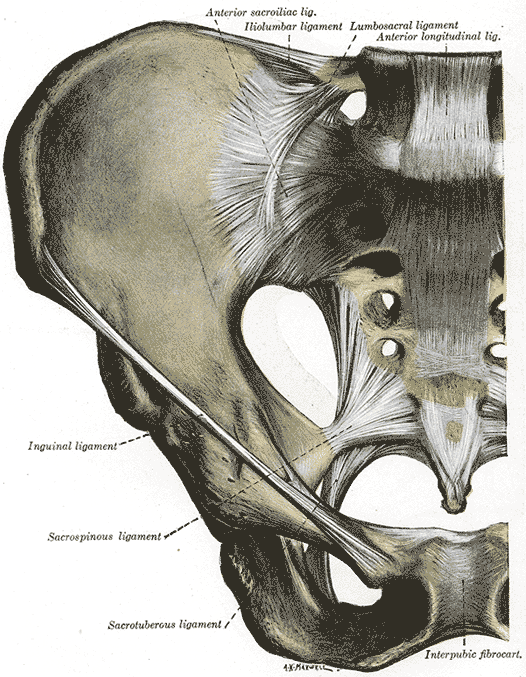
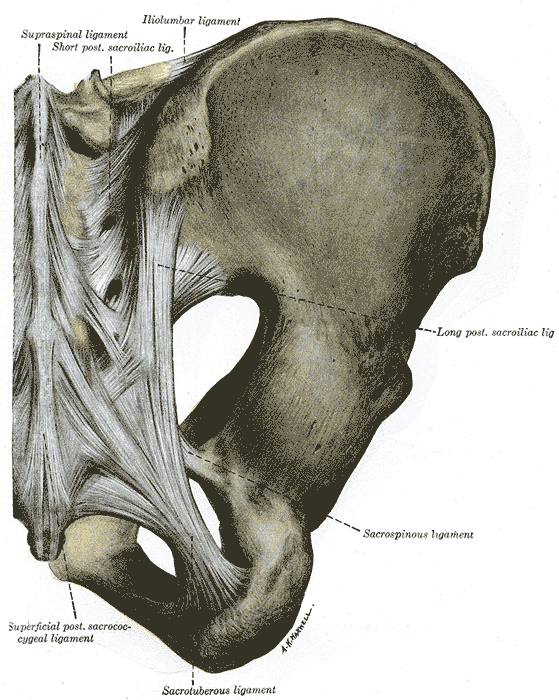
Ashby K, Yilmaz E, Mathkour M, Olewnik Ł, Hage D, Iwanaga J, Loukas M, Tubbs RS. Ligaments stabilizing the sacrum and sacroiliac joint: a comprehensive review. Neurosurgical review. 2022 Feb:45(1):357-364. doi: 10.1007/s10143-021-01625-y. Epub 2021 Aug 25
[PubMed PMID: 34432162]
[6]
Becker I, Woodley SJ, Stringer MD. The adult human pubic symphysis: a systematic review. Journal of anatomy. 2010 Nov:217(5):475-87. doi: 10.1111/j.1469-7580.2010.01300.x. Epub 2010 Sep 14
[PubMed PMID: 20840351]
Level 1 (high-level) evidence
[7]
Wu LP, Li YK, Li YM, Zhang YQ, Zhong SZ. Variable morphology of the sacrum in a Chinese population. Clinical anatomy (New York, N.Y.). 2009 Jul:22(5):619-26. doi: 10.1002/ca.20809. Epub
[PubMed PMID: 19484801]
[8]
Mahato NK. Relationship of sacral articular surfaces and gender with occurrence of lumbosacral transitional vertebrae. The spine journal : official journal of the North American Spine Society. 2011 Oct:11(10):961-5. doi: 10.1016/j.spinee.2011.08.007. Epub 2011 Sep 15
[PubMed PMID: 21924685]
[9]
Aggarwal A, Kaur H, Batra YK, Aggarwal AK, Rajeev S, Sahni D. Anatomic consideration of caudal epidural space: a cadaver study. Clinical anatomy (New York, N.Y.). 2009 Sep:22(6):730-7. doi: 10.1002/ca.20832. Epub
[PubMed PMID: 19637298]
[10]
Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. Journal of anatomy. 2012 Dec:221(6):537-67. doi: 10.1111/j.1469-7580.2012.01564.x. Epub 2012 Sep 19
[PubMed PMID: 22994881]
Level 3 (low-level) evidence
[11]
Hammer N, Steinke H, Lingslebe U, Bechmann I, Josten C, Slowik V, Böhme J. Ligamentous influence in pelvic load distribution. The spine journal : official journal of the North American Spine Society. 2013 Oct:13(10):1321-30. doi: 10.1016/j.spinee.2013.03.050. Epub 2013 Jun 5
[PubMed PMID: 23755919]
[12]
Aldabe D, Hammer N, Flack NAMS, Woodley SJ. A systematic review of the morphology and function of the sacrotuberous ligament. Clinical anatomy (New York, N.Y.). 2019 Apr:32(3):396-407. doi: 10.1002/ca.23328. Epub 2019 Feb 5
[PubMed PMID: 30592090]
Level 1 (high-level) evidence
[13]
Kachlik D, Vobornik T, Dzupa V, Marvanova Z, Toupal O, Navara E, Stevulova N, Baca V. Where and what arteries are most likely injured with pelvic fractures?: The Influence of Localization, Shape, and Fracture Dislocation on the Arterial Injury During Pelvic Fractures. Clinical anatomy (New York, N.Y.). 2019 Jul:32(5):682-688. doi: 10.1002/ca.23372. Epub 2019 Apr 2
[PubMed PMID: 30873674]
[14]
Michel F, Decavel P, Toussirot E, Tatu L, Aleton E, Monnier G, Garbuio P, Parratte B. The piriformis muscle syndrome: an exploration of anatomical context, pathophysiological hypotheses and diagnostic criteria. Annals of physical and rehabilitation medicine. 2013 May:56(4):300-11. doi: 10.1016/j.rehab.2013.03.006. Epub 2013 Apr 30
[PubMed PMID: 23684469]
[15]
Shoja MM, Sharma A, Mirzayan N, Groat C, Watanabe K, Loukas M, Tubbs RS. Neuroanatomy of the female abdominopelvic region: A review with application to pelvic pain syndromes. Clinical anatomy (New York, N.Y.). 2013 Jan:26(1):66-76. doi: 10.1002/ca.22200. Epub 2012 Nov 23
[PubMed PMID: 23175283]
[16]
Fröhlich B, Hötzinger H, Fritsch H. Tomographical anatomy of the pelvis, pelvic floor, and related structures. Clinical anatomy (New York, N.Y.). 1997:10(4):223-30
[PubMed PMID: 9213037]
[17]
Lawson JO. Pelvic anatomy. I. Pelvic floor muscles. Annals of the Royal College of Surgeons of England. 1974 May:54(5):244-52
[PubMed PMID: 4829749]
[18]
Guo M, Li D. Pelvic floor images: anatomy of the levator ani muscle. Diseases of the colon and rectum. 2007 Oct:50(10):1647-55
[PubMed PMID: 17762969]
[19]
Rocca Rossetti S. Functional anatomy of pelvic floor. Archivio italiano di urologia, andrologia : organo ufficiale [di] Societa italiana di ecografia urologica e nefrologica. 2016 Mar 31:88(1):28-37. doi: 10.4081/aiua.2016.1.28. Epub 2016 Mar 31
[PubMed PMID: 27072173]
[20]
Vučinić N, Paulsen F, Milinkov M, Nikolić MB, Todorović ST, Knezi N, Nikolić U. A survey of pelvic types on computed tomography images. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2022 Aug:243():151942. doi: 10.1016/j.aanat.2022.151942. Epub 2022 Apr 2
[PubMed PMID: 35378253]
Level 3 (low-level) evidence
[21]
Wall-Scheffler CM, Myers MJ. The Biomechanical and Energetic Advantages of a Mediolaterally Wide Pelvis in Women. Anatomical record (Hoboken, N.J. : 2007). 2017 Apr:300(4):764-775. doi: 10.1002/ar.23553. Epub
[PubMed PMID: 28297181]
[22]
Pavličev M, Romero R, Mitteroecker P. Evolution of the human pelvis and obstructed labor: new explanations of an old obstetrical dilemma. American journal of obstetrics and gynecology. 2020 Jan:222(1):3-16. doi: 10.1016/j.ajog.2019.06.043. Epub 2019 Jun 25
[PubMed PMID: 31251927]
[23]
Mostafa AMHAM, Kyriacou H, Chimutengwende-Gordon M, Khan WS. An overview of the key principles and guidelines in the management of pelvic fractures. Journal of perioperative practice. 2021 Sep:31(9):341-348. doi: 10.1177/1750458920947358. Epub 2020 Sep 8
[PubMed PMID: 32894996]
Level 3 (low-level) evidence
[24]
Stern N, Pignanelli M, Welk B. The management of an extraperitoneal bladder injury associated with a pelvic fracture. Canadian Urological Association journal = Journal de l'Association des urologues du Canada. 2019 Jun:13(6 Suppl4):S56-S60. doi: 10.5489/cuaj.5930. Epub
[PubMed PMID: 31194928]
[25]
Steer R, Balendra G, Matthews J, Wullschleger M, Reidy J. The use of anterior subcutaneous internal fixation (INFIX) for treatment of pelvic ring injuries in major trauma patients, complications and outcomes. SICOT-J. 2019:5():22. doi: 10.1051/sicotj/2019019. Epub 2019 Jun 28
[PubMed PMID: 31250805]
[26]
Chen HW, Liu GD, Fei J, Yi XH, Pan J, Ou S, Zhou JH. Treatment of unstable posterior pelvic ring fracture with percutaneous reconstruction plate and percutaneous sacroiliac screws: a comparative study. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association. 2012 Sep:17(5):580-7. doi: 10.1007/s00776-012-0257-1. Epub 2012 Jul 19
[PubMed PMID: 22810807]
Level 2 (mid-level) evidence
[27]
Qi H, Geng X, Yu X, Chen W, Jia J, Tian W. Posterior INFIX for Treating Unilateral Unstable Sacral Fractures. Orthopaedic surgery. 2022 Apr:14(4):750-757. doi: 10.1111/os.13251. Epub 2022 Mar 27
[PubMed PMID: 35343061]
Level 2 (mid-level) evidence
[28]
Do MT, Levine AD, Liu RW. An anatomical study defining the safe range of angles in percutaneous iliosacral and transsacral screw fixation. Clinical anatomy (New York, N.Y.). 2022 Apr:35(3):280-287. doi: 10.1002/ca.23807. Epub 2021 Nov 19
[PubMed PMID: 34766656]
[29]
Fierro NM, Dhillon NK, Siletz AE, Muníz T, Barmparas G, Ley EJ, Hashim YM. Which Pelvic Fractures Are Associated With Extravasation on Angiography? The American surgeon. 2022 Oct:88(10):2493-2498. doi: 10.1177/00031348221101514. Epub 2022 May 12
[PubMed PMID: 35546075]
[30]
Young JW, Burgess AR, Brumback RJ, Poka A. Pelvic fractures: value of plain radiography in early assessment and management. Radiology. 1986 Aug:160(2):445-51
[PubMed PMID: 3726125]
[31]
Alton TB, Gee AO. Classifications in brief: young and burgess classification of pelvic ring injuries. Clinical orthopaedics and related research. 2014 Aug:472(8):2338-42. doi: 10.1007/s11999-014-3693-8. Epub 2014 May 28
[PubMed PMID: 24867452]
[32]
Putnis SE, Pearce R, Wali UJ, Bircher MD, Rickman MS. Open reduction and internal fixation of a traumatic diastasis of the pubic symphysis: one-year radiological and functional outcomes. The Journal of bone and joint surgery. British volume. 2011 Jan:93(1):78-84. doi: 10.1302/0301-620X.93B1.23941. Epub
[PubMed PMID: 21196548]
[33]
Steelman K, Russell R, Vaidya R. Bilateral vertical shear sacroiliac joint dislocations treated with bilateral triangular osteosynthesis in a young female: A case report. Trauma case reports. 2021 Jun:33():100485. doi: 10.1016/j.tcr.2021.100485. Epub 2021 Apr 21
[PubMed PMID: 33997229]
Level 3 (low-level) evidence
[34]
Manson T, O'Toole RV, Whitney A, Duggan B, Sciadini M, Nascone J. Young-Burgess classification of pelvic ring fractures: does it predict mortality, transfusion requirements, and non-orthopaedic injuries? Journal of orthopaedic trauma. 2010 Oct:24(10):603-9. doi: 10.1097/BOT.0b013e3181d3cb6b. Epub
[PubMed PMID: 20871246]