Continuing Education Activity
Ophthalmometer or keratometer is an instrument used to measure the curvature of the anterior corneal surface and assess the extent and axis of astigmatism. Keratometry is the measurement of the curvature of the anterior corneal surface, usually across a fixed chord length of 2 to 3 mm, which falls within the spherical optic zone of the cornea. The principle of keratometry is that the anterior corneal surface behaves as a convex mirror and the size of the image change with the curvature. There are various clinical uses of keratometers, such as corneal astigmatism measurement, contact lens fitting, assessment of refractive error, IOL power calculation, etc. The keratometer readings may not always be perfect because of mistakes in keratometry. The activity deals with keratometers, keratometry principle, type of keratometers, clinical use, errors in keratometry, and clinical significance of keratometers.
Objectives:
- Describe how to perform keratometry.
- Review the interfering factors for a perfect keratometry.
- Summarize the indications of keratometry by using a keratometer.
- Explain the clinical significance of a keratometer.
Introduction
Keratometer or ophthalmometer is an instrument used to measure the anterior corneal curvature and the axis and extent of astigmatism.[1] The process of these measurements is called keratometry. Hermann von Helmholtz invented the first keratometer, and it came into vogue in 1851.[2] The earlier keratometer was designed by Jesse Ramsden and Everard Home in 1796. In keratometry, the measurements are performed at a fixed chord length of 2 to 3 mm, which falls within the spherical zone of the cornea.[3]
The keratometry is based on the principle that the anterior corneal surface behaves like a mirror and the image size varies with the corneal curvature. Hence the radius of curvature of the cornea can be calculated based on image size from the anterior corneal surface.[4]
In a keratometer, the relationship between the object, image, radius of refractive surface, and distance between the surface and object is denoted as r = 2ul/ o, where r is the radius of the reflective surface, o is the object size, l is the image size, and u is the distance measured between the reflective surface and object.[5] However, the exact measurement of image size poses a problem since it is difficult to entirely still a living eye while the image is being observed. The various type of manual keratometers can be Helmholtz keratometer, Bausch and Lomb, and Javal Schiotz keratometer.[6]
There can be surgical or operating keratometers as well as automated keratometers. The activity describes various types of keratometers, parts of a keratometer, indications of keratometry, limitations, complications, patient safety, education, and clinical significance of a keratometer.[7]
Procedures
Manual Keratometers
Helmholtz Keratometer
This consists of two plates. The image is displaced half of its length by both the plates, and total changes in distance or displacement give the size of the image. This doubling of the image helps with the necessity of not moving the living eye. If there is eye movement, the image will also move together during the process. Therefore, any difficulty in the adjustment of the eye is avoided. The plates used are made of glass and are a known thickness and refractive index. These plates are placed adjacent to each other so that each plate cover half of the object of a short telescope. The prime necessity is that the cylinder axis should coincide with the plane of separation of the glass plates. The glass plates can be inclined at an angle, and the angle of incident light can be varied and measured from a point in front.[2]
Bausch and Lomb Keratometer
This keratometer is based on the principle of constant object size and image size variability.[8]
Optics and Parts
Object: This is a circular mire with two plus and two minus signs. A bulb or a lamp is used to illuminate the mires with the help of mirrors placed diagonally. When light from the mire strikes the patient cornea, it produces a diminished image behind it. The image acts as an object for the rest of the optical system.
Objective lens: helps focus the light from the image of the mire (that acts as an object) along the central axis.[9]
Diaphragm and doubling prisms: A four aperture diaphragm is placed near the objective lens. Two doubling prisms are placed beyond the diaphragm, one having a base up and another a base out prism. The prisms can move independently and parallel to the central axis of the instrument. When light passes through the left diaphragmatic aperture, it is made to deviate by the base-up prism above the main optical axis. Similarly, when the light passes through the right diaphragmatic aperture, it is made to deviate by the base out prism, thus placing the second image to the right of the central axis. When light passes through the upper and lower aperture, it doesn't pass through the prism, and an image is produced on the axis.
The total area of combined upper and lower apertures is the sum of each aperture separately, but the brightness of the image is equal. The upper and lower apertures act as Scheiner's disc, doubling the image size. Hence this helps in continuous monitoring of the correct focus. The image doubling phenomenon is a unique phenomenon for Bausch and Lomb keratometer. Double images are produced adjacent as well as 90 degrees to each other; this helps in calculating the power of the cornea in two different meridians without any rotation of the instrument. Hence, this is also labeled as one position keratometer.[1]
Eyepiece: This lens helps get a magnified view of the doubled image.
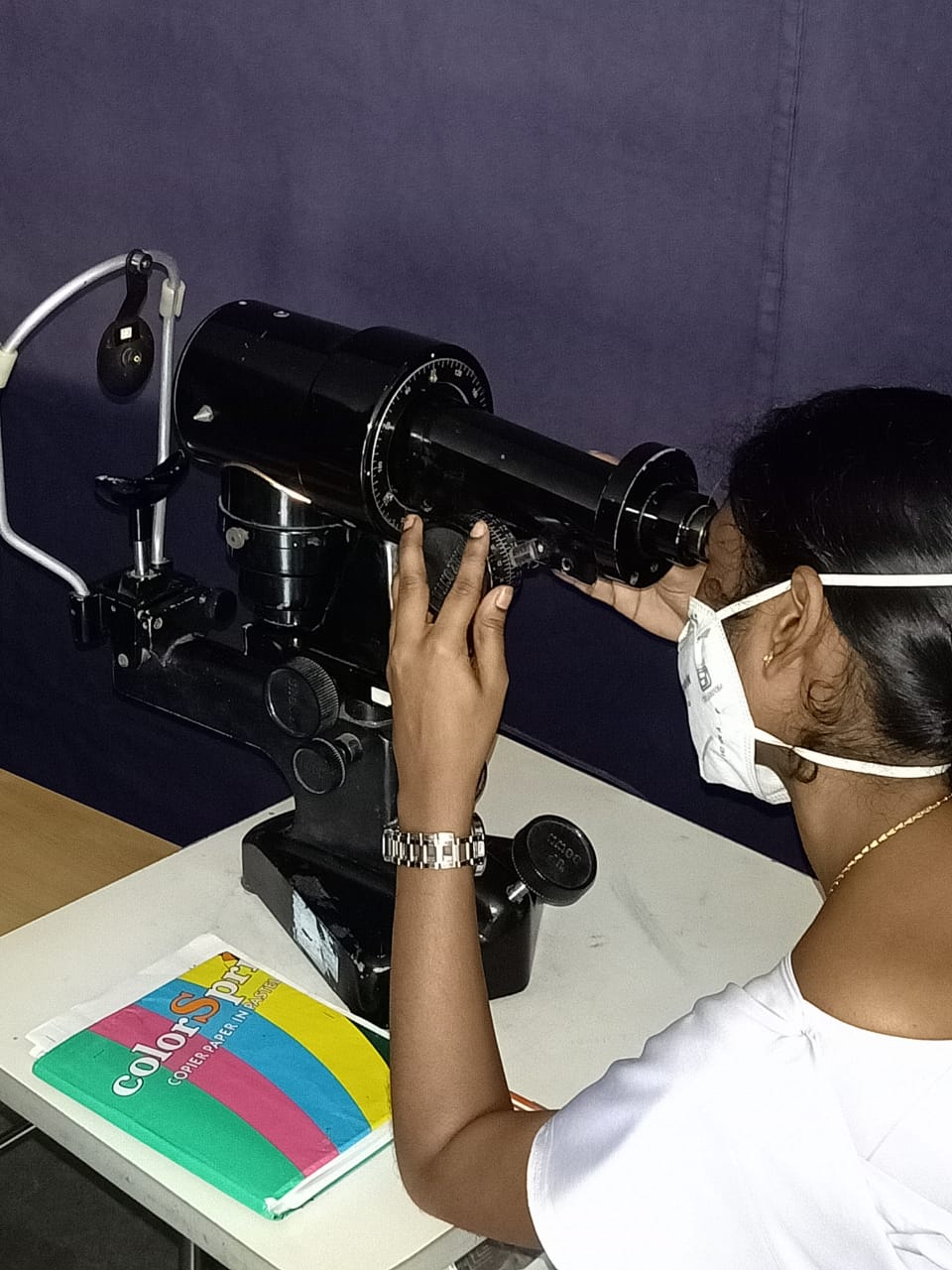
Keratometry Procedure
Instrument Calibration: The keratometer is calibrated with steel balls. A whiteboard is placed in front of the objective piece, and a black line is seen sharply focussed on it. The steel ball of the particular radius of curvature is used, the ball is placed in front of the keratometer, and the value is set on the scale. The mires are focussed on the hit and trial method by the anticlockwise and clockwise movement of the eyepiece. When the mires are focused, the instrument is said to be calibrated.[1]
Patient Adjustment: To obtain perfect keratometry, patient positioning is of utmost importance. The head should be against the headrest, and the chin should rest on the chin rest. An occluder should cover the other eye which is not being examined. This is followed by chin adjustment till the patient's pupil and the projective knob are at the same level.
Mire Focusing
After instrument calibration, alignment, and positioning of the patient, the mires are focused in the corneal center.
Corneal Curvature Assessment
The keratometer is focused on the corneal image so that there is no doubling of the central corneal image. To assess the curvature in the horizontal meridian, the plus sign of the central and left image is superimposed, taking into account the horizontal measuring control. Similarly, the central and upper images are taken into account for assessing the curvature in the vertical meridian. If there is oblique astigmatism, the two-plus signs will not be aligned. The instrument has to be then rotated till both plus signs are aligned.[10]
Javal Schiotz Keratometer
This instrument is based on variable object size and the constant image size principle.[11]
Optical and Parts
Object- This consists of two mires mounted on the arc which can be moved synchronously. The two mires combinedly form the object; hence the variable size is obtained by the movement. The first mire is stepped and has a green filter, and the other mire is rectangular and has a red filter. The mires are split in the center horizontally and are illuminated by a lamp. The first image obtained from the mires acts as an object for the rest of the optical axis.
The objective lens and doubling prisms
They form a doubled image of the new object (mires images created by the cornea). It uses a Wollaston prism which is a type of doubling prism. There is a fixed image doubling by the birefringent, also known as double refracting).[12]
Eyepiece Lens
It helps to obtain a magnified view of the doubled image.
The keratometry procedure of the Javal Schiotz keratometer is more or less similar to Bausch and Lomb keratometer.
Automated Keratometers
They are similar to manual keratometers. In this, the image reflected off the target is focused on the photodetector, which assesses the image size, and hence the radius of curvature is calculated. The mire is illuminated with the IR rays, and an infrared photodetector is used. The various advantages of automated keratometers are that they are compact, less time-consuming, and require less skill to operate.
The majority of the previous studies have found good accuracy using autokeratometry. In the market, the autokeratometers are available as isolated or autorefractometers of autokeratorefractometers. The various types of automated keratometers available are the IOL master, Pentacam, Orbscan, and corneal topographer.[13]
Surgical Keratometer
In this, the keratometers are attached to the microscope. The surgical keratometer helps in monitoring astigmatism while performing corneal and limbal procedures. However, the instrument has limited accuracy due to varied factors such as:
- It is challenging to align the visual axis of the patient with the optical axis of the keratometer.
- Anterior chamber air creates a second target reflection.
- The external compression on the globe results in a change in the corneal curvature.
- The calibrations for keratometers are for a fixed distance from the anterior corneal surface. Hence the different microscope lenses result in different working distances.[7]
Parts of Keratometer
- Headrest
- Chinrest
- Anteroposterior rotation axis scale
- Eyepiece
- Horizontal knob
- Vertical knob
- Focusing knob
- Locking knob
- Elevating knob
- Chin height knob
- Keratometer height knob
- Occluding shield
- Leveling sight
- Horizontal measuring drum
- Vertical measuring drum
- Axis scale[14]
Normal and Critical Findings
Relation Between Radius of Curvature and Power of Cornea
This is indicated by the following equation D= n-1/r, where D is the power of cornea in diameters, n is the refractive index of the cornea, and r is the radius of curvature. Ever since the invention of the keratometer by Helmholtz, the refractive index of the cornea has been 1.3375 for calibrating the instrument. Therefore the formula is read as D= 1.3375-1/r or 0.3375/r or r = 0.3375/D. Hence, the parameters of the keratometers are always labeled for the radius of curvature and dioptric power.[23]
Range of Keratometer
This ranges from 36 to 52 D (6.5 to 9.38 mm). The lower limit is 30D (5.6 mm), and the upper limit is 61 D (10.9 mm) using a lens of -1.0 D and +1.25 D, respectively, in front of the telescope's objective.[24]
Patient Safety and Education
Keratometry is a routine investigation in day-to-day clinical practice. Every patient must be educated regarding the keratometry procedure and the importance of doing it. The patient must be educated regarding the position and how to align themselves with the instrument. The patient should also be educated on how the mires appear.
Clinical Significance
An ideal keratometer can measure the radius in various meridians from the axis of the cornea. The keratometers are designed to be rotated along a particular axis. The objects are labeled as mires. A double device has been incorporated to avoid errors and confusion due to the continuous movement of the eyes.[32]
Spherical Cornea
This is characterized by no difference in power between the two principal meridians, and the mire appears as a perfect sphere.[33]
Astigmatism
This is characterized by the difference in the power between the two principal meridians. As with the rule of astigmatism, horizontally oval mires are seen. As against the rule of astigmatism, vertically oval mires are seen. In oblique astigmatism, the principal meridian lies between 30 and 60 degrees and 120 and 150 degrees. The irregular anterior corneal surface has irregular mires and a doubling of mires.[34]
Keratoconus
Inclination and jumping of mires are seen, also called pulsating mires. Minification of mires is seen in advanced keratoconus due to high myopia. Significant astigmatism shows oval mires. In advanced keratoconus, wavy, irregular, and distorted mires are also seen.[35]