Continuing Education Activity
Phacoemulsification is a modern cataract surgery first developed by Charles Kelman in 1967. The discovery of phacoemulsification came as a boon for the medical fraternity, where a cataractous lens could be emulsified through a small incision of 2-3 mm, giving perfect visual outcomes. There have been a lot of modifications to the current technique, but the basic technique of phacoemulsification remains the gold standard for cataract extraction. It involves the creation of a superior or temporal clear corneal incision of 2-3 mm, two side port incisions of at 2-3 clock hours on either side of the main wound. An ultrasonic probe is used to the trench, emulsify, and aspirate the cataractous lens from the main wound. The creation of small wounds revolutionized modern cataract surgery as it was self-sealing, astigmatically neutral, anatomically better-wound strength, and less incidence of complications. This also gave way to the concept of foldable IOL, wherein a foldable IOL can be implanted in the capsular bag through the smaller incision. Recent innovations have led to the development of micro-incisional cataract surgery (MICS), phakonit, and microphakonit. This activity gives insights into etiology, epidemiology, clinical evaluation by an interprofessional team, investigations needed, the technique, differential diagnosis, and complications of phacoemulsification.
Objectives:
- Describe the evaluation of a patient for phacoemulsification.
- Review the technique of phacoemulsification.
- Outline the complications associated with phacoemulsification.
- Explain the postoperative management of a patient with phacoemulsification.
Introduction
Cataract surgery is most commonly performed in the current era by utilizing the modern-day phacoemulsification technique. It helps to restore vision in patients developing cataracts due to any cause. Charles D Kelman first introduced phacoemulsification in 1948, and the concept was accepted in 1967. When Kelman first visited a dentist, he found dental enamel and debris being removed with ultrasound energy. Using a similar principle, he used a hollow 1 mm titanium needle with ultrasonic power to remove the lens at a speed of 40,000/s.[1]
Phacoemulsification also uses surgeon-guided automated irrigation and aspiration system to aspirate the cortex and nuclear fragments. There was initial reluctance to accept the technique due to the high incidence of complications and the need to enlarge the incision to accommodate the PMMA IOL. The technique became popular in 1980 due to various innovations like ophthalmic viscosurgical devices (OVDs), foldable IOL development, continuous curvilinear capsulorhexis, and improved quality and performance of phaco machines.[2]
While performing phacoemulsification, the ophthalmic surgeon makes a clear corneal incision with a 2.8 to 3.2 mm keratome along with two paracenteses. Then after staining the anterior lens capsule, capsulorhexis of the desired size is performed, and the nucleus is emulsified and aspirated through an ultrasonic phaco probe inserted through the main wound. Following this, the remaining cortical matter is removed from the capsular bag, and a foldable IOL is implanted. The surgery is performed under topical or local anesthesia or as an elective procedure, and the patient can be discharged the same day. Postoperatively on day 1, uncomplicated cases usually have a perfect visual outcome, and the vision gradually improves until 4 to 6 weeks as globe remodeling takes place.[3]
Anatomy and Physiology
The basic functioning of phacoemulsification depends on the irrigation and aspiration system.
Irrigation
Constant irrigation is an essential process in phacoemulsification by which fluid is passed through the sleeve of the phaco tip with minimal passage through the main incision; this helps maintain constant fluid dynamics inside the chamber. Coaxial irrigation helps cool down the ultrasound tip, minimize heat generation, and prevent tissue damage. Irrigation also helps to maintain a stable anterior chamber. The intraocular pressure and depth of the anterior chamber can be modified by changing the bottle height. Gravity plays a vital role in proving the force essential to maintain or increase irrigation. In some phaco machines, the irrigation pressure is supported by a collapsible saline bag. These bags are compressed with pressure plates, which help maintain a stable anterior chamber. Additionally, mydriatics can be instilled in the irrigation bottle to maintain pupillary dilatation during surgery.[4]
Aspiration
A thorough understanding of the aspiration system of a phaco machine plays a crucial role in improving the performance of surgeons' phacoemulsification. It is vital for performing various maneuvers during the surgery. Aspiration flow rate is when the nuclear or cortical matter is attracted towards the phaco tip. The surgeon should use the active fluidics inside the chamber to improve the efficiency of the surgery and the machine without damaging the adjacent tissue like the iris and capsule. Vacuum is a process that determines how tightly the nuclear or cortical matter is held in the aspiration port.[5]
Aspiration Pumps
Peristaltic Pumps (Flow-Based)
It employs flexible tubing mounted on a set of rollers that help push the fluid through the machine. The pressure difference is between the high-pressure chamber and low-pressure tubing build-up vacuum at the aspiration port of the ultrasound tip. The aspiration flow rate can also be linearly controlled by pressing the foot pedal to position 2, which increases the rollers' speed. A high AFR will result in nuclear pieces being attracted to phaco tip more readily. To prevent the collapse of the anterior chamber while surgery, the bottle height can be increased, and AFR can be reduced. The peristaltic flow system doesn't directly control the level of vacuum. Instead, the vacuum is dependent on AFR.
The vacuum is built by the resistance in the fluid circuit. When the tip is occluded by the nuclear material, in the absence of occlusion of the aspiration port, a high AFR will cause more nuclear material to be attracted to the port quickly. The vacuum rise time is defined as the time needed to achieve a particular vacuum level. A higher AFR will result in a faster vacuum rise time during occlusion. Modern phaco machines with peristaltic pumps do not have linear control of vacuum.[6]
Vacuum Pumps (Venturi Based)
The advantage of a vacuum pump is that it directly controls the vacuum level in the aspiration tubing by indirectly controlling the AFR. The pump work on the principle of the venturi effect, which creates a vacuum proportional to the rate of flow of gases. The AFR is built up the resistance of the fluid circuit. Hence, a higher vacuum will produce a higher AFR, rapidly attracting nuclear material to the port even in occlusion. The vacuum can be linearly controlled in the venturi pump by depressing the foot pedal to position 2.[7]
The following terminologies will help to understand pharmacodynamics in detail.
Aspiration Flow Rate
Aspiration flow rate is the fluid and lenticular material removal rate from the eye after passing through the tubing. AFR is quantified in mL/min. AFR occurs when the foot pedal is depressed from position 2 to 3. AFR determines how rapidly the lens fragments are attracted towards the aspiration port.[8]
Aspiration Port
This is an opening in front of the phaco probe, which helps remove saline and lenticular material from the eye.[9]
Compliance
Compliance determines how easily the tubings can be deformed with the help of a vacuum. High compliance has the property that it collapses more readily with vacuum than low compliance tubing, leading to excessive surge when the occlusion is broken.[10]
Followability
It determines how rapidly the lens material or fragments are attracted towards the aspiration port. Followability is dependent on AFR and can be made better by increasing the AFR and vacuum. It can be of two types- distal and proximal. Distal followability is the attraction of fragments towards the aspiration port, and proximal is how the port holds fragments.[11]
Infusion Pressure
It is the fluid pressure inside the tubings. It is dependent on bottle height (gravity-dependent) or intraocular pressure.[4]
Irrigation
It is the amount of fluid that is being influxed inside the eye, and it is governed by infusion pressure.[12]
Occlusion
It means blockage of the aspiration tubing or port that results in the vacuum build-up. The occlusion is broken when the lens matter is dislodged from the tubing or when the vacuum reaches the machine's pre-set value.[6]
Rise Time
It is time for the vacuum to rise once the aspiration port is occluded.[13]
Post-occlusion Surge
This phenomenon occurs when the occlusion is broken, and fluid moves from the anterior chamber (high-pressure zone) to aspiration tubing (low pressure). Surge can also lead to anterior chamber collapse and cause the iris and posterior capsule to be aspirated towards the port. It can be prevented by increasing fluid influx, alleviating vacuum, small diameter coiled tubing, and occlusion mode software.[14]
Vacuum
It is the amount of opposing suction force created in the tubing. It is measured in mmHg and is a determinant of how tightly the material will be held to the aspiration port.[15]
The following terminologies will help to understand ultrasound technology.
Cavitation
It means the formation of gas bubbles in the anterior chamber secondary to pressure changes at the phaco tip. The contraction and expansion of bubbles cause heat generation at the phaco tip causing emulsification of lens matter. Transient cavitation is better than continuous cavitation, which intermittent phaco energy delivery.[16]
Chatter
It is the repulsion of nuclear fragments at the phaco tip until the vacuum again reaches a level to neutralize the repulsive energy. Once the chatter is over, the vacuum similarly holds the nuclear material. A reduction in phaco power reduces the chatter.[17]
Duty Cycle
It is the ratio of power-on time to total time. Energy is calculated as power multiplied by time. Hence, energy depends on two components and can be varied by altering the time or the power.[18]
Frequency
It is the speed of movement of the phaco needle to and fro. The phaco ultrasound frequency is more than 20,000. The handpiece frequency is approximately 27000 to 60000 Hz.[19]
Power
This is the ability of the phaco needle to vibrate and break down the lenticular material. Power is dependent on stroke length, and it is the linear percentage of stroke length of the phaco needle. Power is produced in position 3 of the foot pedal.[19]
Stroke Length
It is the distance traveled by the phaco tip to cavitate the lens material. The normal stroke length is 0.05 to 0.10 mm (0.002 to 0.004).[20]
Indications
Phacoemulsification is indicated when the lens has become cataractous and results in reduced visual acuity. The various indications can be difficulty performing daily activities, decreased near or distant visual acuity, colored halos, photophobia, monocular diplopia, reduced contrast sensitivity, and white reflex in the pupillary area.[21]
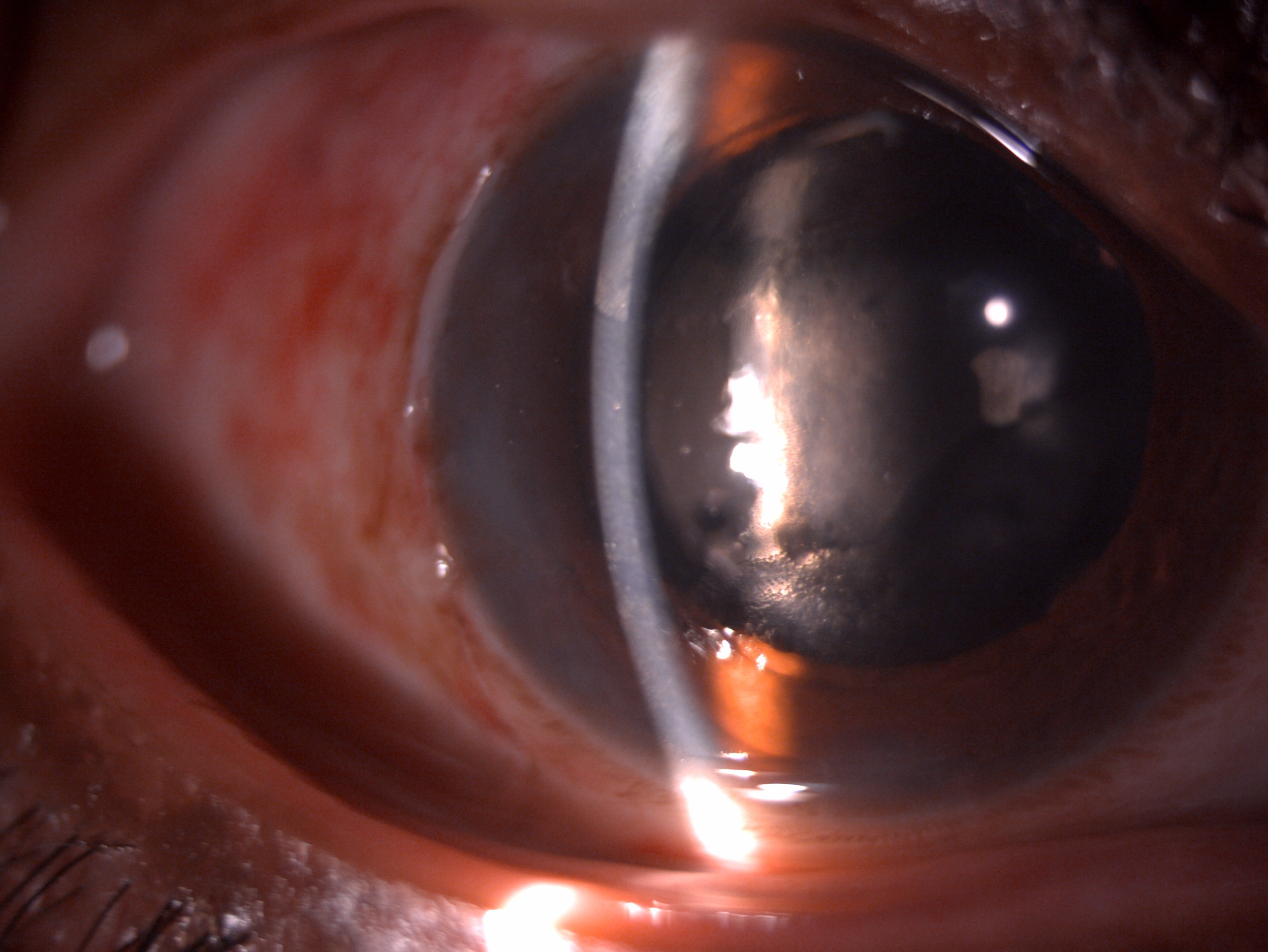
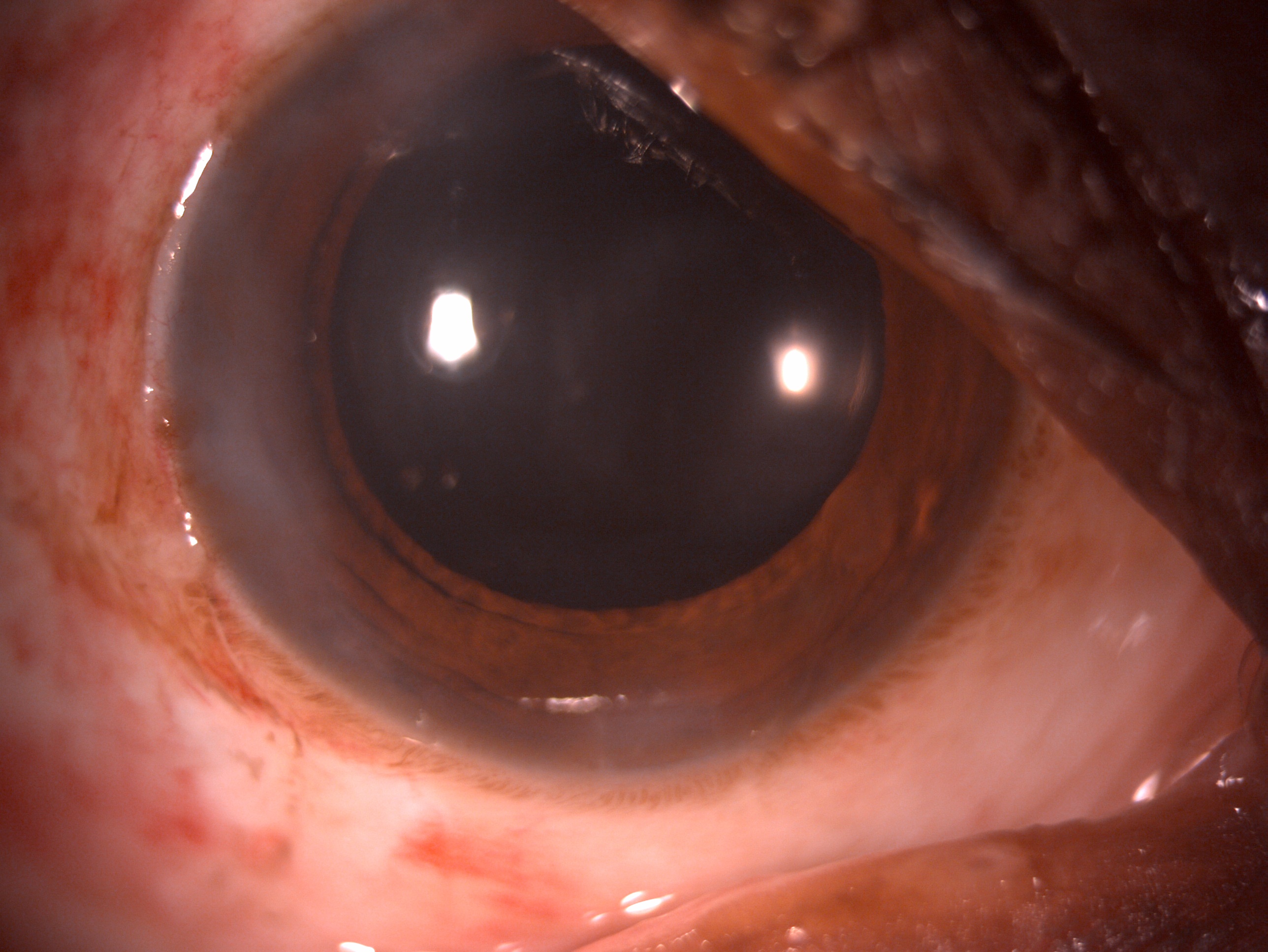
The various types of cataracts which require cataract surgery are posterior subcapsular cataract, nuclear cataract, cortical cataract, brown cataract, mature cataract, nuclear opalescence, traumatic cataract, posterior polar cataract, and subluxated cataract with capsular support devices. Some professions also desire perfect visual acuity with minimally acceptable standards like aviation, driving, armed forces, and operating complex equipment.[22]
Any type of cataract that compromises a patient's visual acuity is the main indication of phacoemulsification. The patients with cataracts often present with the blurring of vision, decreased visual acuity, glare, colored halos, monocular diplopia, decreased visual function, and altered contrast sensitivity. Cortical cataract has a moderate growth rate, produces moderate glare, and have a mild effect on near and distant vision. Nuclear cataract has a slow growth rate, produces mild glare, has a moderate impact on distant vision, and produce moderate induced myopia. In contrast, posterior subcapsular cataract variable growth rate produces marked glow and has a mild effect on distant vision and marked effect on near vision.[21]
The physical examination included assessment of the general physical condition of the patient to rule out systemic comorbidities like diabetes mellitus, hypertension, ischemic heart disease, chronic obstructive pulmonary disease, bleeding diatheses, adrenal suppression, Cushing disease, neurological problems like Alzheimer disease, and Parkinson disease. Any sensitivity to the drug must be ruled out, and a history of anticoagulants and antiplatelets should be noted. It is also imperative to note the history of systemic alpha a1-adrenergic antagonist medications like prazosin, terazosin, alfuzosin as they are associated with intraoperative floppy iris syndrome during cataract surgery.
It is also essential to document any allergy and adverse reaction to the drugs. A detailed anterior and posterior segment is mandated in each case subjected to cataract surgery. Anterior segment examination of lids to rule blepharitis, meibomian gland disease, trichiasis, distichiasis, and any other adnexal pathology, conjunctiva and sclera to rule out conjunctivitis, episcleritis, scleritis, any nodule or mass, corneal examination to rule out punctate epithelial erosions, guttae infiltrate or any corneal scar, anterior chamber depth assessment to rule angle-closure glaucoma, iris to look for any heterochromia, iris atrophy which may indicate past herpes infection, Koeppe or Busacca nodules, pupillary examination to rule out the persistent pupillary membrane, relative afferent pupillary defect, and posterior synechiae, festooned pupil, occlusio pupillae and seclusion pupillae, lens status to assess the grade and type of cataract and ocular motility assessment to rule out any nerve palsy.[23] A detailed fundus examination to rule diabetic retinopathy, hypertensive retinopathy, age-related macular degeneration, retinal detachment, or any other macular pathology.
Contraindications
Various contraindications for phacoemulsification include:
- The patient is not willing for surgery
- Multiple systemic comorbidities
- The patient doesn't desire surgery
- Happy patient having good visual acuity with glasses
- Surgery will not improve the vision
- The patient informed consent cannot be obtained
- Postoperative care is not possible[24]
Equipment
Phacoemulsification is a modern-day cataract surgery that employs ultrasound energy to emulsify the nucleus, vacuum to catch the nuclear material, and irrigation and aspiration for cortex and viscoelastic removal. A typical phaco machine consists of a handpiece, foot pedal, irrigation, and aspiration system. The working of the handpiece has been classically described as the jackhammer effect. The handpiece consists of piezoelectric crystals.[25]
These crystals' two and fro motion produces the mechanical energy for emulsifying the nucleus. The stroke length of the handpiece depends on the power of the machine. The to and fro motion results in compression, producing gas bubbles that help disassemble the nucleus. This process is known as cavitation. The vibrations of the tip can be longitudinal or torsional, which aid in the mechanical disassembly of the nucleus.[26]
The operator's command over the foot pedal is critical in determining a perfect visual outcome. All modern phaco machines have three positions in the foot pedal. Position 1 is for irrigation, 2 for irrigation and aspiration, and 3 for aspiration and ultrasound power. Power delivery can be fixed or variable. In fixed mode, the power delivery is fixed from 0 to 100%, while in variable mode, the depth of depression of the foot pedal determines the amount of energy delivered.[27]
Phaco Power Delivery
The phaco energy delivery in the eye can have favorable and disastrous outcomes. Cavitation and chatter can result in damage. The heat generation during phaco power can result in thermal injury to the endothelium. Hence, it is imperative to use phaco power judiciously and safely. Intermittent phaco power delivery can be used instead of continuous mode to safeguard the endothelium. The size and angle of the tip can also be changed to improve cutting efficiency. Torsional and elliptical movement of phaco tip also helps in reducing energy generation.[28]
Phaco Tip
Various tips are available with the bevel of 0, 15, 30, 45, and 60 degrees. A steeper bevel creates more holding force and higher cutting efficiency. The disadvantage is difficulty in achieving in a full vacuum. Phaco tip-end configuration can be bent, round, ellipsoid, or flared.[26]
Modes of Phaco Delivery
Pulse Modes
In this mode number of pulses per second are delivered with the foot pedal in position 3. There is also an off period during which no phaco power is delivered. The power of each pulse rises as the foot pedal is depressed further down to position 3. In position 3, maximum phaco power is delivered with each pulse.[29]
Burst-mode
Burst mode allows energy delivery of pre-set power (0-100%) separated by intervals of decreasing energy in position 3 of the foot pedal. When the foot pedal is fully depressed to position 3, the power is delivered in continuous mode rather than pulse mode. Burst mode helps in burring the tip in the lenticular matter and helps in chopping.[29]
Torsional Phacoemulsification
In this, the piezoelectric crystals within the handpiece create oscillatory movements, which are increased by using a Kelman-type bent tip. The high side-to-side motion helps in greater cutting efficiency and aids in easy nuclear disassembly.[29]
Elliptical Phacoemulsification
This uses combined transverse and longitudinal modes of phacoemulsification, resulting in an elliptical cutting pattern, increasing nuclear disassembly[29]
Preparation
Visual Acuity Testing
Snellen's distant uncorrected and best-corrected visual acuity assessment will document the visual potential. The near visual acuity must be separately tested with Snellen's chart or jaeger's chart. The visual acuity should be tested in an undilated state because the visual acuity may improve in the dilated state in the posterior subcapsular cataract. In the case of a mature and brown cataract with visual acuity of hand motion or less, the perception of light and projection of rays should be documented to assess the visual potential of the eye.[30]
Refraction
Careful retinoscopy and refraction must be performed for all the patients requiring cataract surgery. Refraction is necessary to know the required IOL power and assess if any myopic shift has occurred postoperatively. If the other eye lens is clear and has high refractive error, targeting emmetropia may result in the problem of postoperative anisometropia. In such scenarios, the patient should be explained the need for refractive surgery or the use of a contact lens.[31]
Glare Testing
Glare testing help to assess the degree of the visual impairment of a patient with the use of a light source located in the visual field.
Contrast Sensitivity Testing
Contrast sensitivity may be diminished even in patients with Snellen visual acuity of 6/6. Contrast sensitivity can be tested with various specialized charts available.[32]
IOL Biometry
Conventional SRK Formula
P=A-2.5L-0.9K
where
- P= power of the lens in dioptres
- L= Axial length in mm
- K- Average keratometry reading in dioptres
- A – Constant of implant
Recently available biometry instruments are IOL master 500 and 700 to determine the IOL power.[33]
The other available biometry formulas are Hoffer Q which is more suitable for short axial lengths, while SRK/T and Haigis formula for longer axial lengths. The recently introduced 4th generation formulas like Holladay 2, Haigis, Barrett, True-K and Olsen and Hill-RBF. Many surgeons use multiple formulas to finalize the final IOL power. The American Society of Cataract and Refractive Surgeons (ASCRS) also provides an open free IOL power calculator online for the benefit of surgeons.[34]
Special Tests
Potential Acuity Meter
This method can assess vision loss due to cataractous changes. This method is helpful in patients with visual acuity of more than 6/60 without any ocular pathology. In this test, the patient is told to read the brightly illuminated near card through a pinhole. The other available meter is the Retinal Acuity Meter. In some cases, PAM can be misleading with pre-existing pathologies like age-related macular degeneration, amblyopia, secondary glaucoma, macular pathologies like scar and edema, and retinal detachment.[35]
Visual Field Evaluation
It is imperative to screen visual fields with confrontation testing in all patients planned for cataract surgery. The visual field evaluation is not mandatory in all patients. Visual field testing is indicated in patients with pre-existing glaucoma, optic nerve abnormality, or retinal pathology. This testing modality can pick up early field loss and vision loss due to abnormalities other than cataracts. Filed loss induced due to cataract improves after cataract removal.[36]
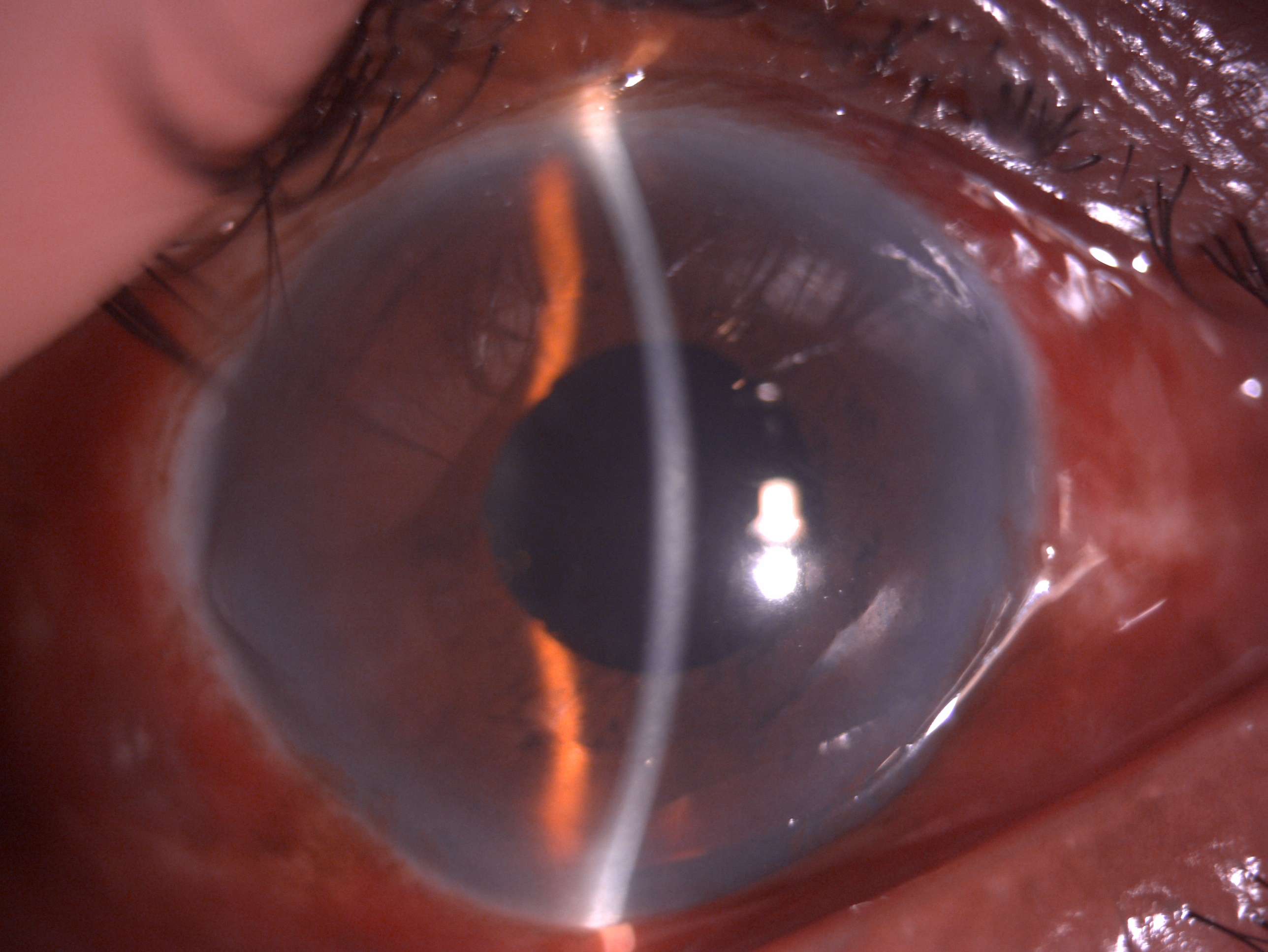
Specular Microscopy
A clinical picture of cornea guttae (Fuch dystrophy) in a cataract patient mandates specular microscopy to assess the endothelial status. The other indications for specular microscopy can be endothelial dystrophies, trauma, previous intraocular surgery, and patients planned for combined surgery like DSEK with cataract extraction. This helps in counseling the patients regarding the risk of corneal decompensation. Cataract surgery results in endothelial cell loss. Hence patients with low endothelial cell count should be operated on with soft shell technique under guarded prognosis.[37]
Pachymetry
Pachymetry is an indirect way to assess the corneal endothelial status. Patients with a higher central corneal thickness of more than 640 um are at increased risk of corneal decompensation.[38]
Macular Function Tests
Optical coherence tomography helps assess macular statuses like edema, holes, vitreomacular traction, and adhesions. Various surgeons are increasingly using it before putting the patients for cataract surgery.[39]
Technique or Treatment
Conventional Steps of Phacoemulsification
Marking the Eye and Time-Out
Before starting the surgery, it is essential to mark the eye with a pen or sticker to avoid operating on the wrong eye. The marking can be a tick or a cross, or a circle. The mark can be placed above the eyebrow or below the cheek. The time out is when the surgeon reviews the patient details like name, place, age, correct eye, and IOL power to avoid mistakes while operating.
Globe Exposure
After draping and administering anesthesia to the eye, a speculum should be applied to hold the eyelids apart. The speculum should be applied wide enough to allow easy instrumentations. The surgeon can operate from the superior side or temporal side. The axis of astigmatism should also be considered while placing the incision as it needs better exposure in that area.[40]
Side Port Incisions (Paracentesis)
Side port incisions are made on either side approximately 2 to 3 clock hours from the main precise corneal incision. The paracentesis is performed with a 15-degree blade or MVR blade. The paracentesis is helpful for insertion of the second instrument like rhexis needle, viscoelastic, iris hooks, rhexis forceps, and other intracameral additives. The incisions are made parallel to the iris plane.[41]
Clear Corneal Incision
The clear corneal incisions are placed temporally or superiorly approximately 2.2 to 3.2 mm wide. The incision is large enough to accommodate the handpiece of phaco and IOL. The objective of establishing a clear corneal incision is that it should be self-sealing, water-tight without any leakage, and minimizes astigmatism during the surgery. There should be minimal manipulation of the incision to fish mouthing of the incision, and care should be taken to avoid wound burn from the phaco probe. The incision can be uniplanar, biplanar, or tri-planar.
Sclerocorneal Tunnel Incision
A sclerocorneal tunnel incision is used when PMMA rigid IOL insertion is planned, or there is a need to convert a clear corneal phaco to sclerocorneal during a complication. One advantage of this incision is that it reduces surgically induced astigmatism.
Continuous Curvilinear Capsulorrhexis (CCC)
After a clear corneal incision, the next step is to perform a rhexis to expose the lens for emulsification. CCC helps the surgeon to stabilize the nucleus, perform controlled maneuvers inside the capsular bag, prevent radial tears and rhexis run out. The ideal size of CCC for phacoemulsification is 5 to 5.5 mm to accommodate a 6 mm optic of the IOL.[42] A tight contact between the IOL and anterior lens capsule will reduce PCO incidence. The CCC has usually performed with a bent 26 G needle the cystitome or rhexis forceps under cover of viscoelastic.
Hydrodissection
This is one of the most critical steps in phacoemulsification to separate the cortex from the posterior capsule. A correctly performed hydro dissection will facilitate nucleus rotation, trenching, and nuclear breakdown. Hydrodissection is performed using a 2 ml or 5 ml syringe with a 25-30 G cannula. After lifting the capsular flap, saline-injected to separate the cortex from the capsule. The passage of a wave of dissection from one end to the other indicates adequate hydrodissection. In a mature and sometimes brown cataract, the nucleus is free from the cortex, and there is no need to perform a hydrodissection.[43]
Hydrodelineation
This separates the endonucleus from the epinucleus and is indicated in posterior polar cataract cases. The separation of endonucleus from epinucleus creates a golden brown ring. Hydrodelineation has a limited role in phacoemulsification.[44]
Nuclear Rotation
After an adequate hydrodissection, nucleus rotation becomes accessible within the capsular bag. When the nucleus rotates freely, it becomes easier to perform divide and conquer, stop and chop, and direct chop techniques of phaco. If the dissection is not proper, it will stress the zonules and result in zonular dialysis.[45]
Techniques of Nucleus Break and Removal
The various steps include pre-phaco, sculpting, trenching, cracking, chopping, holding, and emulsification.
Plane of Phacoemulsification
The plane of phacoemulsification can be the posterior chamber, iris plane, or anterior chamber.
Posterior Chamber
The nucleus cracking and emulsification is performed in the posterior chamber. The significant advantage is less risk and trauma to the corneal endothelium. The disadvantage is the risk of posterior capsular rent.
Iris Plane
The nucleus is prolapsed anteriorly, and phaco is performed at the iris plane. This technique is helpful for beginner phaco surgeons and in cases with pre-existing zonular weakness. The disadvantage is being closer to the endothelium may result in endothelial damage.
Anterior Chamber
This is also known as the suprascapular approach. In this, the nucleus is prolapsed in the anterior chamber and emulsified in the anterior chamber. This is advantageous in cases of posterior capsular rupture and cases with zonular weakness. The disadvantage is the risk of endothelial trauma and a high chance of aspirating the iris tissue. It is recommended to coat the endothelium with viscoelastic before performing anterior chamber phacoemulsification[46]
Techniques of Nucleus Cracking
Divide and Conquer Nucleofractis
Divide and conquer nucleofractis is a valuable technique for all cataracts except very soft nuclei. In this, a deep central groove is made in the form of a plus sign of adequate depth to facilitate bimanual mechanical cracking. Signs of adequate depth include the appearance of a red glow, a deep grove of 2-3 phaco tip diameter, and loss of striations.[47]
Stop and Chop
In this technique, a central deeper linear groove is made. The nucleus is divided into two heminuclei by mechanical cracking using a Sinskey chopper in the left hand and a phaco probe in the right hand.[48]
Direct Chop
In this technique, a central deep crater is formed. The nucleus is cracked into multiple pieces by engaging the phaco probe deep in the nuclear material under a high vacuum and mechanically cracking the piece with a Sinskey hook.
Chopping Techniques
Horizontal Chop
In this technique, the central groove is not fashioned. The phaco probe is deeply buried in the center of the nucleus under a high vacuum, and the chopper or a sinskey hook is inserted in the endonucleus under the anterior lens capsule and brought towards the central phaco tip. This, in turn, facilitates cracking.[49]
Vertical Chop
In this technique, the phaco tip is buried deeply in the central part of the nucleus, and the chopper is impaled adjacent to the phaco tip. The phaco tip is lifted slightly, and the chopper is depressed and nuclear pieces are cracked.[50]
Irrigation and Aspiration (I/A)
Irrigation and aspiration is a technique for the removal of epinucleus and cortical matter from the capsular bag. Coaxial I/A or bimanual I/A can perform this. A bimanual Simcoe cannula can also be used to remove the cortex. This technique is also helpful for polishing the capsule and removal of viscoelastic after putting IOL in the bag.[51]
IOL Implantation
The final step in phacoemulsification is the insertion of a foldable IOL with the help of IOL injectors. In uncomplicated cases, the aim is to place the IOL in the capsular bag. However, IOL can be easily implanted in the sulcus with sufficient capsular support in case of a complication. The IOL implantation should be performed under liberal viscoelastic cover. After implantation, the viscoelastic is removed with I/A to avoid secondary glaucoma. This is followed by anterior chamber formation and injection of intracameral moxifloxacin.
Complications
Intraoperative
- Wound leak
- Wound dehiscence
- Wound burn
- Descemet membrane detachment[52]
- Corneal burn
- Iridodialysis
- Rhexis extension
- Zonular dialysis
- Posterior capsular tear
- Nuclear drop
- Retained Cortex
- Vitreous prolapse
- Choroidal detachment
- Retinal detachment[53]
Postoperative
- Wound leak
- Astigmatism[54]
- Striate Keratopathy
- Corneal edema
- Pupillary block
- Uveitis
- IOL decentration
- IOL tilt
- IOL subluxation
- IOL dislocation[55]
- Vitreous wick syndrome
- Vitreous touch syndrome
- Endophthalmitis
- Toxic anterior segment syndrome
Clinical Significance
Modern-day phacoemulsification has revolutionized cataract surgical outcomes. With the advent of innovative and premium intraocular lenses, cataract surgery has become the most commonly performed refractive surgery worldwide. The patient expectations and surgeon expertise and skill have also increased. Every eye deserves the best, and it is the duty of all cataract surgeons to perform the surgery ethically and give a perfect visual outcome. The patient should be educated about the risk and benefits of cataract surgery. The patient should be educated regarding the benefits of modern-day phacoemulsification.[56]
The clinician should help the patient fully understand the phacoemulsification technique, the types of foldable and premium intraocular lenses available, and which lens will benefit the patient most. In addition, in case of risk factors like Fuch's dystrophy, compromised endothelium, or small pupil cases, the patient should receive counsel regarding the need for additional instruments and devices like iris hooks and viscoelastic devices. In case of any intraoperative complication, the patient should be described in detail the intraocular mishap and what best can be done intraoperative or postoperatively to achieve a perfect visual outcome.
Any patient requiring cataract surgery must be examined in detail by an ophthalmologist. Patients with high-risk factors for cataract surgery like pseudoexfoliation, limited pupillary dilatation, zonulopathy, history of uveitis, narrow-angle and shallow anterior chamber, subluxated cataractous lens, corneal opacity, secondary glaucoma, retinitis pigmentosa, etc. can be referred to a cataract and IOL surgeon with the skilled expertise to manage such cases. A vitreoretinal surgeon should evaluate patients landing with intraoperative complications like zonular dialysis, posterior capsular tear, and vitreous prolapse postoperatively to rule out nucleus or cortex drop in the vitreous cavity other dreaded complications like retinal and choroidal detachment.[57]
Enhancing Healthcare Team Outcomes
Phacoemulsification has evolved ever since its inception from anterior segment phaco to pupillary plane to posterior chamber phacoemulsification to safeguard the corneal endothelium, minimize complications and give a perfect postoperative visual outcome. The ophthalmic cataract surgeons and researchers have a crucial role in determining the ideal outcome.
The nursing team plays a crucial role in preoperative investigations, counseling, intraoperative patient preparation, surgeon's assistance, postoperative patient counseling, and follow-up. The pharmacists also play a vital role in supplying the essential topical medications and guidance of the patients. In case of any complications, the vitreoretinal surgeon also plays an essential role in assessing the retinal status and need for retinal surgery like pars plana vitrectomy and lensectomy. In a nutshell, a multidisciplinary, coordinated effort is required for a perfect outcome after phacoemulsification.[58]