[1]
Tranos PG, Wickremasinghe SS, Stangos NT, Topouzis F, Tsinopoulos I, Pavesio CE. Macular edema. Survey of ophthalmology. 2004 Sep-Oct:49(5):470-90
[PubMed PMID: 15325193]
Level 3 (low-level) evidence
[2]
Rotsos TG, Moschos MM. Cystoid macular edema. Clinical ophthalmology (Auckland, N.Z.). 2008 Dec:2(4):919-30
[PubMed PMID: 19668445]
[3]
Scholl S, Kirchhof J, Augustin AJ. Pathophysiology of macular edema. Ophthalmologica. Journal international d'ophtalmologie. International journal of ophthalmology. Zeitschrift fur Augenheilkunde. 2010:224 Suppl 1():8-15. doi: 10.1159/000315155. Epub 2010 Aug 18
[PubMed PMID: 20714176]
[4]
Cunha-Vaz J. Mechanisms of Retinal Fluid Accumulation and Blood-Retinal Barrier Breakdown. Developments in ophthalmology. 2017:58():11-20. doi: 10.1159/000455265. Epub 2017 Mar 28
[PubMed PMID: 28351041]
[5]
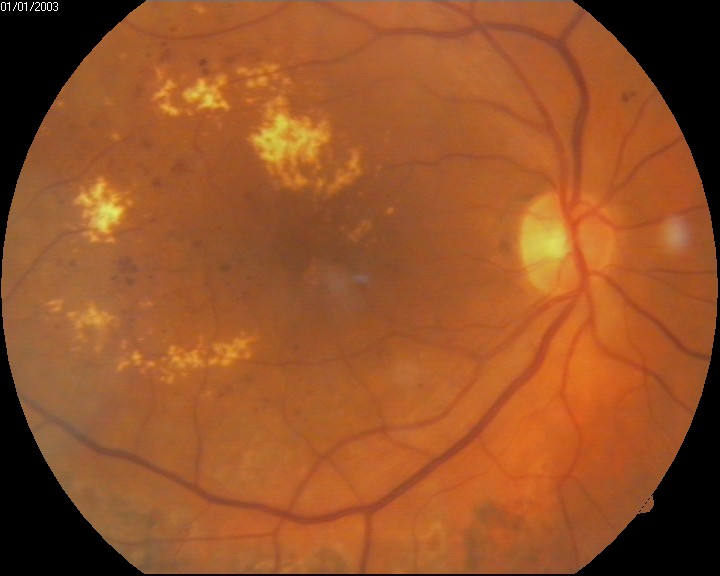
Sen M, Shields CL, Honavar SG, Shields JA. Coats disease: An overview of classification, management and outcomes. Indian journal of ophthalmology. 2019 Jun:67(6):763-771. doi: 10.4103/ijo.IJO_841_19. Epub
[PubMed PMID: 31124484]
Level 3 (low-level) evidence
[6]
Pitkänen L, Tommila P, Kaarniranta K, Jääskeläinen JE, Kinnunen K. Retinal arterial macroaneurysms. Acta ophthalmologica. 2014 Mar:92(2):101-4. doi: 10.1111/aos.12210. Epub 2013 Jun 25
[PubMed PMID: 23800325]
[7]
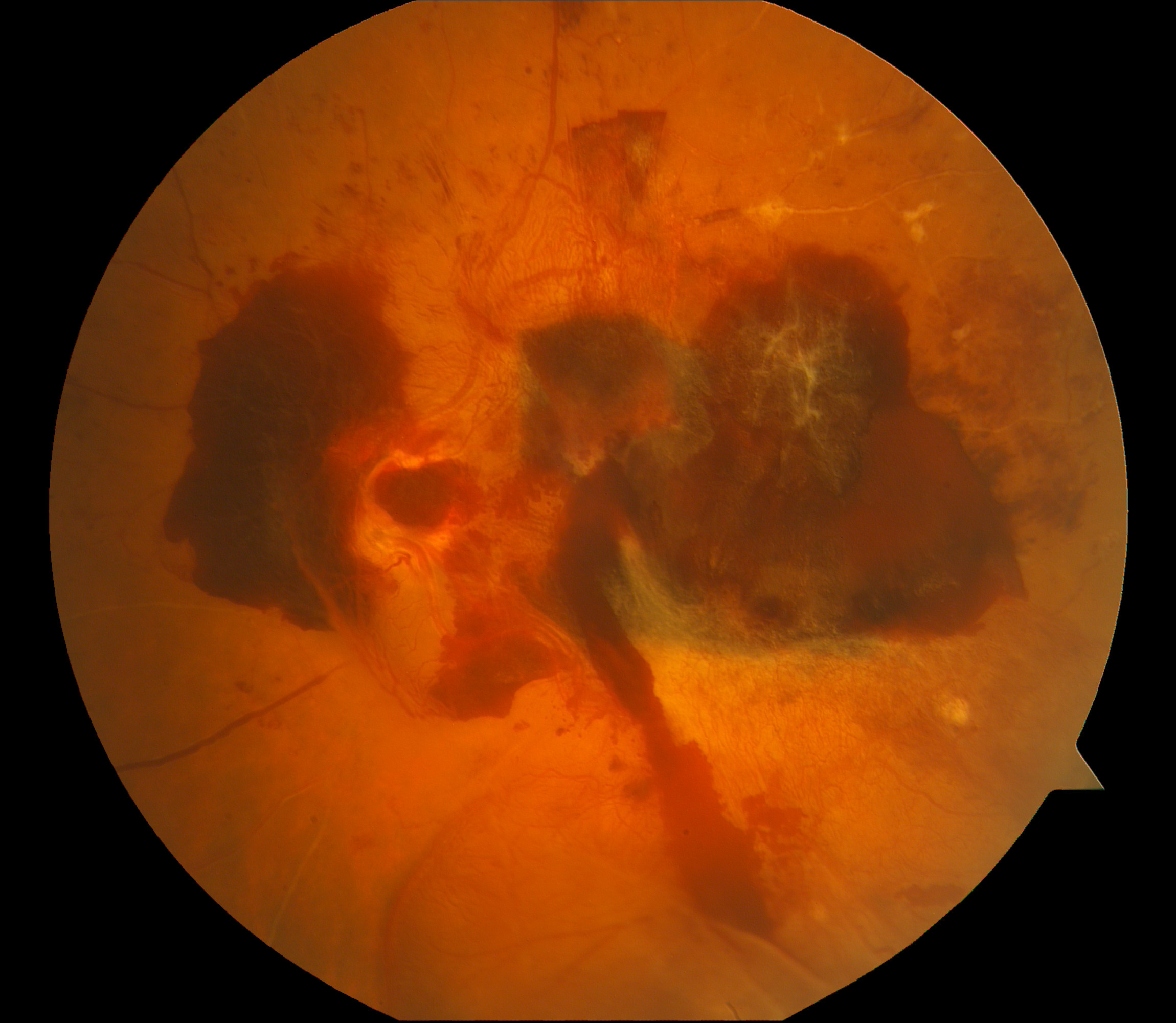
Brown GC, Shields JA, Sanborn G, Augsburger JJ, Savino PJ, Schatz NJ. Radiation retinopathy. Ophthalmology. 1982 Dec:89(12):1494-501
[PubMed PMID: 7162794]
[8]
Horgan N, Shields CL, Mashayekhi A, Shields JA. Classification and treatment of radiation maculopathy. Current opinion in ophthalmology. 2010 May:21(3):233-8. doi: 10.1097/ICU.0b013e3283386687. Epub
[PubMed PMID: 20393294]
Level 3 (low-level) evidence
[9]
Grzybowski A, Sikorski BL, Ascaso FJ, Huerva V. Pseudophakic cystoid macular edema: update 2016. Clinical interventions in aging. 2016:11():1221-1229
[PubMed PMID: 27672316]
[10]
Koronis S, Stavrakas P, Balidis M, Kozeis N, Tranos PG. Update in treatment of uveitic macular edema. Drug design, development and therapy. 2019:13():667-680. doi: 10.2147/DDDT.S166092. Epub 2019 Feb 19
[PubMed PMID: 30858697]
[11]
Hedges TR 3rd, Vuong LN, Gonzalez-Garcia AO, Mendoza-Santiesteban CE, Amaro-Quierza ML. Subretinal fluid from anterior ischemic optic neuropathy demonstrated by optical coherence tomography. Archives of ophthalmology (Chicago, Ill. : 1960). 2008 Jun:126(6):812-5. doi: 10.1001/archopht.126.6.812. Epub
[PubMed PMID: 18541844]
[12]
Drenser K, Sarraf D, Jain A, Small KW. Crystalline retinopathies. Survey of ophthalmology. 2006 Nov-Dec:51(6):535-49
[PubMed PMID: 17134644]
Level 3 (low-level) evidence
[14]
Domanico D, Verboschi F, Altimari S, Zompatori L, Vingolo EM. Ocular Effects of Niacin: A Review of the Literature. Medical hypothesis, discovery & innovation ophthalmology journal. 2015 Summer:4(2):64-71
[PubMed PMID: 26060832]
[15]
Strong S, Liew G, Michaelides M. Retinitis pigmentosa-associated cystoid macular oedema: pathogenesis and avenues of intervention. The British journal of ophthalmology. 2017 Jan:101(1):31-37. doi: 10.1136/bjophthalmol-2016-309376. Epub 2016 Dec 2
[PubMed PMID: 27913439]
[16]
Lee R, Wong TY, Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye and vision (London, England). 2015:2():17. doi: 10.1186/s40662-015-0026-2. Epub 2015 Sep 30
[PubMed PMID: 26605370]
[17]
Toklu Y, Sarac O, Berk S, Simsek S. Angioedema after intravitreal bevacizumab injection. Cutaneous and ocular toxicology. 2012 Mar:31(1):85-6. doi: 10.3109/15569527.2011.609207. Epub
[PubMed PMID: 22309281]
[18]
. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study research group. Archives of ophthalmology (Chicago, Ill. : 1960). 1985 Dec:103(12):1796-806
[PubMed PMID: 2866759]
[19]
Laursen ML, Moeller F, Sander B, Sjoelie AK. Subthreshold micropulse diode laser treatment in diabetic macular oedema. The British journal of ophthalmology. 2004 Sep:88(9):1173-9
[PubMed PMID: 15317711]
[20]
Sander B, Larsen M, Engler C, Strøm C, Moldow B, Larsen N, Lund-Andersen H. Diabetic macular oedema: a comparison of vitreous fluorometry, angiography, and retinopathy. The British journal of ophthalmology. 2002 Mar:86(3):316-20
[PubMed PMID: 11864891]
[21]
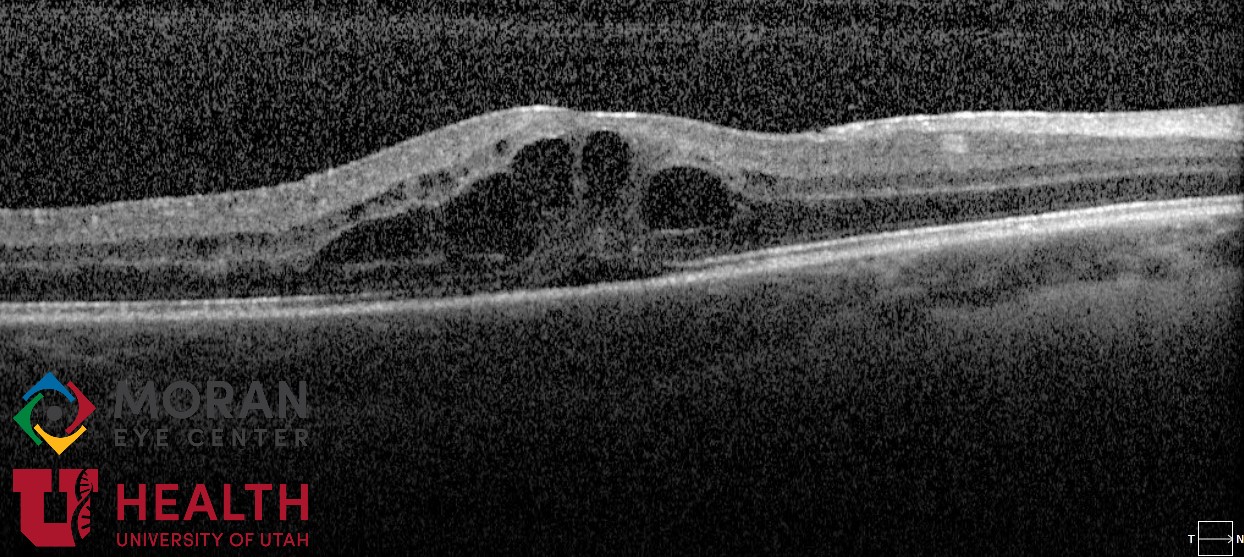
Kim BY, Smith SD, Kaiser PK. Optical coherence tomographic patterns of diabetic macular edema. American journal of ophthalmology. 2006 Sep:142(3):405-12
[PubMed PMID: 16935584]
[22]
Prenner JL, Capone A Jr, Ciaccia S, Takada Y, Sieving PA, Trese MT. Congenital X-linked retinoschisis classification system. Retina (Philadelphia, Pa.). 2006 Sep:26(7 Suppl):S61-4
[PubMed PMID: 16946682]
[23]
Rao P, Dedania VS, Drenser KA. Congenital X-Linked Retinoschisis: An Updated Clinical Review. Asia-Pacific journal of ophthalmology (Philadelphia, Pa.). 2018 May-Jun:7(3):169-175. doi: 10.22608/APO.201803. Epub 2018 Apr 9
[PubMed PMID: 29633586]
[24]
Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Davis M, Rand L, Siebert C. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The New England journal of medicine. 1993 Sep 30:329(14):977-86
[PubMed PMID: 8366922]
[25]
. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet (London, England). 1998 Sep 12:352(9131):837-53
[PubMed PMID: 9742976]
[26]
Klein R, Klein BE, Moss SE, Cruickshanks KJ. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. XV. The long-term incidence of macular edema. Ophthalmology. 1995 Jan:102(1):7-16
[PubMed PMID: 7831044]
[27]
ACCORD Study Group, ACCORD Eye Study Group, Chew EY, Ambrosius WT, Davis MD, Danis RP, Gangaputra S, Greven CM, Hubbard L, Esser BA, Lovato JF, Perdue LH, Goff DC Jr, Cushman WC, Ginsberg HN, Elam MB, Genuth S, Gerstein HC, Schubart U, Fine LJ. Effects of medical therapies on retinopathy progression in type 2 diabetes. The New England journal of medicine. 2010 Jul 15:363(3):233-44. doi: 10.1056/NEJMoa1001288. Epub 2010 Jun 29
[PubMed PMID: 20587587]
[28]
Keech AC, Mitchell P, Summanen PA, O'Day J, Davis TM, Moffitt MS, Taskinen MR, Simes RJ, Tse D, Williamson E, Merrifield A, Laatikainen LT, d'Emden MC, Crimet DC, O'Connell RL, Colman PG, FIELD study investigators. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet (London, England). 2007 Nov 17:370(9600):1687-97
[PubMed PMID: 17988728]
Level 1 (high-level) evidence
[29]
Taubenslag KJ, Kim SJ, Grzybowski A. Anti-inflammatory Pharmacotherapy for the Prevention of Cystoid Macular Edema After Cataract Surgery. American journal of ophthalmology. 2021 Dec:232():1-8. doi: 10.1016/j.ajo.2021.06.009. Epub 2021 Jun 19
[PubMed PMID: 34157275]
[30]
Friedman SM, Almukhtar TH, Baker CW, Glassman AR, Elman MJ, Bressler NM, Maker MP, Jampol LM, Melia M, Diabetic Retinopathy Clinical Research Network. Topical nepafenec in eyes with noncentral diabetic macular edema. Retina (Philadelphia, Pa.). 2015 May:35(5):944-56. doi: 10.1097/IAE.0000000000000403. Epub
[PubMed PMID: 25602634]
[31]
Romero-Aroca P, Reyes-Torres J, Baget-Bernaldiz M, Blasco-Suñe C. Laser treatment for diabetic macular edema in the 21st century. Current diabetes reviews. 2014 Mar:10(2):100-12
[PubMed PMID: 24852439]
[32]
Writing Committee for the Diabetic Retinopathy Clinical Research Network, Fong DS, Strauber SF, Aiello LP, Beck RW, Callanan DG, Danis RP, Davis MD, Feman SS, Ferris F, Friedman SM, Garcia CA, Glassman AR, Han DP, Le D, Kollman C, Lauer AK, Recchia FM, Solomon SD. Comparison of the modified Early Treatment Diabetic Retinopathy Study and mild macular grid laser photocoagulation strategies for diabetic macular edema. Archives of ophthalmology (Chicago, Ill. : 1960). 2007 Apr:125(4):469-80
[PubMed PMID: 17420366]
[33]
. Focal photocoagulation treatment of diabetic macular edema. Relationship of treatment effect to fluorescein angiographic and other retinal characteristics at baseline: ETDRS report no. 19. Early Treatment Diabetic Retinopathy Study Research Group. Archives of ophthalmology (Chicago, Ill. : 1960). 1995 Sep:113(9):1144-55
[PubMed PMID: 7661748]
[34]
Diabetic Retinopathy Clinical Research Network. A randomized trial comparing intravitreal triamcinolone acetonide and focal/grid photocoagulation for diabetic macular edema. Ophthalmology. 2008 Sep:115(9):1447-9, 1449.e1-10. doi: 10.1016/j.ophtha.2008.06.015. Epub 2008 Jul 26
[PubMed PMID: 18662829]
Level 1 (high-level) evidence
[35]
Miller SD. Argon laser photocoagulation for macular edema in branch vein occlusion. American journal of ophthalmology. 1985 Feb 15:99(2):218-9
[PubMed PMID: 4038586]
[36]
. Evaluation of grid pattern photocoagulation for macular edema in central vein occlusion. The Central Vein Occlusion Study Group M report. Ophthalmology. 1995 Oct:102(10):1425-33
[PubMed PMID: 9097788]
[37]
Jain N, Johnson MW. Pathogenesis and treatment of maculopathy associated with cavitary optic disc anomalies. American journal of ophthalmology. 2014 Sep:158(3):423-35. doi: 10.1016/j.ajo.2014.06.001. Epub 2014 Jun 14
[PubMed PMID: 24932988]
[38]
Babu N, Kohli P, Ramasamy K. Comparison of various surgical techniques for optic disc pit maculopathy: vitrectomy with internal limiting membrane (ILM) peeling alone versus inverted ILM flap 'plug' versus autologous scleral 'plug'. The British journal of ophthalmology. 2020 Nov:104(11):1567-1573. doi: 10.1136/bjophthalmol-2019-315075. Epub 2020 Feb 6
[PubMed PMID: 32029434]
[39]
Ng EW, Shima DT, Calias P, Cunningham ET Jr, Guyer DR, Adamis AP. Pegaptanib, a targeted anti-VEGF aptamer for ocular vascular disease. Nature reviews. Drug discovery. 2006 Feb:5(2):123-32
[PubMed PMID: 16518379]
[40]
Diabetic Retinopathy Clinical Research Network, Scott IU, Edwards AR, Beck RW, Bressler NM, Chan CK, Elman MJ, Friedman SM, Greven CM, Maturi RK, Pieramici DJ, Shami M, Singerman LJ, Stockdale CR. A phase II randomized clinical trial of intravitreal bevacizumab for diabetic macular edema. Ophthalmology. 2007 Oct:114(10):1860-7
[PubMed PMID: 17698196]
Level 1 (high-level) evidence
[41]
Michaelides M, Kaines A, Hamilton RD, Fraser-Bell S, Rajendram R, Quhill F, Boos CJ, Xing W, Egan C, Peto T, Bunce C, Leslie RD, Hykin PG. A prospective randomized trial of intravitreal bevacizumab or laser therapy in the management of diabetic macular edema (BOLT study) 12-month data: report 2. Ophthalmology. 2010 Jun:117(6):1078-1086.e2. doi: 10.1016/j.ophtha.2010.03.045. Epub 2010 Apr 22
[PubMed PMID: 20416952]
Level 1 (high-level) evidence
[42]
Massin P, Bandello F, Garweg JG, Hansen LL, Harding SP, Larsen M, Mitchell P, Sharp D, Wolf-Schnurrbusch UE, Gekkieva M, Weichselberger A, Wolf S. Safety and efficacy of ranibizumab in diabetic macular edema (RESOLVE Study): a 12-month, randomized, controlled, double-masked, multicenter phase II study. Diabetes care. 2010 Nov:33(11):2399-405. doi: 10.2337/dc10-0493. Epub
[PubMed PMID: 20980427]
Level 1 (high-level) evidence
[43]
Mitchell P, Bandello F, Schmidt-Erfurth U, Lang GE, Massin P, Schlingemann RO, Sutter F, Simader C, Burian G, Gerstner O, Weichselberger A, RESTORE study group. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011 Apr:118(4):615-25. doi: 10.1016/j.ophtha.2011.01.031. Epub
[PubMed PMID: 21459215]
[44]
Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L, Gibson A, Sy J, Rundle AC, Hopkins JJ, Rubio RG, Ehrlich JS, RISE and RIDE Research Group. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012 Apr:119(4):789-801. doi: 10.1016/j.ophtha.2011.12.039. Epub 2012 Feb 11
[PubMed PMID: 22330964]
Level 1 (high-level) evidence
[45]
Elman MJ, Bressler NM, Qin H, Beck RW, Ferris FL 3rd, Friedman SM, Glassman AR, Scott IU, Stockdale CR, Sun JK, Diabetic Retinopathy Clinical Research Network. Expanded 2-year follow-up of ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2011 Apr:118(4):609-14. doi: 10.1016/j.ophtha.2010.12.033. Epub
[PubMed PMID: 21459214]
Level 2 (mid-level) evidence
[46]
Campochiaro PA, Heier JS, Feiner L, Gray S, Saroj N, Rundle AC, Murahashi WY, Rubio RG, BRAVO Investigators. Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010 Jun:117(6):1102-1112.e1. doi: 10.1016/j.ophtha.2010.02.021. Epub 2010 Apr 15
[PubMed PMID: 20398941]
[47]
Brown DM, Campochiaro PA, Singh RP, Li Z, Gray S, Saroj N, Rundle AC, Rubio RG, Murahashi WY, CRUISE Investigators. Ranibizumab for macular edema following central retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010 Jun:117(6):1124-1133.e1. doi: 10.1016/j.ophtha.2010.02.022. Epub 2010 Apr 9
[PubMed PMID: 20381871]
[48]
Do DV, Nguyen QD, Boyer D, Schmidt-Erfurth U, Brown DM, Vitti R, Berliner AJ, Gao B, Zeitz O, Ruckert R, Schmelter T, Sandbrink R, Heier JS, da Vinci Study Group. One-year outcomes of the da Vinci Study of VEGF Trap-Eye in eyes with diabetic macular edema. Ophthalmology. 2012 Aug:119(8):1658-65. doi: 10.1016/j.ophtha.2012.02.010. Epub 2012 Apr 24
[PubMed PMID: 22537617]
[49]
Brown DM, Schmidt-Erfurth U, Do DV, Holz FG, Boyer DS, Midena E, Heier JS, Terasaki H, Kaiser PK, Marcus DM, Nguyen QD, Jaffe GJ, Slakter JS, Simader C, Soo Y, Schmelter T, Yancopoulos GD, Stahl N, Vitti R, Berliner AJ, Zeitz O, Metzig C, Korobelnik JF. Intravitreal Aflibercept for Diabetic Macular Edema: 100-Week Results From the VISTA and VIVID Studies. Ophthalmology. 2015 Oct:122(10):2044-52. doi: 10.1016/j.ophtha.2015.06.017. Epub 2015 Jul 18
[PubMed PMID: 26198808]
[50]
Diabetic Retinopathy Clinical Research Network, Wells JA, Glassman AR, Ayala AR, Jampol LM, Aiello LP, Antoszyk AN, Arnold-Bush B, Baker CW, Bressler NM, Browning DJ, Elman MJ, Ferris FL, Friedman SM, Melia M, Pieramici DJ, Sun JK, Beck RW. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. The New England journal of medicine. 2015 Mar 26:372(13):1193-203. doi: 10.1056/NEJMoa1414264. Epub 2015 Feb 18
[PubMed PMID: 25692915]
[51]
Wells JA, Glassman AR, Ayala AR, Jampol LM, Bressler NM, Bressler SB, Brucker AJ, Ferris FL, Hampton GR, Jhaveri C, Melia M, Beck RW, Diabetic Retinopathy Clinical Research Network. Aflibercept, Bevacizumab, or Ranibizumab for Diabetic Macular Edema: Two-Year Results from a Comparative Effectiveness Randomized Clinical Trial. Ophthalmology. 2016 Jun:123(6):1351-9. doi: 10.1016/j.ophtha.2016.02.022. Epub 2016 Feb 27
[PubMed PMID: 26935357]
Level 2 (mid-level) evidence
[52]
Baker CW, Glassman AR, Beaulieu WT, Antoszyk AN, Browning DJ, Chalam KV, Grover S, Jampol LM, Jhaveri CD, Melia M, Stockdale CR, Martin DF, Sun JK, DRCR Retina Network. Effect of Initial Management With Aflibercept vs Laser Photocoagulation vs Observation on Vision Loss Among Patients With Diabetic Macular Edema Involving the Center of the Macula and Good Visual Acuity: A Randomized Clinical Trial. JAMA. 2019 May 21:321(19):1880-1894. doi: 10.1001/jama.2019.5790. Epub
[PubMed PMID: 31037289]
Level 1 (high-level) evidence
[53]
Clark WL, Boyer DS, Heier JS, Brown DM, Haller JA, Vitti R, Kazmi H, Berliner AJ, Erickson K, Chu KW, Soo Y, Cheng Y, Campochiaro PA. Intravitreal Aflibercept for Macular Edema Following Branch Retinal Vein Occlusion: 52-Week Results of the VIBRANT Study. Ophthalmology. 2016 Feb:123(2):330-336. doi: 10.1016/j.ophtha.2015.09.035. Epub 2015 Oct 30
[PubMed PMID: 26522708]
[54]
Brown DM, Heier JS, Clark WL, Boyer DS, Vitti R, Berliner AJ, Zeitz O, Sandbrink R, Zhu X, Haller JA. Intravitreal aflibercept injection for macular edema secondary to central retinal vein occlusion: 1-year results from the phase 3 COPERNICUS study. American journal of ophthalmology. 2013 Mar:155(3):429-437.e7. doi: 10.1016/j.ajo.2012.09.026. Epub 2012 Dec 4
[PubMed PMID: 23218699]
[55]
Korobelnik JF, Holz FG, Roider J, Ogura Y, Simader C, Schmidt-Erfurth U, Lorenz K, Honda M, Vitti R, Berliner AJ, Hiemeyer F, Stemper B, Zeitz O, Sandbrink R, GALILEO Study Group. Intravitreal Aflibercept Injection for Macular Edema Resulting from Central Retinal Vein Occlusion: One-Year Results of the Phase 3 GALILEO Study. Ophthalmology. 2014 Jan:121(1):202-208. doi: 10.1016/j.ophtha.2013.08.012. Epub 2013 Sep 29
[PubMed PMID: 24084497]
[56]
Dugel PU, Koh A, Ogura Y, Jaffe GJ, Schmidt-Erfurth U, Brown DM, Gomes AV, Warburton J, Weichselberger A, Holz FG, HAWK and HARRIER Study Investigators. HAWK and HARRIER: Phase 3, Multicenter, Randomized, Double-Masked Trials of Brolucizumab for Neovascular Age-Related Macular Degeneration. Ophthalmology. 2020 Jan:127(1):72-84. doi: 10.1016/j.ophtha.2019.04.017. Epub 2019 Apr 12
[PubMed PMID: 30986442]
Level 1 (high-level) evidence
[57]
Pearson PA, Comstock TL, Ip M, Callanan D, Morse LS, Ashton P, Levy B, Mann ES, Eliott D. Fluocinolone acetonide intravitreal implant for diabetic macular edema: a 3-year multicenter, randomized, controlled clinical trial. Ophthalmology. 2011 Aug:118(8):1580-7. doi: 10.1016/j.ophtha.2011.02.048. Epub
[PubMed PMID: 21813090]
Level 1 (high-level) evidence
[58]
Campochiaro PA, Brown DM, Pearson A, Chen S, Boyer D, Ruiz-Moreno J, Garretson B, Gupta A, Hariprasad SM, Bailey C, Reichel E, Soubrane G, Kapik B, Billman K, Kane FE, Green K, FAME Study Group. Sustained delivery fluocinolone acetonide vitreous inserts provide benefit for at least 3 years in patients with diabetic macular edema. Ophthalmology. 2012 Oct:119(10):2125-32. doi: 10.1016/j.ophtha.2012.04.030. Epub 2012 Jun 21
[PubMed PMID: 22727177]
[59]
Scott IU, Ip MS, VanVeldhuisen PC, Oden NL, Blodi BA, Fisher M, Chan CK, Gonzalez VH, Singerman LJ, Tolentino M, SCORE Study Research Group. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular Edema secondary to branch retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 6. Archives of ophthalmology (Chicago, Ill. : 1960). 2009 Sep:127(9):1115-28. doi: 10.1001/archophthalmol.2009.233. Epub
[PubMed PMID: 19752420]
Level 1 (high-level) evidence
[60]
Boyer DS, Yoon YH, Belfort R Jr, Bandello F, Maturi RK, Augustin AJ, Li XY, Cui H, Hashad Y, Whitcup SM, Ozurdex MEAD Study Group. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology. 2014 Oct:121(10):1904-14. doi: 10.1016/j.ophtha.2014.04.024. Epub 2014 Jun 4
[PubMed PMID: 24907062]
Level 1 (high-level) evidence
[61]
Gillies MC, Lim LL, Campain A, Quin GJ, Salem W, Li J, Goodwin S, Aroney C, McAllister IL, Fraser-Bell S. A randomized clinical trial of intravitreal bevacizumab versus intravitreal dexamethasone for diabetic macular edema: the BEVORDEX study. Ophthalmology. 2014 Dec:121(12):2473-81. doi: 10.1016/j.ophtha.2014.07.002. Epub 2014 Aug 22
[PubMed PMID: 25155371]
Level 1 (high-level) evidence
[62]
Haller JA, Bandello F, Belfort R Jr, Blumenkranz MS, Gillies M, Heier J, Loewenstein A, Yoon YH, Jacques ML, Jiao J, Li XY, Whitcup SM, OZURDEX GENEVA Study Group. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010 Jun:117(6):1134-1146.e3. doi: 10.1016/j.ophtha.2010.03.032. Epub 2010 Apr 24
[PubMed PMID: 20417567]
Level 1 (high-level) evidence
[63]
Maturi RK, Glassman AR, Liu D, Beck RW, Bhavsar AR, Bressler NM, Jampol LM, Melia M, Punjabi OS, Salehi-Had H, Sun JK, Diabetic Retinopathy Clinical Research Network. Effect of Adding Dexamethasone to Continued Ranibizumab Treatment in Patients With Persistent Diabetic Macular Edema: A DRCR Network Phase 2 Randomized Clinical Trial. JAMA ophthalmology. 2018 Jan 1:136(1):29-38. doi: 10.1001/jamaophthalmol.2017.4914. Epub
[PubMed PMID: 29127949]
Level 1 (high-level) evidence
[64]
Piccolino FC, De La Longrais RR, Manea M, Cicinelli S. Posterior cystoid retinal degeneration in central serous chorioretinopathy. Retina (Philadelphia, Pa.). 2008 Jul-Aug:28(7):1008-12. doi: 10.1097/IAE.0b013e31816b4b86. Epub
[PubMed PMID: 18698305]
[65]
Kessel L, Hamann S, Wegener M, Tong J, Fraser CL. Microcystic macular oedema in optic neuropathy: case series and literature review. Clinical & experimental ophthalmology. 2018 Dec:46(9):1075-1086. doi: 10.1111/ceo.13327. Epub 2018 Jun 20
[PubMed PMID: 29799159]
Level 2 (mid-level) evidence
[66]
Sipperley JO, Quigley HA, Gass DM. Traumatic retinopathy in primates. The explanation of commotio retinae. Archives of ophthalmology (Chicago, Ill. : 1960). 1978 Dec:96(12):2267-73
[PubMed PMID: 718521]
[67]
Sun JK, Lin MM, Lammer J, Prager S, Sarangi R, Silva PS, Aiello LP. Disorganization of the retinal inner layers as a predictor of visual acuity in eyes with center-involved diabetic macular edema. JAMA ophthalmology. 2014 Nov:132(11):1309-16. doi: 10.1001/jamaophthalmol.2014.2350. Epub
[PubMed PMID: 25058813]
[68]
Uji A, Murakami T, Nishijima K, Akagi T, Horii T, Arakawa N, Muraoka Y, Ellabban AA, Yoshimura N. Association between hyperreflective foci in the outer retina, status of photoreceptor layer, and visual acuity in diabetic macular edema. American journal of ophthalmology. 2012 Apr:153(4):710-7, 717.e1. doi: 10.1016/j.ajo.2011.08.041. Epub 2011 Dec 3
[PubMed PMID: 22137207]
[69]
Liang MC, Vora RA, Duker JS, Reichel E. Solid-appearing retinal cysts in diabetic macular edema: a novel optical coherence tomography finding. Retinal cases & brief reports. 2013 Summer:7(3):255-8. doi: 10.1097/ICB.0b013e31828eef49. Epub
[PubMed PMID: 25391118]
Level 3 (low-level) evidence
[70]
Kashani AH, Lee SY, Moshfeghi A, Durbin MK, Puliafito CA. OPTICAL COHERENCE TOMOGRAPHY ANGIOGRAPHY OF RETINAL VENOUS OCCLUSION. Retina (Philadelphia, Pa.). 2015 Nov:35(11):2323-31. doi: 10.1097/IAE.0000000000000811. Epub
[PubMed PMID: 26457395]
[71]
Forooghian F, Stetson PF, Meyer SA, Chew EY, Wong WT, Cukras C, Meyerle CB, Ferris FL 3rd. Relationship between photoreceptor outer segment length and visual acuity in diabetic macular edema. Retina (Philadelphia, Pa.). 2010 Jan:30(1):63-70. doi: 10.1097/IAE.0b013e3181bd2c5a. Epub
[PubMed PMID: 19952996]
[72]
Ota M, Nishijima K, Sakamoto A, Murakami T, Takayama K, Horii T, Yoshimura N. Optical coherence tomographic evaluation of foveal hard exudates in patients with diabetic maculopathy accompanying macular detachment. Ophthalmology. 2010 Oct:117(10):1996-2002. doi: 10.1016/j.ophtha.2010.06.019. Epub 2010 Aug 17
[PubMed PMID: 20723993]