Continuing Education Activity
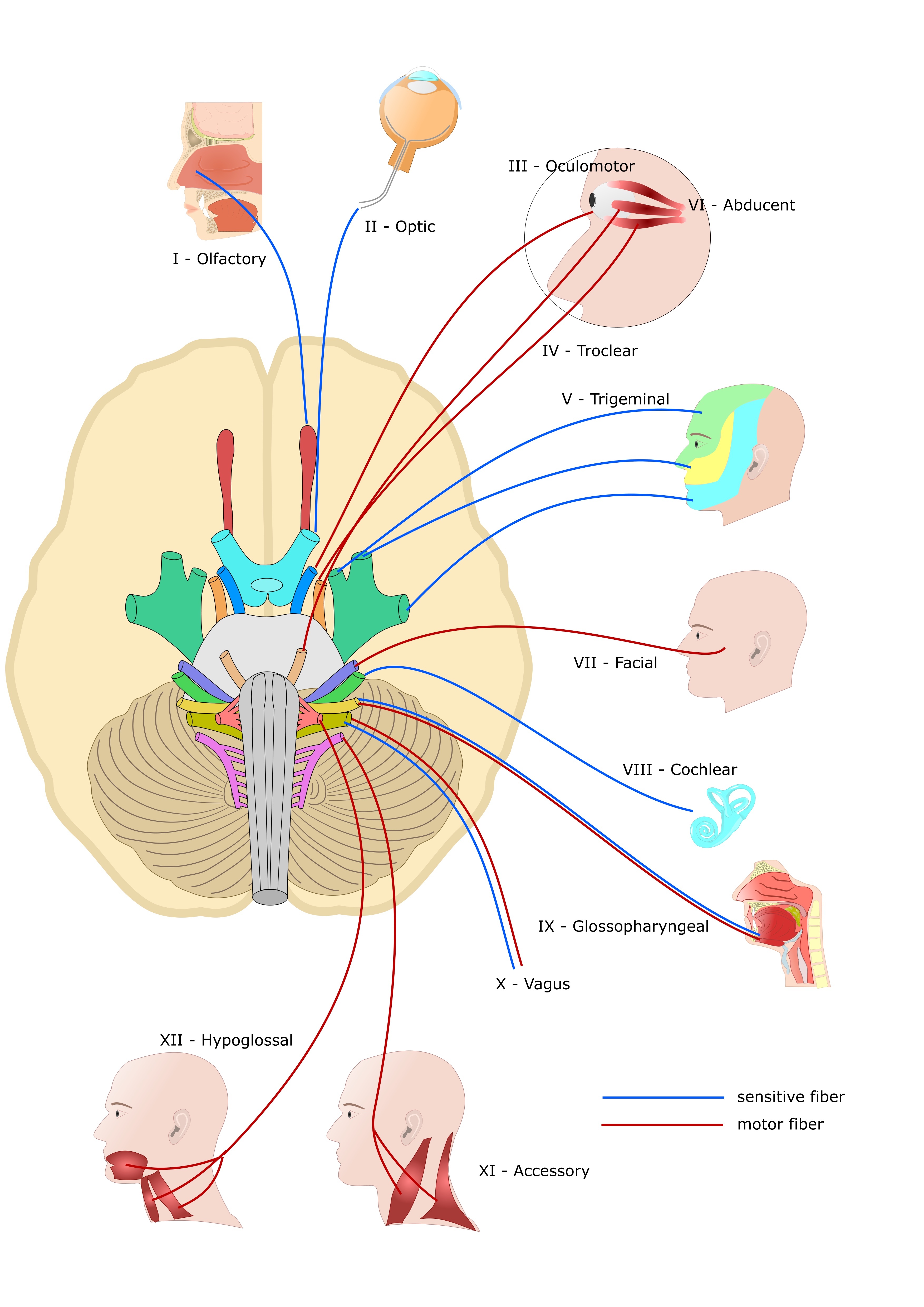
Otalgia or ear pain is a multifaceted condition categorized into primary and secondary otalgia. Primary otalgia originates directly from an ear pathology, while secondary otalgia results from referred pain from extraneous sources. The differential diagnoses and evaluation strategies are extensive due to the intricate neural network responsible for ear sensations. Cranial nerves V, VII, IX, and X, and cervical plexus branches C2 and C3, innervate the ear and adjacent structures. The auricle, ear canal, tympanic membrane, and middle ear all receive sensory input from these nerves, creating a complex network allowing for multiple different causes of ear pain. Understanding the relevant neural connections is pivotal for diagnostic accuracy and management effectiveness.
Cranial nerve V, encompassing ophthalmic, maxillary, and mandibular divisions, plays a crucial role in sensory innervation to the face, sinuses, palate, and teeth, making it a common culprit in dental and temporomandibular joint pathology. Cranial nerve VII, responsible for taste sensation and facial muscle control, is implicated in geniculate neuralgia when the nervus intermedius is inflamed. Cranial nerves IX and X contribute to otalgia through their connections to the oropharynx, larynx, and distant organs. The activity underscores the collaborative role of the interprofessional team in diagnosing and managing otalgia, considering the diverse neural pathways involved in this intricate sensory experience.
Objectives:
Differentiate the various conditions giving rise to primary and secondary otalgia.
Develop a clinically appropriate diagnostic plan for a patient with otalgia.
Create an individualized management strategy for a patient with otalgia.
Develop effective communication and coordination strategies within an interprofessional team to ensure optimal care and outcomes for patients with primary or secondary otalgia.
Introduction
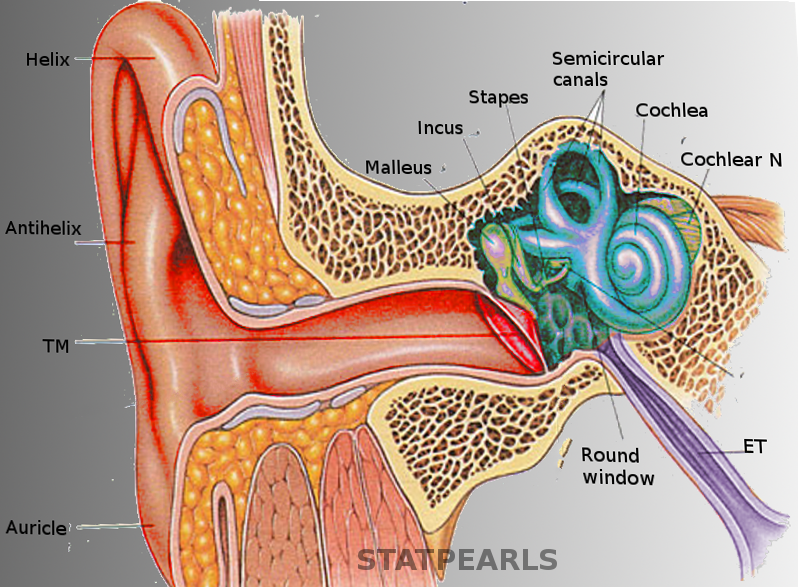
Otalgia or ear pain is divided into 2 broad categories based on etiology: primary and secondary otalgia. Primary otalgia is ear pain arising directly from inner, middle, or external ear pathology. Secondary or referred otalgia is ear pain from extraotic conditions. The ear receives sensory innervation from an intricate neural network due to the organ's complex embryologic development. The ear shares this neural network with other regional and distant organs, leading to numerous potential causes of referred ear pain (see Image. Ear Anatomy).[1]
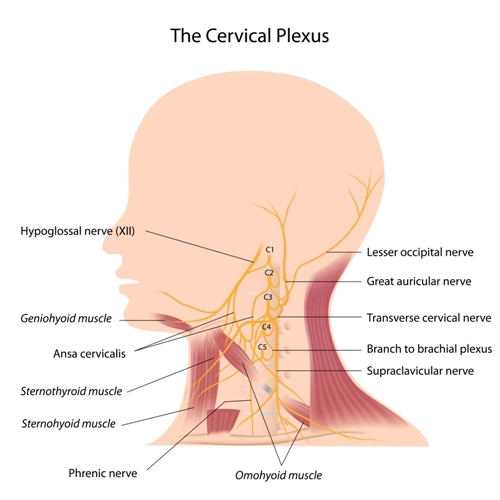
The trigeminal (cranial nerve V or CN V), facial (CN VII), glossopharyngeal (CN IX), and vagus (CN X) nerves and cervical plexus branches C2 and C3 all innervate the ear (see Images. Cranial Nerves & Cervical Plexus).[2][3]
- The auricle is innervated by cranial nerves V, VII, and X, and C2 and C3.
- The ear canal is innervated by cranial nerves V, VII, and X.
- The tympanic membrane is innervated by cranial nerves VII, IX, and X.
- The middle ear is innervated by cranial nerves V, VII, and IX.
Cranial nerves V, VII, IX, X, and C2 and C3 also supply organs outside the ear, resulting in multiple sources of referred ear pain.
- CN V is composed of the ophthalmic (V1), maxillary (V2), and mandibular (V3) divisions. The trigeminal nerve provides sensory innervation to the face, sinuses, palate, and teeth and controls the tensor tympani, tensor veil palatini, and mastication muscles. CN V's auriculotemporal branch innervates the temporomandibular joint (TMJ). This branch is most commonly implicated in TMJ dysfunction. Dental and TMJ pathology commonly cause secondary otalgia.
- CN VII provides taste sensation to the tongue's anterior two-thirds via the chorda tympani nerve and innervates the sublingual and submandibular salivary glands. The facial nerve also controls the stapedius, digastric posterior belly, stylohyoid, and facial expression muscles. The nervus intermedius is CN VII's sensory portion, innervating a part of the external auditory canal's skin and the nasal and nasopharyngeal mucosa. These fibers also carry taste sensations from the chorda tympani. Inflammatory nervus intermedius pain is known as geniculate neuralgia due to the nerve's synapse at the geniculate ganglion.
- CN IX provides taste and somatic sensation to the tongue's posterior third and afferents to the carotid body and oropharynx. The glossopharyngeal nerve also controls the stylopharyngeus muscle.
- CN X innervates the sinuses, thyroid gland, pharynx, and larynx. The vagus nerve's superior laryngeal branch innervates the vocal cords. The vagus nerve also innervates distant organs such as the heart, lungs, and parts of the gastrointestinal tract.
- C2 and C3 are cervical plexus branches innervating the auricular lobule, cervical paraspinal muscles, and posterior head.
Understanding the innervation patterns of these nerves helps in the differential diagnosis of otalgia and determining whether the pain originates from the ear itself or is referred from nearby structures. Accurate diagnosis based on the underlying etiology is essential for appropriate management and ear pain resolution.
Etiology
Both primary and secondary otalgia have extensive differential diagnoses, as discussed below. A comprehensive and systematic approach to otalgia evaluation is thus essential. Primary otalgia typically results from infectious, mechanical, neoplastic, or inflammatory causes. Secondary otalgia is best classified by organ system. Local and regional causes of referred otalgia include dental, temporomandibular, and pharyngeal pathology (see Image. Temporomandibular Joint Disorder). Distant etiologies include cardiac, gastrointestinal, and pulmonary pathology.
Epidemiology
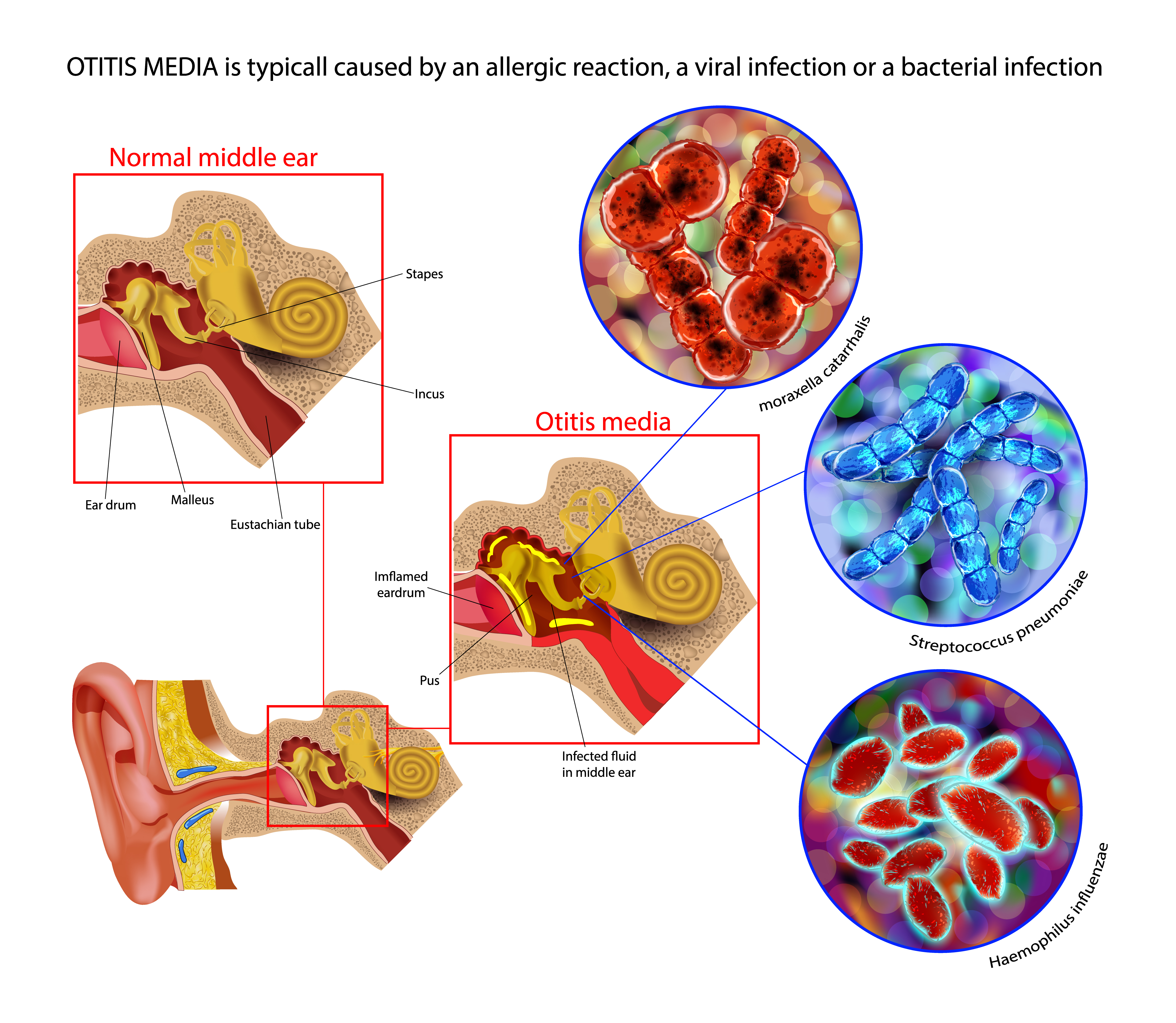
Ear complaints are relatively common reasons for presentation to primary care.[4] Primary causes are more common overall. Men are most commonly afflicted with primary otalgia, while women are more likely to have secondary otalgia.[5][6] Most pediatric otalgia cases are primary, with acute otitis media (AOM) being the most common. About 80% of children will have at least 1 otitis media episode before age 3.[7] AOM produces a significant disease burden in the United States. This condition accounted for 9.5% of all pediatric outpatient visits from 1997 to 1999.
Streptococcus pneumoniae is the most common cause of AOM. Pneumococcal conjugate vaccines 7 and 13 were approved in 2000 and 2010, respectively, to provide immunity against Streptococcus pneumoniae. Consequently, the percentage of outpatient AOM visits decreased from 9.5% to 5.5% between 2012 and 2014. AOM from non-typeable Haemophilus influenzae infection has become more frequent than AOM from type B Haemophilus influenzae infection, which currently has a vaccine.[8]
While primary otalgia is thought to be more common than secondary otalgia, some studies report that primary and secondary cases are equally frequent.[9] Adults and women with otalgia are more likely to have secondary causes. While the literature is inconsistent, TMJ, dental pathology, tonsillitis, and pharyngitis are cited as among the most common secondary otalgia causes.[10] However, Fenton et al reported in 2018 that mechanical neck and jaw disorders may be more frequent causes of referred otalgia.[11]
Patients older than 65 are more likely to experience otalgia from cervical spine disease. Women aged 20 to 40 are more likely to experience TMJ dysfunction.[12] Malignancies or distant secondary causes, such as thyroid, cardiac, gastrointestinal, or lung pathology, are rare but must be considered during patient examination, especially if medical history reveals risk factors.[13] Other secondary etiologies, such as petrous apicitis, malignant otitis externa, and Eagle syndrome, are also uncommon. However, migraine-associated otalgia is increasingly being recognized.[14]
Pathophysiology
Primary otalgia stems most commonly from infection. AOM is the most frequent primary otalgia cause in children (see Image. Acute Otitis Media Pathophysiology). The disease is typically associated with an upper respiratory tract infection that causes eustachian tube congestion and swelling. The eustachian tube narrows at the bony-cartilaginous junction, known as the isthmus, between the middle ear and the nasopharynx. Eustachian tube swelling at this location can impede or prevent middle ear drainage.[15] Collected middle ear secretions, known as an effusion, may lead to conductive hearing loss and potential bacterial growth, resulting in acute infection and pain.[16]
Chronic suppurative otitis media is the most common primary cause of otalgia in adults. The condition is a complication of eustachian tube dysfunction, similar to AOM. However, chronic suppurative otitis media is more likely to be a long-term problem requiring surgical management.[17] Infections can also directly affect the auricle or ear canal in perichondritis or otitis externa, respectively, leading to primary otalgia. Infection spread to the adjacent bone can cause petrous apicitis, mastoiditis, or malignant otitis externa.[18][19][20]
Secondary or referred otalgia occurs due to the ear's complex sensory nerve network. This nerve network also provides innervation to structures in the head and neck and distant sites, predisposing to referred pain when neurally connected distant sites are injured or inflamed. One theoretical mechanism of referred otalgia is the convergence-projection theory, which states that these nerves converge onto a shared neural pathway. Given the plethora of organs sharing the ear's innervation pathways, secondary otalgia can arise from many locations.
History and Physical
History
A comprehensive history and physical examination are critical when evaluating otalgia. The clinician must consider both primary and secondary causes. Table 1 summarizes the otalgia-associated features that may be elicited from the patient's medical history and their significance.
Table 1. Otalgia-Associated Historical Features and Their Significance
|
Key features of the present illness history
- Acute otalgia generally suggests benign causes. Insidious onset and chronic pain may suggest a sinister cause.
- Ear pain lasting longer than 4 weeks is more suspicious for malignancy, especially in the presence of risk factors and normal otoscopy.
- Ear fullness rather than ear pain may be more associated with cholesteatomas.
- Sharp, lancinating pain is more indicative of neuralgia or neuropathy.
- Unilateral than bilateral symptoms are more common in cases of malignancy.[21]
- Ear pain exacerbated by swallowing is suggestive of glossopharyngeal neuralgia.
- Pain at the "otalgia point" or the jugulodigastric region's apex is likely to be relieved after either myringotomy or nasal steroid usage if patients have normal physical examinations, tympanograms, and age-appropriate audiograms.[22]
- Otalgia may arise during the early postoperative phase of laryngeal or pharyngeal procedures, such as tonsillectomy.
|
|
Red flags associated with otalgia
- Dysphagia, odynophagia, dysphonia, or hemoptysis
- Loss of vision or black spots
- Unintended weight loss, chills, fevers, or night sweats
|
|
Risk factors for a life-threatening condition, such as malignancy
- Chronic smoking history
- A long history of excessive alcohol use, ie, approximately 3.5 or more drinks per day
- Previous human papillomavirus infection or risk thereof, ie, more than 10 oral sex partners
- Chronic immunosuppressed state, eg, diabetes mellitus and human immunodeficiency virus infection
|
Table 2 summarizes otalgia-associated symptoms that may signify referred pain and their possible origins.
Table 2. Referred Ear Pain-Associated Symptoms and Their Likely Origins
| Referred Pain Source |
Otalgia-Associated Symptoms |
| Chronic rhinosinusitis |
Nasal congestion |
|
Dental pathology
|
Toothaches |
|
Laryngeal pathology
|
Hoarseness |
| Gastroesophageal reflux |
Heartburn |
| Coronary artery disease |
Chest pain |
| Lung disease |
Shortness of breath |
| Cervical disc disease or myofascial pain |
Upper back pain |
|
Temporal (giant cell) arteritis
|
Headache, vision changes, malaise, jaw claudication |
Physical Examination
Ear examination is paramount, as this part of the physical examination identifies signs of ear infection or another primary ear pathology. Otoscopy may reveal vesicular lesions often found in herpes zoster oticus or, if facial paralysis co-occurs, Ramsay Hunt syndrome.
Nasal examination may show an inflamed nasal mucosa or nasal polyps. Anterior rhinoscopy may reveal chronic rhinosinusitis. Oral cavity examination may identify dental caries, loose fillings, aphthous ulcers, mass lesions, or abscesses. Intraoral palpation may also detect an elongated styloid process or calcified stylohyoid ligament, which can occur in Eagle syndrome.[23]
TMJ examination may demonstrate temporalis, lateral or medial pterygoid, or masseter muscle tenderness. This part of the physical examination may reveal trigger points or TMJ syndrome. Head examination may identify parotid or other salivary gland pathologies. Salivary gland tumors or sialadenitis may also be discovered. Tenderness along the path of the superficial temporal artery may indicate temporal arteritis.
Neck examination may uncover lymphadenopathy or thyroid gland pathology, which may indicate thyroiditis or lymph node metastasis. Fiberoptic nasopharyngoscopy may show upper aerodigestive tract lesions, such as nasopharyngeal and laryngeal tumors. Cervical spine examination may reveal musculoskeletal pathology, which may signify myofascial pain or cervical degenerative disc disease.
Cranial nerve examination may identify cranial nerve neuropathies, which may reveal trigeminal, geniculate, glossopharyngeal, sphenopalatine, occipital, or vagal neuralgia or Ramsay Hunt syndrome. Cervical spine, cardiac, pulmonary, and abdominal physical examinations may identify other sources of referred pain.
Evaluation
The first step in evaluating otalgia is a comprehensive clinical evaluation, encompassing a thorough history and physical examination. The ear examination is often enough to conclude whether otalgia is primary or secondary. However, a primary ear pathology should still be further evaluated to arrive at the correct diagnosis.
AOM is the most common cause of primary otalgia and is typically detected on simple otoscopy. Pneumatic otoscopy typically reveals opacification, bulging, and tympanic membrane immobility in most AOM cases. Evaluation beyond a comprehensive history and physical examination is rarely necessary for this condition unless red flags are present. Otitis externa is another frequent cause of primary otalgia. Bacterial infection of the external auditory meatus produces lesions that may be noted on visual inspection or otoscopy.
Eustachian tube dysfunction is a common otalgia cause often presenting with abnormal otoscopy findings. Tympanometry often demonstrates decreased tympanic membrane compliance or negative middle ear pressure. The Eustachian Tube Dysfunction Questionnaire (ETDQ-7) may also help determine the presence of eustachian tube dysfunction.[24] Audiometry should also be considered if hearing loss is present.
A normal otoscopic examination warrants a comprehensive evaluation for secondary ear pain sources. Clinical assessment should guide the need for laboratory or imaging studies. Dental and TMJ disorders are common sources of secondary otalgia. An orthopantomogram (panoramic x-ray) can provide a fast and easy way to view the jaw and all teeth fully. Imaging studies are not routinely required to evaluate a TMJ disorder.
Imaging studies such as head and neck computed tomography (CT) and magnetic resonance imaging (MRI), panendoscopy, including nasolaryngoscopy and direct visualization of the upper aerodigestive tract, may be performed if a serious condition cannot be ruled out by clinical examination alone. CT imaging of the temporal bone may help identify a possible petrous apicitis. CT and MRI imaging can also evaluate malignant otitis externa. A cranial nerve MRI may be obtained to determine cranial nerve neuropathies.
A biopsy can help rule out a head and neck malignancy, with tissue specimens taken from the primary site and suspicious lymph nodes. Imaging studies like CT and MRI can help determine the presence of metastasis.
A complete blood count can help screen for extraotic or systemic infection if the otoscopic examination is unremarkable. Nonsteroidal analgesics such as ibuprofen or acetaminophen may be prescribed to patients with no historical red flags, malignancy risk factors, and referred otalgia clinical signs. Specialty referral and advanced diagnostic studies should be considered if symptoms persist for longer than 4 weeks.
Gastrointestinal red flags should prompt a barium esophagram or referral to gastroenterology for esophagogastroduodenoscopy. Chest pain and cardiac risk factors warrant a complete cardiac evaluation. Clinical signs of temporal arteritis require laboratory studies, such as erythrocyte sedimentation rate or C-reactive protein levels. An erythrocyte sedimentation rate greater than 50 mm per hour indicates the need for an urgent ophthalmology and otolaryngology referral.
Treatment / Management
Treatment of otalgia depends on the diagnosis. Infections cause most primary otalgia and are treated with antibiotics. AOM associated with purulent conjunctivitis warrants the administration of amoxicillin with clavulanic acid, the drug of choice. Eustachian tube dysfunction is addressed with decongestants, nasal steroids, or myringotomy.
Secondary otalgia causes include various diagnoses, some of which require urgent management. Temporal arteritis is an example, needing prompt rheumatology referral and steroid administration. Therapy should otherwise address the underlying medical condition, such as malignancy, dental caries, TMJ dysfunction, coronary artery disease, or gastroesophageal reflux.
Differential Diagnosis
The differential diagnosis of primary and secondary otalgia includes a vast array of conditions, some of which are listed below. A thorough clinical evaluation and judicious use of diagnostic studies can help differentiate these conditions.
Primary Otalgia Differential Diagnosis
Infectious causes:
- Acute or chronic otitis media (see Image. Otitis Media on Otoscopy)
- Acute otitis externa (see Image. Otitis Externa)
- Bullous otitis externa or myringitis
- Auricular perichondritis
- Herpes zoster oticus, Ramsay Hunt syndrome
- Malignant otitis externa
Mechanical causes:
- Eustachian tube dysfunction
- Cerumen impaction
- Barotrauma
- Hematoma of pinna
- Auricular trauma
- Temporal bone fracture
- Foreign body in the external auditory canal
- Acute tympanic membrane perforation
Neoplastic causes:
- Squamous cell carcinoma (see Image. Squamous Cell Carcinoma)
- Basal cell carcinoma
- Melanoma
- Cholesteatoma
Inflammatory causes:
- Chondrodermatitis nodularis helicis
- Relapsing polychondritis
- Wegener granulomatosis/polyarteritis with granulomatosis (with associated serous otitis media)
Possible Reasons for Secondary Otalgia
- Head vascular pathology: temporal arteritis
- Sinus lesions: sinusitis, nasal polyps
- TMJ condition: TMJ dysfunction, bruxism
- Temporal bone pathology: petrous apicitis, Eagle syndrome
- Salivary gland conditions: sialadenitis, sialolithiasis, salivary gland tumor
- Oral cavity pathology: dental caries or other dental pathology, squamous cell carcinoma of the tongue
- Thyroid lesions: thyroiditis, thyroid carcinoma
- Neck conditions: carotidynia
- Lymphatic pathology: lymphadenopathy, lymph node malignancies
- Nerve conditions: trigeminal, glossopharyngeal, sphenopalatine, vagal, occipital, or geniculate neuralgia [9]
- Pharyngeal disorders: pharyngitis, oropharyngeal carcinoma, nasopharyngeal carcinoma, tonsillitis, posttonsillectomy pain, deep neck space abscess, tonsillolithiasis
- Laryngeal pathology: laryngitis, vocal cord dysfunction, laryngeal carcinoma
- Musculoskeletal disorders: myofascial pain, torticollis, cervical disc degeneration, cervical radiculopathy
- Lung disease
- Cardiac disease: myocardial infarction
- Gastrointestinal disease: gastroesophageal reflux disease, esophageal carcinoma
- Idiopathic or psychogenic
Prognosis
The prognosis of ear pain generally depends on the etiology, severity of the primary condition and associated symptoms, and timeliness and appropriateness of management. Both primary and secondary otalgia can arise from a wide variety of etiologies, most of which are readily treatable.
Complications
Acute and chronic pain, whether otic or not, can profoundly affect quality of life.[25][26] Severe otalgia may result in difficulty concentrating, loss of sleep, and a negative outlook. Complications from the underlying causes of otalgia should also be considered, as preventing or mitigating these conditions depends upon prompt recognition of the etiology.
For primary otalgia, complications may include hearing loss, tinnitus, vertigo, otorrhea, cranial neuropathies (eg, facial paralysis, facial numbness, diplopia), cerebrospinal fluid leak, and central nervous system involvement. Complications from secondary otalgia vary from nasal obstruction, endocrinopathy, and blindness to death from fatal causes like myocardial infarction and metastatic malignancy.
Deterrence and Patient Education
Ear pain can arise from various causes. Preventive measures for primary otalgia include practicing ear hygiene, wearing ear protection at work or during recreation, avoiding water entry into the ear, managing allergies, and preventing ear trauma, eg, from loud noises or excessively blowing the nose. Preventive measures for secondary otalgia depend on the primary cause. What can help generally are management of underlying conditions, treatment adherence, trigger avoidance, and regular health consultations. Other preventive measures to consider are explained below.
Primary Otalgia
Most cases of primary otalgia in children aged 6 to 24 months result from AOM, peaking between 9 and 15 months. Watchful waiting for 24 to 72 hours is reasonable before providing antibiosis to children without severe illness signs. The American Academy of Pediatrics has excellent guidelines for determining the appropriate treatment and the timing. Breastfed infants in their first 6 months of life have lower AOM rates than formula-fed infants. This phenomenon may result from infant position and pressure differentials during feeding.[27]
Secondary Otalgia
Secondary otalgia has an extensive differential diagnosis. The clinician must identify red flags that may indicate a possibly aggressive or fatal condition when evaluating patients with secondary otalgia. Regular dental exams every 6 to 12 months help prevent dental pathology, which may decrease the incidence of otalgia. Moderate-intensity exercise for 150 minutes every week may prevent cardiac pathology, which may also decrease the incidence of secondary otalgia.
Pearls and Other Issues
An important initial step when evaluating otalgia is distinguishing between primary and secondary sources, which significantly narrows down the differential diagnosis and speeds up management. Common primary causes of otalgia include otitis media, otitis externa, and eustachian tube dysfunction. Referred otalgia may result from extraotic conditions such as dental infections, temporomandibular joint disorders, pharyngitis, or cervical spine pathology. Certain red-flag symptoms associated with otalgia may indicate more serious underlying conditions and warrant further diagnostic testing.
Otalgia treatment depends on the underlying cause. For primary otalgia, management may include analgesics, antibiotics for infection, ear drops, or addressing contributing factors such as excessive cerumen. Referred otalgia requires addressing the underlying source, which may involve dental treatment, TMJ therapy, or management of pharyngitis or cervical spine issues. Appropriate follow-up for patients with otalgia must be ensured, particularly if symptoms persist or worsen despite treatment or if red-flag symptoms are present. Referral to specialists such as an otolaryngologist or dentist may be necessary for further evaluation and management.
Enhancing Healthcare Team Outcomes
Collaborative management involving healthcare professionals from various disciplines optimizes care and outcomes for patients with otalgia. However, the approach differs between primary and secondary cases.
Primary otalgia most commonly results from a local ear infection or inflammation and is generally addressed on an outpatient basis. The primary care physician and nurse provide the definitive treatment for patients with primary otalgia. A pharmacist's input regarding drug-drug interactions and dosages may be beneficial in more complicated cases, such as when the condition is compounded by allergy or antibiotic resistance. An otorhinolaryngologist may lend their expertise if the primary otic condition is complex and may require surgery.
Secondary otalgia often requires larger interdisciplinary care teams for comprehensive evaluation management. For example, TMJ dysfunction may require coordination between the primary care physician, pain clinic, and a dentist or oromaxillofacial surgeon. Dental pathology requires a dental referral. Chronic musculoskeletal conditions, such as cervical disc degeneration or trigger points, require care coordination involving physical therapy, pain management, and potentially orthopedic surgery. Malignancy necessitates the input of pathologists, radiologists, and surgical, medical, and radiation oncologists.
By bringing together healthcare professionals with diverse expertise and skills, patients receive holistic, personalized care addressing their physical, emotional, social, and psychological needs. Collaboration among team members fosters a culture of mutual respect, communication, shared decision-making, and continuous learning, ultimately leading to better patient outcomes.