[1]
Opfer E, Shah S. Advances in Pediatric Cardiovascular Imaging. Missouri medicine. 2018 Jul-Aug:115(4):354-360
[PubMed PMID: 30228767]
Level 3 (low-level) evidence
[2]
Benavidez OJ, Gauvreau K, Jenkins KJ, Geva T. Diagnostic errors in pediatric echocardiography: development of taxonomy and identification of risk factors. Circulation. 2008 Jun 10:117(23):2995-3001. doi: 10.1161/CIRCULATIONAHA.107.758532. Epub 2008 Jun 2
[PubMed PMID: 18519849]
[3]
Hoffman JI,Kaplan S, The incidence of congenital heart disease. Journal of the American College of Cardiology. 2002 Jun 19;
[PubMed PMID: 12084585]
[4]
Campbell RM, Douglas PS, Eidem BW, Lai WW, Lopez L, Sachdeva R. ACC/AAP/AHA/ASE/HRS/SCAI/SCCT/SCMR/SOPE 2014 appropriate use criteria for initial transthoracic echocardiography in outpatient pediatric cardiology: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Academy of Pediatrics, American Heart Association, American Society of Echocardiography, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Pediatric Echocardiography. Journal of the American College of Cardiology. 2014 Nov 11:64(19):2039-60. doi: 10.1016/j.jacc.2014.08.003. Epub 2014 Sep 29
[PubMed PMID: 25277848]
[5]
Sachdeva R, Valente AM, Armstrong AK, Cook SC, Han BK, Lopez L, Lui GK, Pickard SS, Powell AJ, Bhave NM, Sachdeva R, Valente AM, Pickard SS, Baffa JM, Banka P, Cohen SB, Glickstein JS, Kanter JP, Kanter RJ, Kim YY, Kipps AK, Latson LA, Lin JP, Parra DA, Rodriguez FH 3rd, Saarel EV, Srivastava S, Stephenson EA, Stout KK, Zaidi AN. ACC/AHA/ASE/HRS/ISACHD/SCAI/SCCT/SCMR/SOPE 2020 Appropriate Use Criteria for Multimodality Imaging During the Follow-Up Care of Patients With Congenital Heart Disease: A Report of the American College of Cardiology Solution Set Oversight Committee and Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Pediatric Echocardiography. Journal of the American College of Cardiology. 2020 Feb 18:75(6):657-703. doi: 10.1016/j.jacc.2019.10.002. Epub 2020 Jan 6
[PubMed PMID: 31918898]
[6]
Cheitlin MD, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, Davis JL, Douglas PS, Faxon DP, Gillam LD, Kimball TR, Kussmaul WG, Pearlman AS, Philbrick JT, Rakowski H, Thys DM, Antman EM, Smith SC Jr, Alpert JS, Gregoratos G, Anderson JL, Hiratzka LF, Hunt SA, Fuster V, Jacobs AK, Gibbons RJ, Russell RO, American College of Cardiology, American Heart Association, American Society of Echocardiography. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation. 2003 Sep 2:108(9):1146-62
[PubMed PMID: 12952829]
Level 1 (high-level) evidence
[7]
Tissot C, Muehlethaler V, Sekarski N. Basics of Functional Echocardiography in Children and Neonates. Frontiers in pediatrics. 2017:5():235. doi: 10.3389/fped.2017.00235. Epub 2017 Dec 1
[PubMed PMID: 29250515]
[8]
Ni JR, Yan PJ, Liu SD, Hu Y, Yang KH, Song B, Lei JQ. Diagnostic accuracy of transthoracic echocardiography for pulmonary hypertension: a systematic review and meta-analysis. BMJ open. 2019 Dec 22:9(12):e033084. doi: 10.1136/bmjopen-2019-033084. Epub 2019 Dec 22
[PubMed PMID: 31871259]
Level 1 (high-level) evidence
[9]
Kitada R, Fukuda S, Watanabe H, Oe H, Abe Y, Yoshiyama M, Song JM, Sitges M, Shiota T, Ito H, Yoshikawa J. Diagnostic accuracy and cost-effectiveness of a pocket-sized transthoracic echocardiographic imaging device. Clinical cardiology. 2013 Oct:36(10):603-10. doi: 10.1002/clc.22171. Epub 2013 Jul 24
[PubMed PMID: 23893844]
[10]
Li RJ, Sun Z, Yang J, Yang Y, Li YJ, Leng ZT, Liu GW, Pu LH. Diagnostic Value of Transthoracic Echocardiography in Patients With Anomalous Origin of the Left Coronary Artery From the Pulmonary Artery. Medicine. 2016 Apr:95(15):e3401. doi: 10.1097/MD.0000000000003401. Epub
[PubMed PMID: 27082616]
[11]
O'Byrne ML, Glatz AC, Goldberg DJ, Shinohara R, Dori Y, Rome JJ, Gillespie MJ. Accuracy of Transthoracic Echocardiography in Assessing Retro-aortic Rim prior to Device Closure of Atrial Septal Defects. Congenital heart disease. 2015 Jul-Aug:10(4):E146-54. doi: 10.1111/chd.12226. Epub 2014 Sep 16
[PubMed PMID: 25227430]
[12]
Kabirdas D, Scridon C, Brenes JC, Hernandez AV, Novaro GM, Asher CR. Accuracy of transthoracic echocardiography for the measurement of the ascending aorta: comparison with transesophageal echocardiography. Clinical cardiology. 2010 Aug:33(8):502-7. doi: 10.1002/clc.20807. Epub
[PubMed PMID: 20734448]
[13]
Monin JL, Dehant P, Roiron C, Monchi M, Tabet JY, Clerc P, Fernandez G, Houel R, Garot J, Chauvel C, Gueret P. Functional assessment of mitral regurgitation by transthoracic echocardiography using standardized imaging planes diagnostic accuracy and outcome implications. Journal of the American College of Cardiology. 2005 Jul 19:46(2):302-9
[PubMed PMID: 16022959]
[14]
Parlakay AO, Karagöz T, Ozkutlu S, Ozen S, Alehan D, Yiğit S. Evaluation of diagnostic accuracy of portable echocardiography in newborns. Anadolu kardiyoloji dergisi : AKD = the Anatolian journal of cardiology. 2011 Nov:11(7):627-32. doi: 10.5152/akd.2011.167. Epub 2011 Sep 29
[PubMed PMID: 21959878]
[15]
Sluysmans T, Colan SD. Theoretical and empirical derivation of cardiovascular allometric relationships in children. Journal of applied physiology (Bethesda, Md. : 1985). 2005 Aug:99(2):445-57
[PubMed PMID: 15557009]
[16]
Daubeney PE, Blackstone EH, Weintraub RG, Slavik Z, Scanlon J, Webber SA. Relationship of the dimension of cardiac structures to body size: an echocardiographic study in normal infants and children. Cardiology in the young. 1999 Jul:9(4):402-10
[PubMed PMID: 10476831]
[17]
Pettersen MD, Du W, Skeens ME, Humes RA. Regression equations for calculation of z scores of cardiac structures in a large cohort of healthy infants, children, and adolescents: an echocardiographic study. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2008 Aug:21(8):922-34. doi: 10.1016/j.echo.2008.02.006. Epub 2008 Apr 11
[PubMed PMID: 18406572]
[18]
Kaski JP, Daubeney PE. Normalization of echocardiographically derived paediatric cardiac dimensions to body surface area: time for a standardized approach. European journal of echocardiography : the journal of the Working Group on Echocardiography of the European Society of Cardiology. 2009 Jan:10(1):44-5. doi: 10.1093/ejechocard/jen242. Epub 2008 Sep 30
[PubMed PMID: 18827032]
[19]
Gokhroo RK, Anantharaj A, Bisht D, Kishor K, Plakkal N, Mondal N. A pediatric echocardiographic Z-score nomogram for a developing country: Indian pediatric echocardiography study - The Z-score. Annals of pediatric cardiology. 2018 Jan-Apr:11(1):109-111. doi: 10.4103/apc.APC_123_17. Epub
[PubMed PMID: 29440845]
[20]
Cantinotti M, Scalese M, Giordano R, Assanta N, Marchese P, Franchi E, Viacava C, Koestenberger M, Jani V, Kutty S. A statistical comparison of reproducibility in current pediatric two-dimensional echocardiographic nomograms. Pediatric research. 2021 Feb:89(3):579-590. doi: 10.1038/s41390-020-0900-z. Epub 2020 Apr 24
[PubMed PMID: 32330930]
[21]
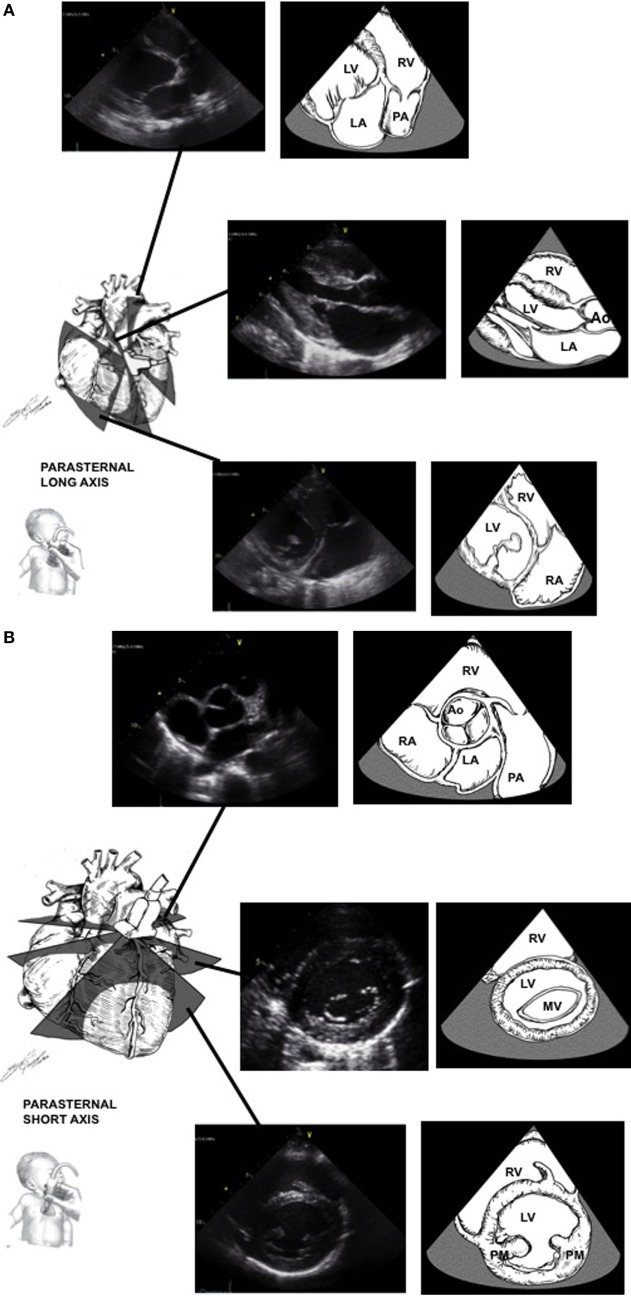
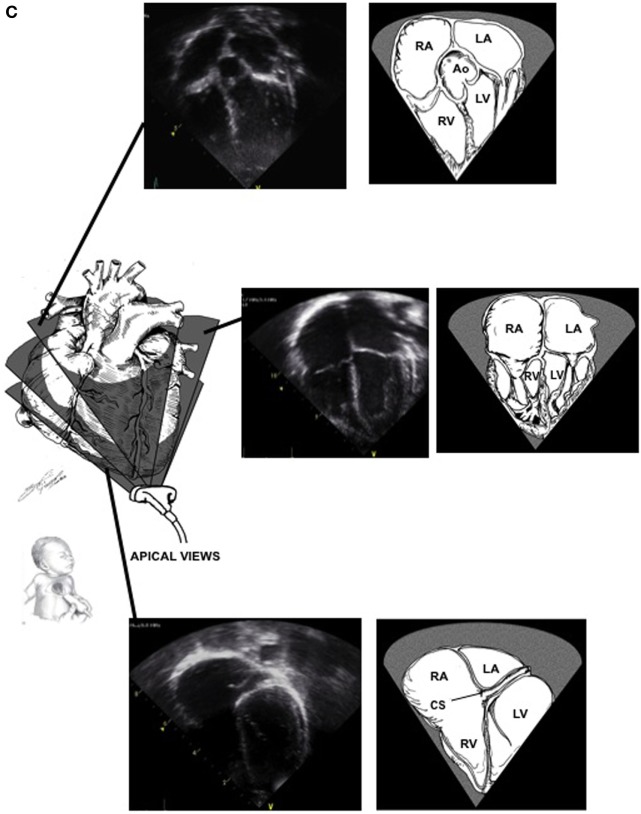
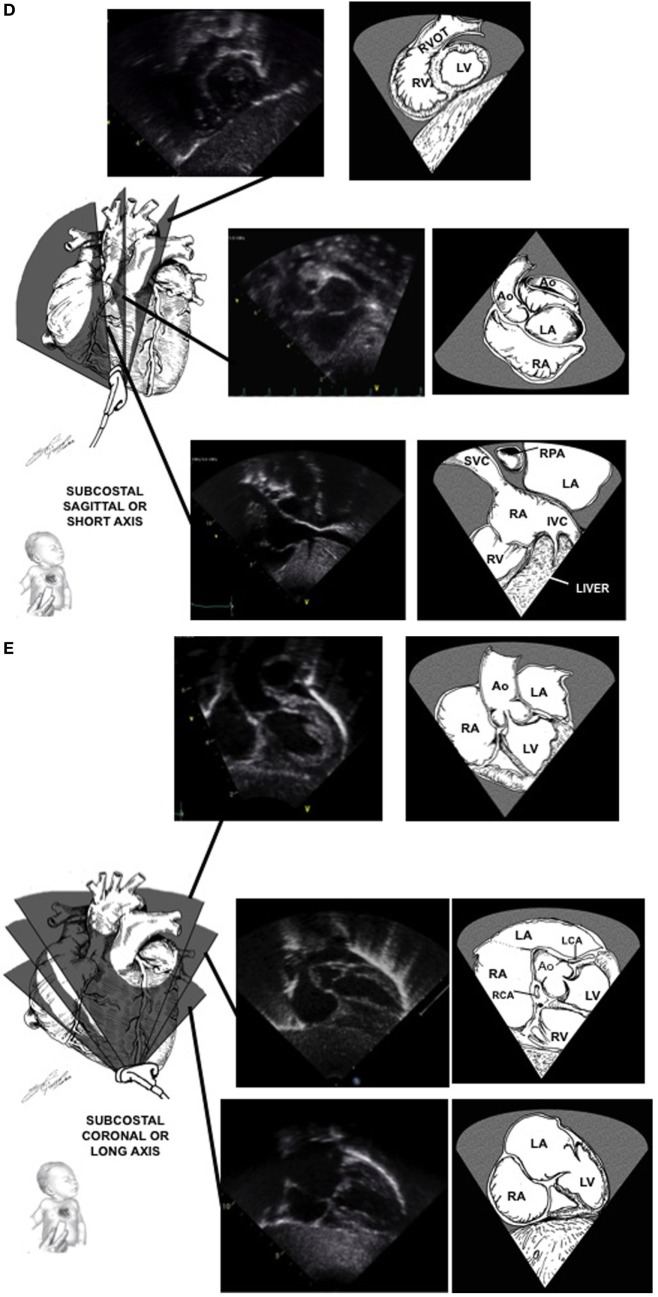
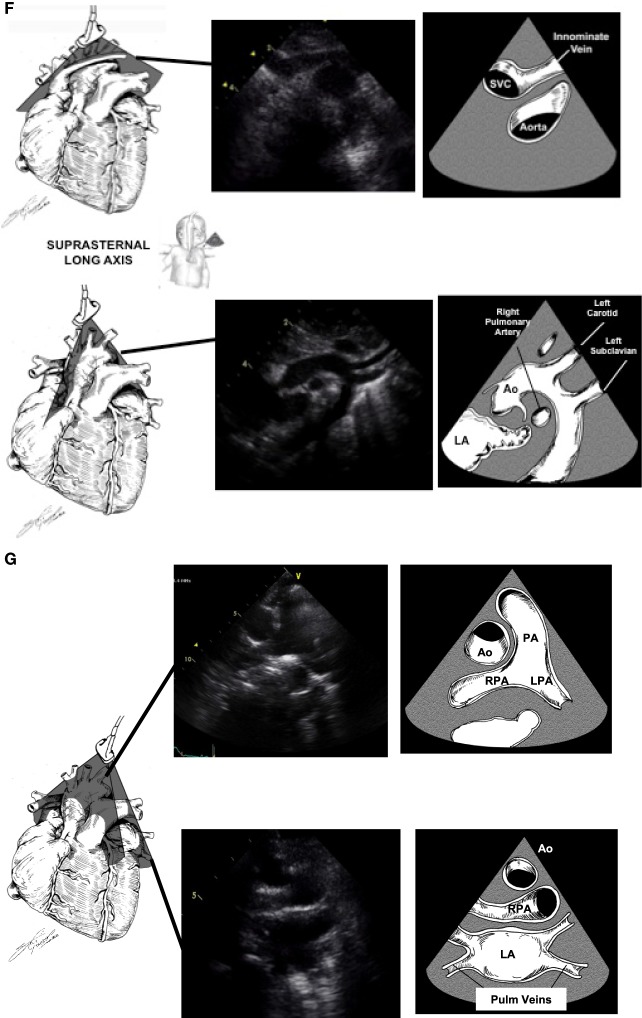
Lai WW, Geva T, Shirali GS, Frommelt PC, Humes RA, Brook MM, Pignatelli RH, Rychik J, Task Force of the Pediatric Council of the American Society of Echocardiography, Pediatric Council of the American Society of Echocardiography. Guidelines and standards for performance of a pediatric echocardiogram: a report from the Task Force of the Pediatric Council of the American Society of Echocardiography. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2006 Dec:19(12):1413-30
[PubMed PMID: 17138024]
[22]
Gardin JM, Adams DB, Douglas PS, Feigenbaum H, Forst DH, Fraser AG, Grayburn PA, Katz AS, Keller AM, Kerber RE, Khandheria BK, Klein AL, Lang RM, Pierard LA, Quinones MA, Schnittger I, American Society of Echocardiography. Recommendations for a standardized report for adult transthoracic echocardiography: a report from the American Society of Echocardiography's Nomenclature and Standards Committee and Task Force for a Standardized Echocardiography Report. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2002 Mar:15(3):275-90
[PubMed PMID: 11875394]
[23]
Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P, Moon-Grady AJ, Coon PD, Noori S, Simpson J, Lai WW, Writing Group of the American Society of Echocardiography, European Association of Echocardiography, Association for European Pediatric Cardiologists. Targeted Neonatal Echocardiography in the Neonatal Intensive Care Unit: practice guidelines and recommendations for training. Writing Group of the American Society of Echocardiography (ASE) in collaboration with the European Association of Echocardiography (EAE) and the Association for European Pediatric Cardiologists (AEPC). Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2011 Oct:24(10):1057-78. doi: 10.1016/j.echo.2011.07.014. Epub
[PubMed PMID: 21933743]
Level 1 (high-level) evidence
[24]
Singh Y, Katheria A, Tissot C. Functional Echocardiography in the Neonatal Intensive Care Unit. Indian pediatrics. 2018 May 15:55(5):417-424
[PubMed PMID: 29845957]
[25]
Gaspar HA, Morhy SS. The Role of Focused Echocardiography in Pediatric Intensive Care: A Critical Appraisal. BioMed research international. 2015:2015():596451. doi: 10.1155/2015/596451. Epub 2015 Oct 28
[PubMed PMID: 26605333]
[26]
Williams JL, Raees MA, Sunthankar S, Killen SAS, Bichell D, Parra DA, Soslow JH. Sedated Echocardiograms Better Characterize Branch Pulmonary Arteries Following Bidirectional Glenn Palliation with Minimal Risk of Adverse Events. Pediatric cardiology. 2020 Jun:41(5):955-961. doi: 10.1007/s00246-020-02342-x. Epub 2020 Apr 4
[PubMed PMID: 32248280]