[1]
Jiang YL, Zhang RC, Zhou YC. Comparison of overall survival and perioperative outcomes of laparoscopic pancreaticoduodenectomy and open pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: a systematic review and meta-analysis. BMC cancer. 2019 Aug 7:19(1):781. doi: 10.1186/s12885-019-6001-x. Epub 2019 Aug 7
[PubMed PMID: 31391085]
Level 1 (high-level) evidence
[2]
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA: a cancer journal for clinicians. 2022 Jan:72(1):7-33. doi: 10.3322/caac.21708. Epub 2022 Jan 12
[PubMed PMID: 35020204]
[3]
Are C, Dhir M, Ravipati L. History of pancreaticoduodenectomy: early misconceptions, initial milestones and the pioneers. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2011 Jun:13(6):377-84. doi: 10.1111/j.1477-2574.2011.00305.x. Epub 2011 Mar 31
[PubMed PMID: 21609369]
[4]
Schnelldorfer T, Adams DB, Warshaw AL, Lillemoe KD, Sarr MG. Forgotten pioneers of pancreatic surgery: beyond the favorite few. Annals of surgery. 2008 Jan:247(1):191-202
[PubMed PMID: 18156940]
[5]
Kimura W, Miyata H, Gotoh M, Hirai I, Kenjo A, Kitagawa Y, Shimada M, Baba H, Tomita N, Nakagoe T, Sugihara K, Mori M. A pancreaticoduodenectomy risk model derived from 8575 cases from a national single-race population (Japanese) using a web-based data entry system: the 30-day and in-hospital mortality rates for pancreaticoduodenectomy. Annals of surgery. 2014 Apr:259(4):773-80. doi: 10.1097/SLA.0000000000000263. Epub
[PubMed PMID: 24253151]
Level 3 (low-level) evidence
[6]
Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE. Hospital volume and surgical mortality in the United States. The New England journal of medicine. 2002 Apr 11:346(15):1128-37
[PubMed PMID: 11948273]
[7]
Asbun HJ, Stauffer JA. Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the Accordion Severity Grading System. Journal of the American College of Surgeons. 2012 Dec:215(6):810-9. doi: 10.1016/j.jamcollsurg.2012.08.006. Epub 2012 Sep 19
[PubMed PMID: 22999327]
[8]
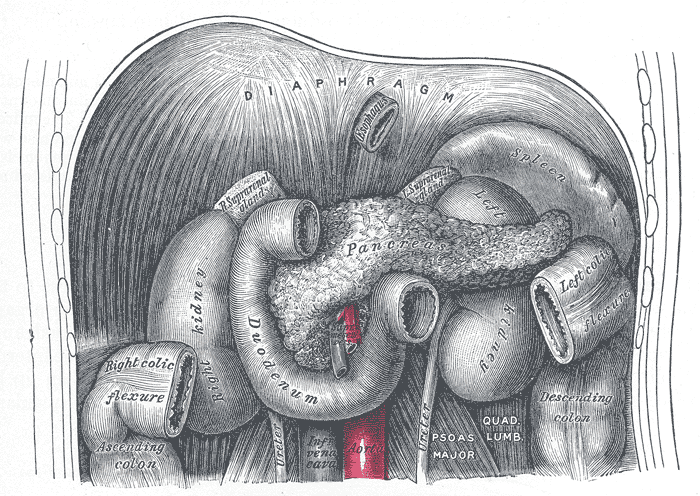
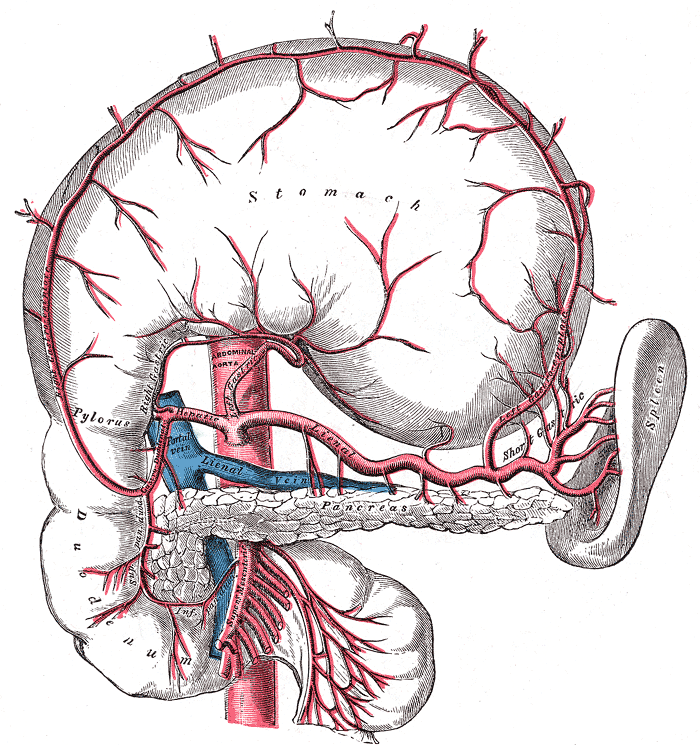
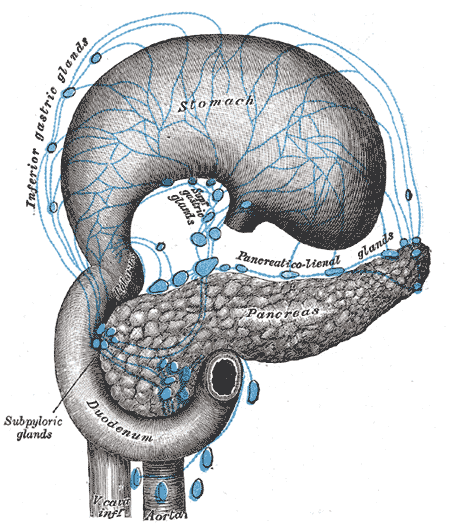
Skandalakis LJ, Rowe JS Jr, Gray SW, Skandalakis JE. Surgical embryology and anatomy of the pancreas. The Surgical clinics of North America. 1993 Aug:73(4):661-97
[PubMed PMID: 8378816]
[9]
Negoi I, Beuran M, Hostiuc S, Negoi RI, Inoue Y. Surgical Anatomy of the Superior Mesenteric Vessels Related to Colon and Pancreatic Surgery: A Systematic Review and Meta-Analysis. Scientific reports. 2018 Mar 8:8(1):4184. doi: 10.1038/s41598-018-22641-x. Epub 2018 Mar 8
[PubMed PMID: 29520096]
Level 1 (high-level) evidence
[10]
O'Sullivan AW, Heaton N, Rela M. Cancer of the uncinate process of the pancreas: surgical anatomy and clinicopathological features. Hepatobiliary & pancreatic diseases international : HBPD INT. 2009 Dec:8(6):569-74
[PubMed PMID: 20007071]
[11]
Covey AM, Brody LA, Maluccio MA, Getrajdman GI, Brown KT. Variant hepatic arterial anatomy revisited: digital subtraction angiography performed in 600 patients. Radiology. 2002 Aug:224(2):542-7
[PubMed PMID: 12147854]
[12]
Rubio-Manzanares-Dorado M, Marín-Gómez LM, Aparicio-Sánchez D, Suárez-Artacho G, Bellido C, Álamo JM, Serrano-Díaz-Canedo J, Padillo-Ruiz FJ, Gómez-Bravo MÁ. Implication of the presence of a variant hepatic artery during the Whipple procedure. Revista espanola de enfermedades digestivas. 2015 Jul:107(7):417-22
[PubMed PMID: 26140634]
[13]
Liang B, Chen Y, Li M, Dong X, Yao S, Liu T. Total laparoscopic duodenum-preserving pancreatic head resection for solid pseudopaillary neoplasm of pancreas: A case report. Medicine. 2019 May:98(21):e15823. doi: 10.1097/MD.0000000000015823. Epub
[PubMed PMID: 31124984]
Level 3 (low-level) evidence
[14]
Kim H, Song KB, Hwang DW, Lee JH, Alshammary S, Kim SC. Laparoscopic versus open pancreaticoduodenectomy for pancreatic neuroendocrine tumors: a single-center experience. Surgical endoscopy. 2019 Dec:33(12):4177-4185. doi: 10.1007/s00464-019-06969-7. Epub 2019 Jul 12
[PubMed PMID: 31300907]
[15]
Zhou Y, Wang X, Si X, Wang S, Cai Z. Surgery for duodenal gastrointestinal stromal tumor: A systematic review and meta-analysis of pancreaticoduodenectomy versus local resection. Asian journal of surgery. 2020 Jan:43(1):1-8. doi: 10.1016/j.asjsur.2019.02.006. Epub 2019 Mar 8
[PubMed PMID: 30853211]
Level 1 (high-level) evidence
[16]
Hüttner FJ, Capdeville L, Pianka F, Ulrich A, Hackert T, Büchler MW, Probst P, Diener MK. Systematic review of the quantity and quality of randomized clinical trials in pancreatic surgery. The British journal of surgery. 2019 Jan:106(1):23-31. doi: 10.1002/bjs.11030. Epub
[PubMed PMID: 30582642]
Level 2 (mid-level) evidence
[17]
Babiker HM, Hoilat GJ, Menon G, Mukkamalla SKR. Mucinous Cystic Pancreatic Neoplasms. StatPearls. 2024 Jan:():
[PubMed PMID: 28846358]
[18]
Morales E, Zimmitti G, Codignola C, Manzoni A, Garatti M, Sega V, Rosso E. Follow "the superior mesenteric artery": laparoscopic approach for total mesopancreas excision during pancreaticoduodenectomy. Surgical endoscopy. 2019 Dec:33(12):4186-4191. doi: 10.1007/s00464-019-06994-6. Epub 2019 Jul 22
[PubMed PMID: 31332566]
[19]
Yoshimachi S, Ohtsuka H, Aoki T, Miura T, Ariake K, Masuda K, Ishida M, Mizuma M, Hayashi H, Nakagawa K, Morikawa T, Motoi F, Kanno A, Masamune A, Fujishima F, Sasano H, Kamei T, Naitoh T, Unno M. Mixed adenoneuroendocrine carcinoma of the ampulla of Vater: a case report and literature review. Clinical journal of gastroenterology. 2020 Feb:13(1):37-45. doi: 10.1007/s12328-019-01009-2. Epub 2019 Jul 24
[PubMed PMID: 31342462]
Level 3 (low-level) evidence
[20]
Mikulić D, Bubalo T, Mrzljak A, Škrtić A, Jadrijević S, Kanižaj TF, Kocman B. Role of total pancreatectomy in the treatment of paraduodenal pancreatitis: A case report. World journal of gastrointestinal surgery. 2019 Jun 27:11(6):296-302. doi: 10.4240/wjgs.v11.i6.296. Epub
[PubMed PMID: 31367277]
Level 3 (low-level) evidence
[21]
Rios G, Conrad A, Cole D, Adams D, Leveen M, O'Brien P, Baron P. Trends in indications and outcomes in the Whipple procedure over a 40-year period. The American surgeon. 1999 Sep:65(9):889-93
[PubMed PMID: 10484097]
[22]
Tempero MA, Malafa MP, Al-Hawary M, Asbun H, Bain A, Behrman SW, Benson AB 3rd, Binder E, Cardin DB, Cha C, Chiorean EG, Chung V, Czito B, Dillhoff M, Dotan E, Ferrone CR, Hardacre J, Hawkins WG, Herman J, Ko AH, Komanduri S, Koong A, LoConte N, Lowy AM, Moravek C, Nakakura EK, O'Reilly EM, Obando J, Reddy S, Scaife C, Thayer S, Weekes CD, Wolff RA, Wolpin BM, Burns J, Darlow S. Pancreatic Adenocarcinoma, Version 2.2017, NCCN Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network : JNCCN. 2017 Aug:15(8):1028-1061. doi: 10.6004/jnccn.2017.0131. Epub
[PubMed PMID: 28784865]
Level 1 (high-level) evidence
[23]
Mullapudi B, Hawkes PJ, Patel A, Are C, Misra S. Borderline resectable pancreatic cancer. Indian journal of surgical oncology. 2015 Mar:6(1):63-68. doi: 10.1007/s13193-014-0374-8. Epub 2015 Jan 4
[PubMed PMID: 25937766]
[24]
Ta R, O'Connor DB, Sulistijo A, Chung B, Conlon KC. The Role of Staging Laparoscopy in Resectable and Borderline Resectable Pancreatic Cancer: A Systematic Review and Meta-Analysis. Digestive surgery. 2019:36(3):251-260. doi: 10.1159/000488372. Epub 2018 Apr 12
[PubMed PMID: 29649825]
Level 1 (high-level) evidence
[25]
Warshaw AL, Thayer SP. Pancreaticoduodenectomy. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2004 Sep-Oct:8(6):733-41. doi: 10.1016/j.gassur.2004.03.005. Epub
[PubMed PMID: 15358336]
[26]
Vasiliadis KD. "Mesopancreas-first" radical resection of pancreatic head cancer following the Cattell-Braasch-Valdoni maneuver: Appreciating the legacy of pioneers in visceral surgery. Annals of hepato-biliary-pancreatic surgery. 2021 Aug 31:25(3):376-385. doi: 10.14701/ahbps.2021.25.3.376. Epub
[PubMed PMID: 34402439]
[27]
Gao Y, Lu Y. Variations of Gastrocolic Trunk of Henle and Its Significance in Gastrocolic Surgery. Gastroenterology research and practice. 2018:2018():3573680. doi: 10.1155/2018/3573680. Epub 2018 Jun 6
[PubMed PMID: 29977286]
[28]
Lad NL, Squires MH, Maithel SK, Fisher SB, Mehta VV, Cardona K, Russell MC, Staley CA, Adsay NV, Kooby DA. Is it time to stop checking frozen section neck margins during pancreaticoduodenectomy? Annals of surgical oncology. 2013 Oct:20(11):3626-33. doi: 10.1245/s10434-013-3080-9. Epub 2013 Jul 10
[PubMed PMID: 23838908]
[29]
Guo C, Xie B, Guo D. Does pancreatic duct stent placement lead to decreased postoperative pancreatic fistula rates after pancreaticoduodenectomy? A meta-analysis. International journal of surgery (London, England). 2022 Jul:103():106707. doi: 10.1016/j.ijsu.2022.106707. Epub 2022 Jun 10
[PubMed PMID: 35697324]
Level 1 (high-level) evidence
[30]
Xiong JJ, Altaf K, Mukherjee R, Huang W, Hu WM, Li A, Ke NW, Liu XB. Systematic review and meta-analysis of outcomes after intraoperative pancreatic duct stent placement during pancreaticoduodenectomy. The British journal of surgery. 2012 Aug:99(8):1050-61. doi: 10.1002/bjs.8788. Epub 2012 May 24
[PubMed PMID: 22622664]
Level 1 (high-level) evidence
[31]
Berger AC, Howard TJ, Kennedy EP, Sauter PK, Bower-Cherry M, Dutkevitch S, Hyslop T, Schmidt CM, Rosato EL, Lavu H, Nakeeb A, Pitt HA, Lillemoe KD, Yeo CJ. Does type of pancreaticojejunostomy after pancreaticoduodenectomy decrease rate of pancreatic fistula? A randomized, prospective, dual-institution trial. Journal of the American College of Surgeons. 2009 May:208(5):738-47; discussion 747-9. doi: 10.1016/j.jamcollsurg.2008.12.031. Epub
[PubMed PMID: 19476827]
Level 1 (high-level) evidence
[32]
Andersson R, Søreide K, Ansari D. The Dilemma of Drains after Pancreatoduodenectomy: Still an Issue? Scandinavian journal of surgery : SJS : official organ for the Finnish Surgical Society and the Scandinavian Surgical Society. 2020 Dec:109(4):359-361. doi: 10.1177/1457496919866014. Epub 2019 Aug 1
[PubMed PMID: 31370750]
[33]
Bergeat D, Merdrignac A, Robin F, Gaignard E, Rayar M, Meunier B, Beloeil H, Boudjema K, Laviolle B, Sulpice L. Nasogastric Decompression vs No Decompression After Pancreaticoduodenectomy: The Randomized Clinical IPOD Trial. JAMA surgery. 2020 Sep 1:155(9):e202291. doi: 10.1001/jamasurg.2020.2291. Epub 2020 Sep 16
[PubMed PMID: 32667635]
Level 1 (high-level) evidence
[34]
Koek S, Wiegele S, Ballal M. Drain fluid amylase and lipase as a predictive factor of postoperative pancreatic fistula. ANZ journal of surgery. 2022 Mar:92(3):414-418. doi: 10.1111/ans.17296. Epub 2021 Oct 22
[PubMed PMID: 34676961]
[35]
Navez J, Hubert C, Dokmak S, Frick De La Maza I, Tabchouri N, Benoit O, Hermand H, Zech F, Gigot JF, Sauvanet A. Early Versus Late Oral Refeeding After Pancreaticoduodenectomy for Malignancy: a Comparative Belgian-French Study in Two Tertiary Centers. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2020 Jul:24(7):1597-1604. doi: 10.1007/s11605-019-04316-8. Epub 2019 Jul 19
[PubMed PMID: 31325133]
Level 2 (mid-level) evidence
[36]
Simon R. Complications After Pancreaticoduodenectomy. The Surgical clinics of North America. 2021 Oct:101(5):865-874. doi: 10.1016/j.suc.2021.06.011. Epub 2021 Jul 29
[PubMed PMID: 34537148]
[37]
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M, International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005 Jul:138(1):8-13
[PubMed PMID: 16003309]
[38]
Morgan KA, Adams DB. Management of internal and external pancreatic fistulas. The Surgical clinics of North America. 2007 Dec:87(6):1503-13, x
[PubMed PMID: 18053844]
[39]
Feng F, Cao X, Liu X, Qin J, Xing Z, Duan J, Liu C, Liu J. Two forms of one complication: Late erosive and nonerosive postpancreatectomy hemorrhage following laparoscopic pancreaticoduodenectomy. Medicine. 2019 Jul:98(30):e16394. doi: 10.1097/MD.0000000000016394. Epub
[PubMed PMID: 31348239]
Level 2 (mid-level) evidence
[40]
Kato H, Iizawa Y, Nakamura K, Gyoten K, Hayasaki A, Fujii T, Murata Y, Tanemura A, Kuriyama N, Azumi Y, Kishiwada M, Mizuo S, Usui M, Sakurai H, Isaji S. The Critical Role of Biliary Candidiasis in Development of Surgical Site Infections after Pancreatoduodenectomy: Results of Prospective Study Using a Selective Culture Medium for Candida Species. BioMed research international. 2018:2018():5939724. doi: 10.1155/2018/5939724. Epub 2018 Nov 18
[PubMed PMID: 30581862]
[41]
Ashitomi Y, Sugawara S, Takahashi R, Ashino K, Watanabe T, Hachiya O, Kimura W. Severe acute pancreatitis 5 years after pancreaticoduodenectomy: A case report. International journal of surgery case reports. 2019:61():99-102. doi: 10.1016/j.ijscr.2019.07.045. Epub 2019 Jul 22
[PubMed PMID: 31357105]
Level 3 (low-level) evidence
[42]
Goess R, Ceyhan GO, Friess H. Pancreatic exocrine insufficiency after pancreatic surgery. Panminerva medica. 2016 Jun:58(2):151-9
[PubMed PMID: 27058237]
[43]
Maxwell DW, Jajja MR, Tariq M, Mahmooth Z, Galindo RJ, Sweeney JF, Sarmiento JM. Development of Diabetes after Pancreaticoduodenectomy: Results of a 10-Year Series Using Prospective Endocrine Evaluation. Journal of the American College of Surgeons. 2019 Apr:228(4):400-412.e2. doi: 10.1016/j.jamcollsurg.2018.12.042. Epub 2019 Jan 26
[PubMed PMID: 30690075]
[44]
Oh HM, Yoon YS, Han HS, Kim JH, Cho JY, Hwang DW. Risk factors for pancreatogenic diabetes after pancreaticoduodenectomy. Korean journal of hepato-biliary-pancreatic surgery. 2012 Nov:16(4):167-71. doi: 10.14701/kjhbps.2012.16.4.167. Epub 2012 Nov 30
[PubMed PMID: 26388929]
[45]
Giuliano K, Ejaz A, He J. Technical aspects of pancreaticoduodenectomy and their outcomes. Chinese clinical oncology. 2017 Dec:6(6):64. doi: 10.21037/cco.2017.09.01. Epub 2017 Sep 26
[PubMed PMID: 29156887]
[46]
Ferrone CR, Brennan MF, Gonen M, Coit DG, Fong Y, Chung S, Tang L, Klimstra D, Allen PJ. Pancreatic adenocarcinoma: the actual 5-year survivors. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2008 Apr:12(4):701-6
[PubMed PMID: 18027062]