[1]
Pasadhika S, Rosenbaum JT. Ocular Sarcoidosis. Clinics in chest medicine. 2015 Dec:36(4):669-83. doi: 10.1016/j.ccm.2015.08.009. Epub
[PubMed PMID: 26593141]
[2]
Ikonomopoulos JA, Gorgoulis VG, Kastrinakis NG, Galanos AA, Karameris A, Kittas C. Experimental inoculation of laboratory animals with samples collected from sarcoidal patients and molecular diagnostic evaluation of the results. In vivo (Athens, Greece). 2000 Nov-Dec:14(6):761-5
[PubMed PMID: 11204496]
Level 3 (low-level) evidence
[3]
Heyll A, Meckenstock G, Aul C, Söhngen D, Borchard F, Hadding U, Mödder U, Leschke M, Schneider W. Possible transmission of sarcoidosis via allogeneic bone marrow transplantation. Bone marrow transplantation. 1994 Jul:14(1):161-4
[PubMed PMID: 7951107]
[4]
Agrawal R, Kee AR, Ang L, Tun Hang Y, Gupta V, Kon OM, Mitchell D, Zierhut M, Pavesio C. Tuberculosis or sarcoidosis: Opposite ends of the same disease spectrum? Tuberculosis (Edinburgh, Scotland). 2016 May:98():21-6. doi: 10.1016/j.tube.2016.01.003. Epub 2016 Jan 18
[PubMed PMID: 27156614]
[5]
Eishi Y. Etiologic link between sarcoidosis and Propionibacterium acnes. Respiratory investigation. 2013 Jun:51(2):56-68. doi: 10.1016/j.resinv.2013.01.001. Epub 2013 Mar 17
[PubMed PMID: 23790733]
[6]
Newman KL, Newman LS. Occupational causes of sarcoidosis. Current opinion in allergy and clinical immunology. 2012 Apr:12(2):145-50. doi: 10.1097/ACI.0b013e3283515173. Epub
[PubMed PMID: 22314258]
Level 3 (low-level) evidence
[7]
Kucera GP, Rybicki BA, Kirkey KL, Coon SW, Major ML, Maliarik MJ, Iannuzzi MC. Occupational risk factors for sarcoidosis in African-American siblings. Chest. 2003 May:123(5):1527-35
[PubMed PMID: 12740270]
[8]
Kreider ME, Christie JD, Thompson B, Newman L, Rose C, Barnard J, Bresnitz E, Judson MA, Lackland DT, Rossman MD. Relationship of environmental exposures to the clinical phenotype of sarcoidosis. Chest. 2005 Jul:128(1):207-15
[PubMed PMID: 16002937]
[9]
Barnard J, Rose C, Newman L, Canner M, Martyny J, McCammon C, Bresnitz E, Rossman M, Thompson B, Rybicki B, Weinberger SE, Moller DR, McLennan G, Hunninghake G, DePalo L, Baughman RP, Iannuzzi MC, Judson MA, Knatterud GL, Teirstein AS, Yeager H Jr, Johns CJ, Rabin DL, Cherniack R, ACCESS Research Group. Job and industry classifications associated with sarcoidosis in A Case-Control Etiologic Study of Sarcoidosis (ACCESS). Journal of occupational and environmental medicine. 2005 Mar:47(3):226-34
[PubMed PMID: 15761318]
Level 2 (mid-level) evidence
[10]
Rossman MD, Thompson B, Frederick M, Maliarik M, Iannuzzi MC, Rybicki BA, Pandey JP, Newman LS, Magira E, Beznik-Cizman B, Monos D, ACCESS Group. HLA-DRB1*1101: a significant risk factor for sarcoidosis in blacks and whites. American journal of human genetics. 2003 Oct:73(4):720-35
[PubMed PMID: 14508706]
[12]
Calender A, Weichhart T, Valeyre D, Pacheco Y. Current Insights in Genetics of Sarcoidosis: Functional and Clinical Impacts. Journal of clinical medicine. 2020 Aug 13:9(8):. doi: 10.3390/jcm9082633. Epub 2020 Aug 13
[PubMed PMID: 32823753]
[13]
Iannuzzi MC. Genetics of sarcoidosis. Seminars in respiratory and critical care medicine. 2007 Feb:28(1):15-21
[PubMed PMID: 17330189]
[14]
Rybicki BA, Major M, Popovich J Jr, Maliarik MJ, Iannuzzi MC. Racial differences in sarcoidosis incidence: a 5-year study in a health maintenance organization. American journal of epidemiology. 1997 Feb 1:145(3):234-41
[PubMed PMID: 9012596]
[15]
Baughman RP, Field S, Costabel U, Crystal RG, Culver DA, Drent M, Judson MA, Wolff G. Sarcoidosis in America. Analysis Based on Health Care Use. Annals of the American Thoracic Society. 2016 Aug:13(8):1244-52. doi: 10.1513/AnnalsATS.201511-760OC. Epub
[PubMed PMID: 27509154]
[16]
Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. The New England journal of medicine. 2007 Nov 22:357(21):2153-65
[PubMed PMID: 18032765]
[17]
Rothova A, Alberts C, Glasius E, Kijlstra A, Buitenhuis HJ, Breebaart AC. Risk factors for ocular sarcoidosis. Documenta ophthalmologica. Advances in ophthalmology. 1989 Aug:72(3-4):287-96
[PubMed PMID: 2625091]
Level 3 (low-level) evidence
[18]
Yemm RW, Pecen PE, Fliney GD, Palestine AG. Chest X-ray and Uveitis Evaluation in a Population with Low Incidence of Sarcoidosis. Ophthalmology and therapy. 2020 Sep:9(3):577-584. doi: 10.1007/s40123-020-00274-6. Epub 2020 Jul 1
[PubMed PMID: 32613593]
[19]
Varron L, Cottin V, Schott AM, Broussolle C, Sève P. Late-onset sarcoidosis: a comparative study. Medicine. 2012 May:91(3):137-143. doi: 10.1097/MD.0b013e3182569f91. Epub
[PubMed PMID: 22543629]
Level 2 (mid-level) evidence
[20]
Shetty AK, Gedalia A. Childhood sarcoidosis: A rare but fascinating disorder. Pediatric rheumatology online journal. 2008 Sep 23:6():16. doi: 10.1186/1546-0096-6-16. Epub 2008 Sep 23
[PubMed PMID: 18811966]
[21]
Patterson KC, Chen ES. The Pathogenesis of Pulmonary Sarcoidosis and Implications for Treatment. Chest. 2018 Jun:153(6):1432-1442. doi: 10.1016/j.chest.2017.11.030. Epub 2017 Dec 7
[PubMed PMID: 29224832]
[22]
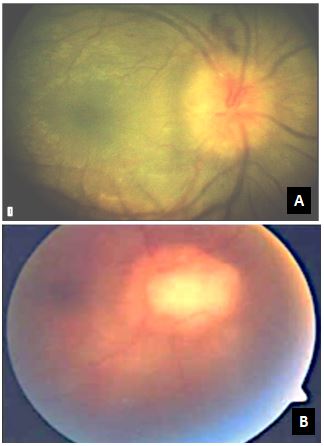
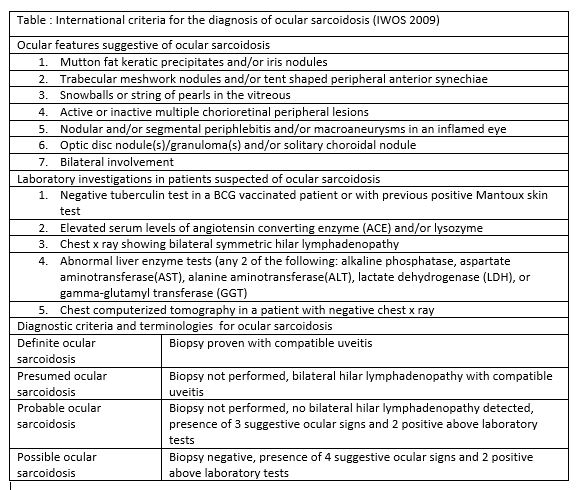
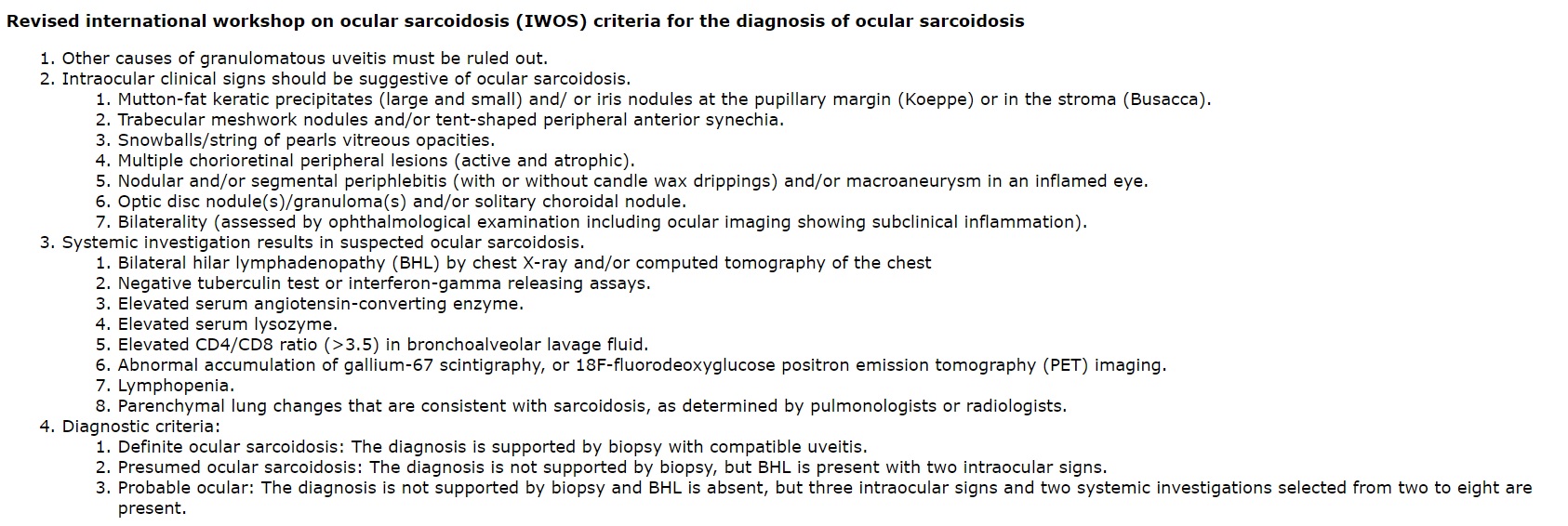
Mochizuki M, Smith JR, Takase H, Kaburaki T, Acharya NR, Rao NA, International Workshop on Ocular Sarcoidosis Study Group. Revised criteria of International Workshop on Ocular Sarcoidosis (IWOS) for the diagnosis of ocular sarcoidosis. The British journal of ophthalmology. 2019 Oct:103(10):1418-1422. doi: 10.1136/bjophthalmol-2018-313356. Epub 2019 Feb 23
[PubMed PMID: 30798264]
[23]
Polverino F, Balestro E, Spagnolo P. Clinical Presentations, Pathogenesis, and Therapy of Sarcoidosis: State of the Art. Journal of clinical medicine. 2020 Jul 24:9(8):. doi: 10.3390/jcm9082363. Epub 2020 Jul 24
[PubMed PMID: 32722050]
[24]
Gupta N, Rajwanshi A, Gupta D. Schaumann body in a case of sarcoidosis diagnosed on transbronchial FNAC. Journal of cytology. 2011 Apr:28(2):88-9. doi: 10.4103/0970-9371.80753. Epub
[PubMed PMID: 21713156]
Level 3 (low-level) evidence
[25]
Mañá J, Marcoval J. Skin manifestations of sarcoidosis. Presse medicale (Paris, France : 1983). 2012 Jun:41(6 Pt 2):e355-74. doi: 10.1016/j.lpm.2012.02.046. Epub 2012 May 9
[PubMed PMID: 22579238]
[26]
Lynch JP 3rd, Hwang J, Bradfield J, Fishbein M, Shivkumar K, Tung R. Cardiac involvement in sarcoidosis: evolving concepts in diagnosis and treatment. Seminars in respiratory and critical care medicine. 2014 Jun:35(3):372-90. doi: 10.1055/s-0034-1376889. Epub 2014 Jul 9
[PubMed PMID: 25007089]
[27]
Chapelon C, Ziza JM, Piette JC, Levy Y, Raguin G, Wechsler B, Bitker MO, Blétry O, Laplane D, Bousser MG. Neurosarcoidosis: signs, course and treatment in 35 confirmed cases. Medicine. 1990 Sep:69(5):261-76
[PubMed PMID: 2205782]
Level 3 (low-level) evidence
[28]
Ungprasert P, Tooley AA, Crowson CS, Matteson EL, Smith WM. Clinical Characteristics of Ocular Sarcoidosis: A Population-Based Study 1976-2013. Ocular immunology and inflammation. 2019:27(3):389-395. doi: 10.1080/09273948.2017.1386791. Epub 2017 Oct 12
[PubMed PMID: 29023165]
[30]
Mavrikakis I, Rootman J. Diverse clinical presentations of orbital sarcoid. American journal of ophthalmology. 2007 Nov:144(5):769-775
[PubMed PMID: 17869205]
[31]
Prabhakaran VC, Saeed P, Esmaeli B, Sullivan TJ, McNab A, Davis G, Valenzuela A, Leibovitch I, Kesler A, Sivak-Callcott J, Hoyama E, Selva D. Orbital and adnexal sarcoidosis. Archives of ophthalmology (Chicago, Ill. : 1960). 2007 Dec:125(12):1657-62
[PubMed PMID: 18071118]
[32]
Kim DS, Korgavkar K, Zahid S, De Lott L, Prabhakar A, Foerster BR, Besirli CG. Vision Loss After Central Retinal Artery Occlusion Secondary to Orbital Sarcoid Mass. Ophthalmic plastic and reconstructive surgery. 2016 Mar-Apr:32(2):e37-40. doi: 10.1097/IOP.0000000000000223. Epub
[PubMed PMID: 25072221]
[33]
JONES BR, STEVENSON CJ. Keratoconjunctivitis sicca due to sarcoidosis. The British journal of ophthalmology. 1957 Mar:41(3):153-60
[PubMed PMID: 13404198]
[34]
Kay DJ, Saffra N, Har-El G. Isolated sarcoidosis of the lacrimal sac without systemic manifestations. American journal of otolaryngology. 2002 Jan-Feb:23(1):53-5
[PubMed PMID: 11791250]
[35]
Hall JG, Cohen KL. Sarcoidosis of the eyelid skin. American journal of ophthalmology. 1995 Jan:119(1):100-1
[PubMed PMID: 7825675]
[36]
Moin M, Kersten RC, Bernardini F, Kulwin DR. Destructive eyelid lesions in sarcoidosis. Ophthalmic plastic and reconstructive surgery. 2001 Mar:17(2):123-5
[PubMed PMID: 11281585]
[37]
Behbehani R, Nipper KS, Eagle RC Jr, Bilyk JR. Systemic sarcoidosis manifested as unilateral eyelid retraction. Archives of ophthalmology (Chicago, Ill. : 1960). 2006 Apr:124(4):599-600
[PubMed PMID: 16606895]
[38]
Dithmar S, Waring GO 3rd, Goldblum TA, Grossniklaus HE. Conjunctival deposits as an initial manifestation of sarcoidosis. American journal of ophthalmology. 1999 Sep:128(3):361-2
[PubMed PMID: 10511034]
[39]
Manrique Lipa RK, de los Bueis AB, De los Ríos JJ, Manrique Lipa RD. Sarcoidosis presenting as acute bulbar follicular conjunctivitis. Clinical & experimental optometry. 2010 Sep:93(5):363-5. doi: 10.1111/j.1444-0938.2010.00508.x. Epub 2010 Aug 16
[PubMed PMID: 20718787]
[40]
Geggel HS, Mensher JH. Cicatricial conjunctivitis in sarcoidosis: recognition and treatment. Annals of ophthalmology. 1989 Mar:21(3):92-4
[PubMed PMID: 2735697]
[41]
Heiligenhaus A, Michel D, Koch JM. Nodular scleritis in a patient with sarcoidosis. The British journal of ophthalmology. 2003 Apr:87(4):507-8
[PubMed PMID: 12642326]
[42]
Dodds EM, Lowder CY, Barnhorst DA, Lavertu P, Caravella LP, White DE. Posterior scleritis with annular ciliochoroidal detachment. American journal of ophthalmology. 1995 Nov:120(5):677-9
[PubMed PMID: 7485375]
[43]
Crick RP, Hoyle C, Smellie H. THE EYES IN SARCOIDOSIS. The British journal of ophthalmology. 1961 Jul:45(7):461-81
[PubMed PMID: 18170695]
[44]
Siracuse-Lee D, Saffra N. Peripheral ulcerative keratitis in sarcoidosis: a case report. Cornea. 2006 Jun:25(5):618-20
[PubMed PMID: 16783154]
Level 3 (low-level) evidence
[45]
Lennarson P, Barney NP. Interstitial keratitis as presenting ophthalmic sign of sarcoidosis in a child. Journal of pediatric ophthalmology and strabismus. 1995 May-Jun:32(3):194-6
[PubMed PMID: 7636703]
[46]
Dana MR, Merayo-Lloves J, Schaumberg DA, Foster CS. Prognosticators for visual outcome in sarcoid uveitis. Ophthalmology. 1996 Nov:103(11):1846-53
[PubMed PMID: 8942880]
[47]
Zaidi AA, Ying GS, Daniel E, Gangaputra S, Rosenbaum JT, Suhler EB, Thorne JE, Foster CS, Jabs DA, Levy-Clarke GA, Nussenblatt RB, Kempen JH, Systemic Immunosuppressive Therapy for Eye Diseases Cohort Study. Hypopyon in patients with uveitis. Ophthalmology. 2010 Feb:117(2):366-72. doi: 10.1016/j.ophtha.2009.07.025. Epub 2009 Dec 14
[PubMed PMID: 20006905]
[48]
Shimizu A, Maruyama K, Yokoyama Y, Tsuda S, Ryu M, Nakazawa T. Characteristics of uveitic glaucoma and evaluation of its surgical treatment. Clinical ophthalmology (Auckland, N.Z.). 2014:8():2383-9. doi: 10.2147/OPTH.S72383. Epub 2014 Nov 26
[PubMed PMID: 25473265]
[50]
Spalton DJ, Sanders MD. Fundus changes in histologically confirmed sarcoidosis. The British journal of ophthalmology. 1981 May:65(5):348-58
[PubMed PMID: 6166318]
[51]
Letocha CE, Shields JA, Goldberg RE. Retinal changes in sarcoidosis. Canadian journal of ophthalmology. Journal canadien d'ophtalmologie. 1975 Apr:10(2):184-92
[PubMed PMID: 1125843]
[52]
Kumawat BL, Chawla R, Venkatesh P, Tripathy K. Inflammatory optic disc neovascularisation managed with oral steroids/immunosuppressants and intravitreal ranibizumab. BMJ case reports. 2017 Nov 3:2017():. pii: bcr-2017-222262. doi: 10.1136/bcr-2017-222262. Epub 2017 Nov 3
[PubMed PMID: 29102974]
Level 3 (low-level) evidence
[53]
GOULD H, KAUFMAN HE. Sarcoid of the fundus. Archives of ophthalmology (Chicago, Ill. : 1960). 1961 Mar:65():453-6
[PubMed PMID: 13707501]
[54]
Phillips YL, Eggenberger ER. Neuro-ophthalmic sarcoidosis. Current opinion in ophthalmology. 2010 Nov:21(6):423-9. doi: 10.1097/ICU.0b013e32833eae4d. Epub
[PubMed PMID: 20736834]
Level 3 (low-level) evidence
[55]
Gass JD, Olson CL. Sarcoidosis with optic nerve and retinal involvement. Archives of ophthalmology (Chicago, Ill. : 1960). 1976 Jun:94(6):945-50
[PubMed PMID: 938285]
[57]
Poole CJ. Argyll Robertson pupils due to neurosarcoidosis: evidence for site of lesion. British medical journal (Clinical research ed.). 1984 Aug 11:289(6441):356
[PubMed PMID: 6432097]
[59]
Zajicek JP, Scolding NJ, Foster O, Rovaris M, Evanson J, Moseley IF, Scadding JW, Thompson EJ, Chamoun V, Miller DH, McDonald WI, Mitchell D. Central nervous system sarcoidosis--diagnosis and management. QJM : monthly journal of the Association of Physicians. 1999 Feb:92(2):103-17
[PubMed PMID: 10209662]
[60]
Chauhan A,Jandial A,Mishra K,Sandal R, Acute arthritis, skin rash and Lofgren's syndrome. BMJ case reports. 2021 Jun 7;
[PubMed PMID: 34099443]
Level 3 (low-level) evidence
[61]
Denny MC, Fotino AD. The Heerfordt-Waldenström syndrome as an initial presentation of sarcoidosis. Proceedings (Baylor University. Medical Center). 2013 Oct:26(4):390-2
[PubMed PMID: 24082416]
[62]
Sfriso P, Caso F, Tognon S, Galozzi P, Gava A, Punzi L. Blau syndrome, clinical and genetic aspects. Autoimmunity reviews. 2012 Nov:12(1):44-51. doi: 10.1016/j.autrev.2012.07.028. Epub 2012 Aug 2
[PubMed PMID: 22884558]
[63]
Herbort CP, Rao NA, Mochizuki M, members of Scientific Committee of First International Workshop on Ocular Sarcoidosis. International criteria for the diagnosis of ocular sarcoidosis: results of the first International Workshop On Ocular Sarcoidosis (IWOS). Ocular immunology and inflammation. 2009 May-Jun:17(3):160-9. doi: 10.1080/09273940902818861. Epub
[PubMed PMID: 19585358]
[64]
Dickson D, Agarwal A, Sadiq MA, Hassan M, High R, Nguyen QD, Sepah YJ. Assessment of vitreous haze using ultra-wide field retinal imaging. Journal of ophthalmic inflammation and infection. 2016 Dec:6(1):35. doi: 10.1186/s12348-016-0105-0. Epub 2016 Sep 29
[PubMed PMID: 27687961]
[65]
Nicholson BP, Nigam D, Miller D, Agrón E, Dalal M, Jacobs-El N, da Rocha Lima B, Cunningham D, Nussenblatt R, Sen HN. Comparison of wide-field fluorescein angiography and 9-field montage angiography in uveitis. American journal of ophthalmology. 2014 Mar:157(3):673-7. doi: 10.1016/j.ajo.2013.12.005. Epub 2013 Dec 7
[PubMed PMID: 24321475]
[68]
Reznicek L, Seidensticker F, Stumpf C, Kampik A, Thurau S, Kernt M, Neubauer A. Systematic analysis of wide-field fundus autofluorescence (FAF) imaging in posterior uveitis. Current eye research. 2014 Feb:39(2):164-71. doi: 10.3109/02713683.2013.834938. Epub 2013 Oct 21
[PubMed PMID: 24144279]
Level 1 (high-level) evidence
[69]
Pakzad-Vaezi K, Or C, Yeh S, Forooghian F. Optical coherence tomography in the diagnosis and management of uveitis. Canadian journal of ophthalmology. Journal canadien d'ophtalmologie. 2014 Feb:49(1):18-29. doi: 10.1016/j.jcjo.2013.10.005. Epub 2013 Dec 22
[PubMed PMID: 24513352]
[70]
Invernizzi A, Mapelli C, Viola F, Cigada M, Cimino L, Ratiglia R, Staurenghi G, Gupta A. Choroidal granulomas visualized by enhanced depth imaging optical coherence tomography. Retina (Philadelphia, Pa.). 2015 Mar:35(3):525-31. doi: 10.1097/IAE.0000000000000312. Epub
[PubMed PMID: 25105317]
[71]
Su DH, Friedman DS, See JL, Chew PT, Chan YH, Nolan WP, Smith SD, Huang D, Zheng C, Li Y, Foster PJ, Aung T. Degree of angle closure and extent of peripheral anterior synechiae: an anterior segment OCT study. The British journal of ophthalmology. 2008 Jan:92(1):103-7
[PubMed PMID: 17584995]
[72]
Concilio M, Cennamo G, Giordano M, Fossataro F, D'Andrea L, Ciampa N, Naddei R, Orlando F, Tranfa F, Alessio M. Anterior Segment-Optical Coherence Tomography features in Blau syndrome. Photodiagnosis and photodynamic therapy. 2021 Jun:34():102278. doi: 10.1016/j.pdpdt.2021.102278. Epub 2021 Apr 1
[PubMed PMID: 33813016]
[73]
Hickman SJ,Quhill F,Pepper IM, The Evolution of an Optic Nerve Head Granuloma Due to Sarcoidosis. Neuro-ophthalmology (Aeolus Press). 2016 Apr;
[PubMed PMID: 27928387]
[74]
Sathyan P, Shilpa S, Anitha A. Optical Coherence Tomography in Glaucoma. Journal of current glaucoma practice. 2012 Jan-Apr:6(1):1-5
[PubMed PMID: 27990063]
[75]
Tran VT, LeHoang P, Herbort CP. Value of high-frequency ultrasound biomicroscopy in uveitis. Eye (London, England). 2001 Feb:15(Pt 1):23-30
[PubMed PMID: 11318288]
[76]
Roters S, Szurman P, Engels BF, Bartz-Schmidt KU, Krieglstein GK. Ultrasound biomicroscopy in chronic ocular hypotony: its impact on diagnosis and management. Retina (Philadelphia, Pa.). 2002 Oct:22(5):581-8
[PubMed PMID: 12441723]
[77]
Kidd DP, Burton BJ, Graham EM, Plant GT. Optic neuropathy associated with systemic sarcoidosis. Neurology(R) neuroimmunology & neuroinflammation. 2016 Oct:3(5):e270. doi: 10.1212/NXI.0000000000000270. Epub 2016 Aug 2
[PubMed PMID: 27536707]
[78]
Takeuchi M,Taguchi M,Sato T,Karasawa K,Sakurai Y,Harimoto K,Ito M, Association of High-Mobility Group Box-1 With Th Cell-Related Cytokines in the Vitreous of Ocular Sarcoidosis Patients. Investigative ophthalmology
[PubMed PMID: 28125840]
[79]
Lynch JP 3rd, Kazerooni EA, Gay SE. Pulmonary sarcoidosis. Clinics in chest medicine. 1997 Dec:18(4):755-85
[PubMed PMID: 9413657]
[80]
Hillerdal G,Nöu E,Osterman K,Schmekel B, Sarcoidosis: epidemiology and prognosis. A 15-year European study. The American review of respiratory disease. 1984 Jul;
[PubMed PMID: 6742607]
[81]
Lynch JP 3rd, Ma YL, Koss MN, White ES. Pulmonary sarcoidosis. Seminars in respiratory and critical care medicine. 2007 Feb:28(1):53-74
[PubMed PMID: 17330192]
[82]
Lynch JP 3rd, Computed tomographic scanning in sarcoidosis. Seminars in respiratory and critical care medicine. 2003 Aug;
[PubMed PMID: 16088560]
[83]
Hennebicque AS,Nunes H,Brillet PY,Moulahi H,Valeyre D,Brauner MW, CT findings in severe thoracic sarcoidosis. European radiology. 2005 Jan;
[PubMed PMID: 15449010]
[84]
Soto-Gomez N, Peters JI, Nambiar AM. Diagnosis and Management of Sarcoidosis. American family physician. 2016 May 15:93(10):840-8
[PubMed PMID: 27175719]
[85]
Lieberman J, Schleissner LA, Nosal A, Sastre A, Mishkin FS. Clinical correlations of serum angiotensin-converting enzyme (ACE) in sarcoidosis. A longitudinal study of serum ACE, 67gallium scans, chest roentgenograms, and pulmonary function. Chest. 1983 Nov:84(5):522-8
[PubMed PMID: 6313303]
[86]
Welker L, Jörres RA, Costabel U, Magnussen H. Predictive value of BAL cell differentials in the diagnosis of interstitial lung diseases. The European respiratory journal. 2004 Dec:24(6):1000-6
[PubMed PMID: 15572545]
[87]
Drent M, Mulder PG, Wagenaar SS, Hoogsteden HC, van Velzen-Blad H, van den Bosch JM. Differences in BAL fluid variables in interstitial lung diseases evaluated by discriminant analysis. The European respiratory journal. 1993 Jun:6(6):803-10
[PubMed PMID: 8339798]
[88]
Ismail S, Embong Z, Hitam WH. Gallium scan in diagnosing ocular sarcoidosis. The Malaysian journal of medical sciences : MJMS. 2005 Jan:12(1):64-7
[PubMed PMID: 22605949]
[89]
Yoshimizu T, Suga K, Orihashi N, Soejima K, Kaneko T, Kawamura M, Nakanishi T, Utsumi H, Yamada N. [The appearance of "lambda" and "panda" sign on Ga-67 scintigraphy in sarcoidosis]. Kaku igaku. The Japanese journal of nuclear medicine. 1991 Oct:28(10):1151-7
[PubMed PMID: 1800775]
[90]
Brudin LH, Valind SO, Rhodes CG, Pantin CF, Sweatman M, Jones T, Hughes JM. Fluorine-18 deoxyglucose uptake in sarcoidosis measured with positron emission tomography. European journal of nuclear medicine. 1994 Apr:21(4):297-305
[PubMed PMID: 8005153]
[91]
Aberg C, Ponzo F, Raphael B, Amorosi E, Moran V, Kramer E. FDG positron emission tomography of bone involvement in sarcoidosis. AJR. American journal of roentgenology. 2004 Apr:182(4):975-7
[PubMed PMID: 15039174]
[92]
Takeda N, Yokoyama I, Hiroi Y, Sakata M, Harada T, Nakamura F, Murakawa Y, Nagai R. Positron emission tomography predicted recovery of complete A-V nodal dysfunction in a patient with cardiac sarcoidosis. Circulation. 2002 Mar 5:105(9):1144-5
[PubMed PMID: 11877369]
[93]
Dubey N, Miletich RS, Wasay M, Mechtler LL, Bakshi R. Role of fluorodeoxyglucose positron emission tomography in the diagnosis of neurosarcoidosis. Journal of the neurological sciences. 2002 Dec 15:205(1):77-81
[PubMed PMID: 12409188]
[94]
Gilman MJ, Wang KP. Transbronchial lung biopsy in sarcoidosis. An approach to determine the optimal number of biopsies. The American review of respiratory disease. 1980 Nov:122(5):721-4
[PubMed PMID: 7447156]
[95]
Trisolini R, Lazzari Agli L, Cancellieri A, Poletti V, Candoli P, Paioli D, Alifano M, Tinelli C, Patelli M. Transbronchial needle aspiration improves the diagnostic yield of bronchoscopy in sarcoidosis. Sarcoidosis, vasculitis, and diffuse lung diseases : official journal of WASOG. 2004 Jun:21(2):147-51
[PubMed PMID: 15281436]
[96]
Trisolini R, Lazzari Agli L, Cancellieri A, Poletti V, Tinelli C, Baruzzi G, Patelli M. The value of flexible transbronchial needle aspiration in the diagnosis of stage I sarcoidosis. Chest. 2003 Dec:124(6):2126-30
[PubMed PMID: 14665490]
[98]
Mikhail JR, Mitchell DN. The Kveim test in sarcoidosis. Postgraduate medical journal. 1970 Aug:46(538):484-5
[PubMed PMID: 5481096]
[99]
Newman LS, Rose CS, Maier LA. Sarcoidosis. The New England journal of medicine. 1997 Apr 24:336(17):1224-34
[PubMed PMID: 9110911]
[100]
Fels C, Riegel A, Javaheripour-Otto K, Obenauer S. Neurosarcoidosis: findings in MRI. Clinical imaging. 2004 May-Jun:28(3):166-9
[PubMed PMID: 15158219]
[101]
Sheppard JD, Toyos MM, Kempen JH, Kaur P, Foster CS. Difluprednate 0.05% versus prednisolone acetate 1% for endogenous anterior uveitis: a phase III, multicenter, randomized study. Investigative ophthalmology & visual science. 2014 May 6:55(5):2993-3002. doi: 10.1167/iovs.13-12660. Epub 2014 May 6
[PubMed PMID: 24677110]
Level 1 (high-level) evidence
[102]
Kok H, Lau C, Maycock N, McCluskey P, Lightman S. Outcome of intravitreal triamcinolone in uveitis. Ophthalmology. 2005 Nov:112(11):1916.e1-7
[PubMed PMID: 16171868]
[103]
Khurana RN, Porco TC. EFFICACY AND SAFETY OF DEXAMETHASONE INTRAVITREAL IMPLANT FOR PERSISTENT UVEITIC CYSTOID MACULAR EDEMA. Retina (Philadelphia, Pa.). 2015 Aug:35(8):1640-6. doi: 10.1097/IAE.0000000000000515. Epub
[PubMed PMID: 25741813]
[104]
Jaffe GJ, Martin D, Callanan D, Pearson PA, Levy B, Comstock T, Fluocinolone Acetonide Uveitis Study Group. Fluocinolone acetonide implant (Retisert) for noninfectious posterior uveitis: thirty-four-week results of a multicenter randomized clinical study. Ophthalmology. 2006 Jun:113(6):1020-7
[PubMed PMID: 16690128]
Level 1 (high-level) evidence
[105]
Pavesio C, Zierhut M, Bairi K, Comstock TL, Usner DW, Fluocinolone Acetonide Study Group. Evaluation of an intravitreal fluocinolone acetonide implant versus standard systemic therapy in noninfectious posterior uveitis. Ophthalmology. 2010 Mar:117(3):567-75, 575.e1. doi: 10.1016/j.ophtha.2009.11.027. Epub 2010 Jan 15
[PubMed PMID: 20079922]
[106]
Gangaputra S, Newcomb CW, Liesegang TL, Kaçmaz RO, Jabs DA, Levy-Clarke GA, Nussenblatt RB, Rosenbaum JT, Suhler EB, Thorne JE, Foster CS, Kempen JH, Systemic Immunosuppressive Therapy for Eye Diseases Cohort Study. Methotrexate for ocular inflammatory diseases. Ophthalmology. 2009 Nov:116(11):2188-98.e1. doi: 10.1016/j.ophtha.2009.04.020. Epub 2009 Sep 12
[PubMed PMID: 19748676]
[107]
Kaçmaz RO, Kempen JH, Newcomb C, Daniel E, Gangaputra S, Nussenblatt RB, Rosenbaum JT, Suhler EB, Thorne JE, Jabs DA, Levy-Clarke GA, Foster CS. Cyclosporine for ocular inflammatory diseases. Ophthalmology. 2010 Mar:117(3):576-84. doi: 10.1016/j.ophtha.2009.08.010. Epub 2010 Jan 19
[PubMed PMID: 20031223]
[108]
Pasadhika S, Kempen JH, Newcomb CW, Liesegang TL, Pujari SS, Rosenbaum JT, Thorne JE, Foster CS, Jabs DA, Levy-Clarke GA, Nussenblatt RB, Suhler EB. Azathioprine for ocular inflammatory diseases. American journal of ophthalmology. 2009 Oct:148(4):500-509.e2. doi: 10.1016/j.ajo.2009.05.008. Epub 2009 Jul 1
[PubMed PMID: 19570522]
[109]
Kane SV. Preparing for biologic or immunosuppressant therapy. Gastroenterology & hepatology. 2011 Aug:7(8):544-6
[PubMed PMID: 22298992]
[110]
Daïen CI, Monnier A, Claudepierre P, Constantin A, Eschard JP, Houvenagel E, Samimi M, Pavy S, Pertuiset E, Toussirot E, Combe B, Morel J, Club Rhumatismes et Inflammation (CRI). Sarcoid-like granulomatosis in patients treated with tumor necrosis factor blockers: 10 cases. Rheumatology (Oxford, England). 2009 Aug:48(8):883-6. doi: 10.1093/rheumatology/kep046. Epub 2009 May 7
[PubMed PMID: 19423648]
Level 3 (low-level) evidence
[111]
Akpek EK, Ilhan-Sarac O, Green WR. Topical cyclosporin in the treatment of chronic sarcoidosis of the conjunctiva. Archives of ophthalmology (Chicago, Ill. : 1960). 2003 Sep:121(9):1333-5
[PubMed PMID: 12963621]
[112]
Cordero Coma M, Sobrin L, Onal S, Christen W, Foster CS. Intravitreal bevacizumab for treatment of uveitic macular edema. Ophthalmology. 2007 Aug:114(8):1574-1579.e1
[PubMed PMID: 17363060]
[113]
Acharya NR, Hong KC, Lee SM. Ranibizumab for refractory uveitis-related macular edema. American journal of ophthalmology. 2009 Aug:148(2):303-309.e2. doi: 10.1016/j.ajo.2009.03.028. Epub 2009 May 9
[PubMed PMID: 19427988]
[117]
Levy A, Hamzeh N, Maier LA. Is it time to scrap Scadding and adopt computed tomography for initial evaluation of sarcoidosis? F1000Research. 2018:7():. pii: F1000 Faculty Rev-600. doi: 10.12688/f1000research.11068.1. Epub 2018 May 16
[PubMed PMID: 29946423]
[118]
Miller BH, Rosado-de-Christenson ML, McAdams HP, Fishback NF. Thoracic sarcoidosis: radiologic-pathologic correlation. Radiographics : a review publication of the Radiological Society of North America, Inc. 1995 Mar:15(2):421-37
[PubMed PMID: 7761646]
[119]
Karma A, Huhti E, Poukkula A. Course and outcome of ocular sarcoidosis. American journal of ophthalmology. 1988 Oct 15:106(4):467-72
[PubMed PMID: 3177566]
[120]
Sato H, Grutters JC, Pantelidis P, Mizzon AN, Ahmad T, Van Houte AJ, Lammers JW, Van Den Bosch JM, Welsh KI, Du Bois RM. HLA-DQB1*0201: a marker for good prognosis in British and Dutch patients with sarcoidosis. American journal of respiratory cell and molecular biology. 2002 Oct:27(4):406-12
[PubMed PMID: 12356573]
[121]
Kobak S. Catch the rainbow: Prognostic factor of sarcoidosis. Lung India : official organ of Indian Chest Society. 2020 Sep-Oct:37(5):425-432. doi: 10.4103/lungindia.lungindia_380_19. Epub
[PubMed PMID: 32883904]
[122]
Tripathy K, Chawla R, Temkar S, Sagar P, Kashyap S, Pushker N, Sharma YR. Phthisis Bulbi-a Clinicopathological Perspective. Seminars in ophthalmology. 2018:33(6):788-803. doi: 10.1080/08820538.2018.1477966. Epub 2018 Jun 14
[PubMed PMID: 29902388]
Level 3 (low-level) evidence
[123]
Matsou A, Tsaousis KT. Management of chronic ocular sarcoidosis: challenges and solutions. Clinical ophthalmology (Auckland, N.Z.). 2018:12():519-532. doi: 10.2147/OPTH.S128949. Epub 2018 Mar 19
[PubMed PMID: 29593377]
[124]
Edelsten C, Pearson A, Joynes E, Stanford MR, Graham EM. The ocular and systemic prognosis of patients presenting with sarcoid uveitis. Eye (London, England). 1999 Dec:13 ( Pt 6)():748-53
[PubMed PMID: 10707138]