[1]
Mok FP, Samartzis D, Karppinen J, Fong DY, Luk KD, Cheung KM. Modic changes of the lumbar spine: prevalence, risk factors, and association with disc degeneration and low back pain in a large-scale population-based cohort. The spine journal : official journal of the North American Spine Society. 2016 Jan 1:16(1):32-41. doi: 10.1016/j.spinee.2015.09.060. Epub 2015 Oct 8
[PubMed PMID: 26456851]
[2]
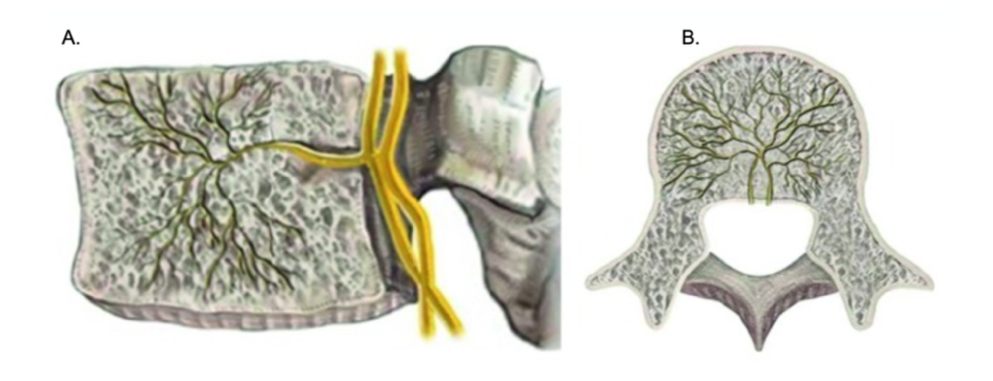
Kim HS, Wu PH, Jang IT. Lumbar Degenerative Disease Part 1: Anatomy and Pathophysiology of Intervertebral Discogenic Pain and Radiofrequency Ablation of Basivertebral and Sinuvertebral Nerve Treatment for Chronic Discogenic Back Pain: A Prospective Case Series and Review of Literature. International journal of molecular sciences. 2020 Feb 21:21(4):. doi: 10.3390/ijms21041483. Epub 2020 Feb 21
[PubMed PMID: 32098249]
Level 2 (mid-level) evidence
[3]
Tzika M, Paraskevas GK, Piagkou M, Papatolios AK, Natsis K. Basivertebral foramina of true vertebrae: morphometry, topography and clinical considerations. Surgical and radiologic anatomy : SRA. 2021 Jun:43(6):889-907. doi: 10.1007/s00276-021-02690-0. Epub 2021 Feb 17
[PubMed PMID: 33598754]
[4]
Kjaer P, Korsholm L, Bendix T, Sorensen JS, Leboeuf-Yde C. Modic changes and their associations with clinical findings. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2006 Sep:15(9):1312-9
[PubMed PMID: 16896838]
[5]
Weishaupt D, Zanetti M, Hodler J, Min K, Fuchs B, Pfirrmann CW, Boos N. Painful Lumbar Disk Derangement: Relevance of Endplate Abnormalities at MR Imaging. Radiology. 2001 Feb:218(2):420-7
[PubMed PMID: 11161156]
[6]
Fras C, Kravetz P, Mody DR, Heggeness MH. Substance P-containing nerves within the human vertebral body. an immunohistochemical study of the basivertebral nerve. The spine journal : official journal of the North American Spine Society. 2003 Jan-Feb:3(1):63-7
[PubMed PMID: 14589248]
[7]
Kuisma M, Karppinen J, Niinimäki J, Ojala R, Haapea M, Heliövaara M, Korpelainen R, Taimela S, Natri A, Tervonen O. Modic changes in endplates of lumbar vertebral bodies: prevalence and association with low back and sciatic pain among middle-aged male workers. Spine. 2007 May 1:32(10):1116-22
[PubMed PMID: 17471095]
[8]
Jensen RK, Leboeuf-Yde C. Is the presence of modic changes associated with the outcomes of different treatments? A systematic critical review. BMC musculoskeletal disorders. 2011 Aug 10:12():183. doi: 10.1186/1471-2474-12-183. Epub 2011 Aug 10
[PubMed PMID: 21831312]
Level 1 (high-level) evidence
[9]
Bailey JF, Liebenberg E, Degmetich S, Lotz JC. Innervation patterns of PGP 9.5-positive nerve fibers within the human lumbar vertebra. Journal of anatomy. 2011 Mar:218(3):263-70. doi: 10.1111/j.1469-7580.2010.01332.x. Epub 2011 Jan 12
[PubMed PMID: 21223256]
[10]
DePalma MJ, Ketchum JM, Saullo T. What is the source of chronic low back pain and does age play a role? Pain medicine (Malden, Mass.). 2011 Feb:12(2):224-33. doi: 10.1111/j.1526-4637.2010.01045.x. Epub 2011 Jan 25
[PubMed PMID: 21266006]
[11]
Lotz JC, Fields AJ, Liebenberg EC. The role of the vertebral end plate in low back pain. Global spine journal. 2013 Jun:3(3):153-64. doi: 10.1055/s-0033-1347298. Epub 2013 May 23
[PubMed PMID: 24436866]
[12]
Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine. 2006 Nov 1:31(23):2724-7
[PubMed PMID: 17077742]
Level 3 (low-level) evidence
[13]
Jensen TS, Karppinen J, Sorensen JS, Niinimäki J, Leboeuf-Yde C. Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2008 Nov:17(11):1407-22. doi: 10.1007/s00586-008-0770-2. Epub 2008 Sep 12
[PubMed PMID: 18787845]
Level 1 (high-level) evidence
[14]
Järvinen J, Karppinen J, Niinimäki J, Haapea M, Grönblad M, Luoma K, Rinne E. Association between changes in lumbar Modic changes and low back symptoms over a two-year period. BMC musculoskeletal disorders. 2015 Apr 22:16():98. doi: 10.1186/s12891-015-0540-3. Epub 2015 Apr 22
[PubMed PMID: 25897658]
[15]
Jensen RK, Leboeuf-Yde C, Wedderkopp N, Sorensen JS, Manniche C. Rest versus exercise as treatment for patients with low back pain and Modic changes. A randomized controlled clinical trial. BMC medicine. 2012 Feb 29:10():22. doi: 10.1186/1741-7015-10-22. Epub 2012 Feb 29
[PubMed PMID: 22376791]
Level 1 (high-level) evidence
[16]
Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. The spine journal : official journal of the North American Spine Society. 2008 Jan-Feb:8(1):8-20. doi: 10.1016/j.spinee.2007.10.005. Epub
[PubMed PMID: 18164449]
Level 1 (high-level) evidence
[17]
Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, Woolf A, Vos T, Buchbinder R. A systematic review of the global prevalence of low back pain. Arthritis and rheumatism. 2012 Jun:64(6):2028-37. doi: 10.1002/art.34347. Epub 2012 Jan 9
[PubMed PMID: 22231424]
Level 1 (high-level) evidence
[18]
Shayota B, Wong TL, Fru D, David G, Iwanaga J, Loukas M, Tubbs RS. A comprehensive review of the sinuvertebral nerve with clinical applications. Anatomy & cell biology. 2019 Jun:52(2):128-133. doi: 10.5115/acb.2019.52.2.128. Epub 2019 Jun 30
[PubMed PMID: 31338228]
[19]
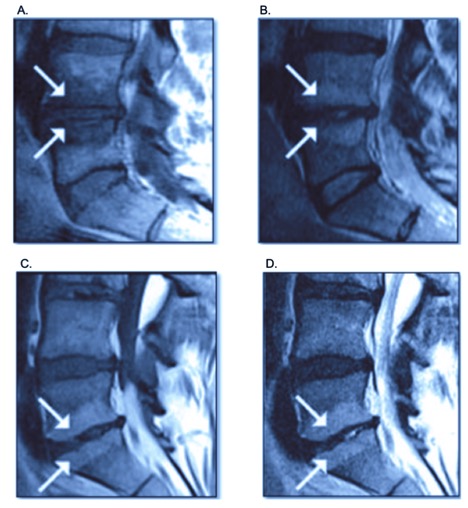
Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988 Jan:166(1 Pt 1):193-9
[PubMed PMID: 3336678]
[20]
Albert HB, Kjaer P, Jensen TS, Sorensen JS, Bendix T, Manniche C. Modic changes, possible causes and relation to low back pain. Medical hypotheses. 2008:70(2):361-8
[PubMed PMID: 17624684]
[21]
Applebaum A, Nessim A, Cho W. Modic Change: An Emerging Complication in the Aging Population. Clinical spine surgery. 2022 Feb 1:35(1):12-17. doi: 10.1097/BSD.0000000000001168. Epub
[PubMed PMID: 33769981]
[22]
Herlin C, Kjaer P, Espeland A, Skouen JS, Leboeuf-Yde C, Karppinen J, Niinimäki J, Sørensen JS, Storheim K, Jensen TS. Modic changes-Their associations with low back pain and activity limitation: A systematic literature review and meta-analysis. PloS one. 2018:13(8):e0200677. doi: 10.1371/journal.pone.0200677. Epub 2018 Aug 1
[PubMed PMID: 30067777]
Level 1 (high-level) evidence
[23]
Mera Y, Teraguchi M, Hashizume H, Oka H, Muraki S, Akune T, Kawaguchi H, Nakamura K, Tamai H, Tanaka S, Yoshida M, Yoshimura N, Yamada H. Association between types of Modic changes in the lumbar region and low back pain in a large cohort: the Wakayama spine study. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2021 Apr:30(4):1011-1017. doi: 10.1007/s00586-020-06618-x. Epub 2020 Oct 9
[PubMed PMID: 33037486]
[24]
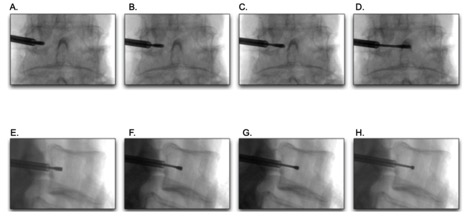
Fischgrund JS, Rhyne A, Franke J, Sasso R, Kitchel S, Bae H, Yeung C, Truumees E, Schaufele M, Yuan P, Vajkoczy P, Depalma M, Anderson DG, Thibodeau L, Meyer B. Intraosseous Basivertebral Nerve Ablation for the Treatment of Chronic Low Back Pain: 2-Year Results From a Prospective Randomized Double-Blind Sham-Controlled Multicenter Study. International journal of spine surgery. 2019 Apr:13(2):110-119. doi: 10.14444/6015. Epub 2019 Apr 30
[PubMed PMID: 31131209]
Level 2 (mid-level) evidence
[25]
Khalil JG, Smuck M, Koreckij T, Keel J, Beall D, Goodman B, Kalapos P, Nguyen D, Garfin S, INTRACEPT Trial Investigators. A prospective, randomized, multicenter study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain. The spine journal : official journal of the North American Spine Society. 2019 Oct:19(10):1620-1632. doi: 10.1016/j.spinee.2019.05.598. Epub 2019 Jun 20
[PubMed PMID: 31229663]
Level 2 (mid-level) evidence
[26]
Markman JD, Rhyne AL, Sasso RC, Patel AA, Hsu WK, Fischgrund JS, Edidin AA, Vajkoczy P. Association Between Opioid Use and Patient-Reported Outcomes in a Randomized Trial Evaluating Basivertebral Nerve Ablation for the Relief of Chronic Low Back Pain. Neurosurgery. 2020 Mar 1:86(3):343-347. doi: 10.1093/neuros/nyz093. Epub
[PubMed PMID: 31034561]
Level 1 (high-level) evidence
[27]
Truumees E, Macadaeg K, Pena E, Arbuckle J 2nd, Gentile J 2nd, Funk R, Singh D, Vinayek S. A prospective, open-label, single-arm, multi-center study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2019 Jul:28(7):1594-1602. doi: 10.1007/s00586-019-05995-2. Epub 2019 May 21
[PubMed PMID: 31115683]
[28]
Fischgrund JS, Rhyne A, Macadaeg K, Moore G, Kamrava E, Yeung C, Truumees E, Schaufele M, Yuan P, DePalma M, Anderson DG, Buxton D, Reynolds J, Sikorsky M. Long-term outcomes following intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 5-year treatment arm results from a prospective randomized double-blind sham-controlled multi-center study. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2020 Aug:29(8):1925-1934. doi: 10.1007/s00586-020-06448-x. Epub 2020 May 25
[PubMed PMID: 32451777]
Level 1 (high-level) evidence
[29]
De Vivo AE, D'Agostino G, D'Anna G, Al Qatami H, Gil I, Ventura F, Manfrè L. Intra-osseous basivertebral nerve radiofrequency ablation (BVA) for the treatment of vertebrogenic chronic low back pain. Neuroradiology. 2021 May:63(5):809-815. doi: 10.1007/s00234-020-02577-8. Epub 2020 Oct 13
[PubMed PMID: 33051706]
[30]
Smuck M, Khalil J, Barrette K, Hirsch JA, Kreiner S, Koreckij T, Garfin S, Mekhail N, INTRACEPT Trial Investigators. Prospective, randomized, multicenter study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 12-month results. Regional anesthesia and pain medicine. 2021 Aug:46(8):683-693. doi: 10.1136/rapm-2020-102259. Epub 2021 May 24
[PubMed PMID: 34031220]
Level 2 (mid-level) evidence
[31]
Kim HS, Adsul N, Yudoyono F, Paudel B, Kim KJ, Choi SH, Kim JH, Chung SK, Choi JH, Jang JS, Jang IT, Oh SH. Transforaminal Epiduroscopic Basivertebral Nerve Laser Ablation for Chronic Low Back Pain Associated with Modic Changes: A Preliminary Open-Label Study. Pain research & management. 2018:2018():6857983. doi: 10.1155/2018/6857983. Epub 2018 Aug 14
[PubMed PMID: 30186540]
[32]
Nguyen KML, Nguyen DTD. Minimally Invasive Treatment for Degenerative Lumbar Spine. Techniques in vascular and interventional radiology. 2020 Dec:23(4):100700. doi: 10.1016/j.tvir.2020.100700. Epub 2020 Oct 5
[PubMed PMID: 33308584]
[33]
Urits I, Noor N, Johal AS, Leider J, Brinkman J, Fackler N, Vij N, An D, Cornett EM, Kaye AD, Viswanath O. Basivertebral Nerve Ablation for the Treatment of Vertebrogenic Pain. Pain and therapy. 2021 Jun:10(1):39-53. doi: 10.1007/s40122-020-00211-2. Epub 2020 Oct 31
[PubMed PMID: 33128702]
[34]
Conger A, Schuster NM, Cheng DS, Sperry BP, Joshi AB, Haring RS, Duszynski B, McCormick ZL. The Effectiveness of Intraosseous Basivertebral Nerve Radiofrequency Neurotomy for the Treatment of Chronic Low Back Pain in Patients with Modic Changes: A Systematic Review. Pain medicine (Malden, Mass.). 2021 May 21:22(5):1039-1054. doi: 10.1093/pm/pnab040. Epub
[PubMed PMID: 33544851]
Level 1 (high-level) evidence
[35]
Lorio M, Clerk-Lamalice O, Beall DP, Julien T. International Society for the Advancement of Spine Surgery Guideline-Intraosseous Ablation of the Basivertebral Nerve for the Relief of Chronic Low Back Pain. International journal of spine surgery. 2020 Feb:14(1):18-25. doi: 10.14444/7002. Epub 2020 Feb 29
[PubMed PMID: 32128298]