Continuing Education Activity
Scalp vein catheterization is a valuable procedure offering an alternative site for peripheral intravenous access, particularly in cases where traditional extremity access is challenging or not feasible. This is a safe and efficient method for administering medications and fluids, making it crucial for certain patient populations, such as those without extremities or those with difficult peripheral access. The procedure involves selecting visible scalp veins, following proper aseptic techniques, and securing the catheter.
Clinicians participating in this continuing education activity on scalp vein catheterization can expect to gain comprehensive insights into the procedural intricacies, including patient evaluation, site selection, aseptic protocols, and catheter insertion techniques. This activity enhances proficiency in scalp vein catheterization, allowing for improved patient outcomes, increased procedural success rates, and a broader skill set for addressing specific challenges in various patient populations. The activity equips clinicians with the knowledge and competence necessary to perform this procedure safely and effectively, expanding their toolkit for intravenous access in challenging scenarios. By engaging in this course, healthcare professionals collaborate across disciplines to improve competence in scalp vein catheterization. This interprofessional approach ensures comprehensive patient care, with team members contributing their expertise to enhance procedural success rates and patient outcomes.
Objectives:
Differentiate between contraindications and indications for scalp vein catheterization, understanding when it is a safe and efficient option compared to traditional peripheral access.
Apply patient anatomy and vein characteristics knowledge to select an optimal site for catheter insertion, considering visibility, vein caliber, and straight-path accessibility.
Implement proficiency in the procedural aspects of scalp vein catheterization, including proper aseptic techniques, site selection, and catheter insertion, ensuring patient safety and procedural success.
Coordinate with colleagues to ensure a systematic approach to scalp vein catheterization, promoting a standardized and efficient process across healthcare settings.
Introduction
Peripheral intravenous (IV) catheterization is an essential procedure performed by various healthcare team members, providing access for blood sampling and direct administration of fluids and medications to the patient. While traditional sites in the extremities are common, obtaining peripheral IV access through scalp veins is an alternative. Despite being less frequently used, scalp IV catheterizations offer efficiency and safety. Understanding the distinctive considerations for scalp IV access is essential for successfully implementing this viable option, expanding the range of choices available to medical practitioners.[1]
Anatomy and Physiology
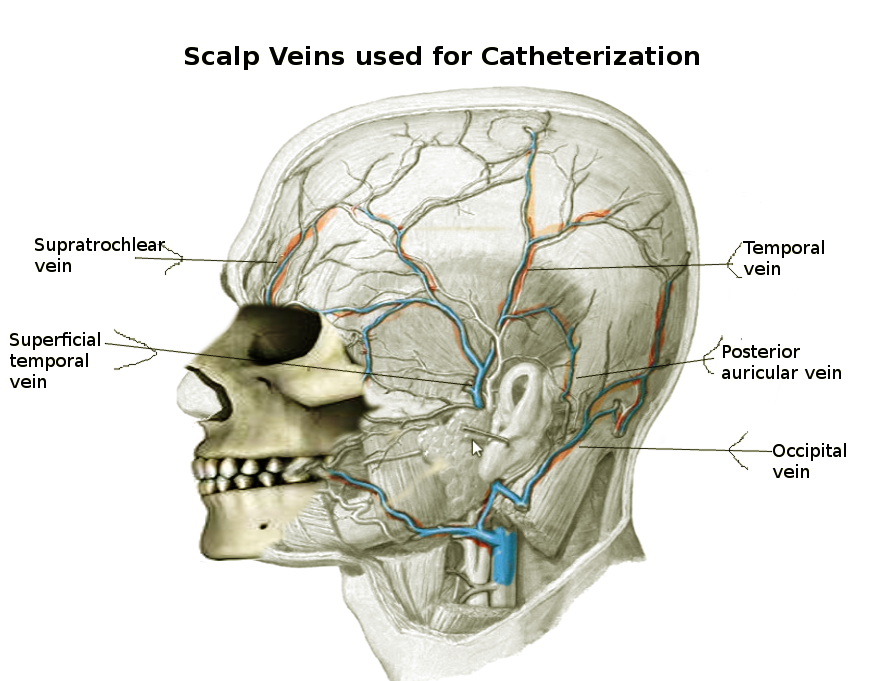
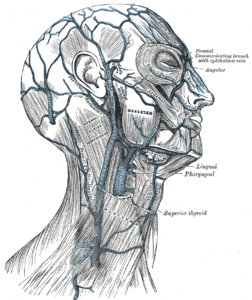
Veins are crucial in returning deoxygenated blood to the heart within the circulatory system. Peripheral veins, positioned close to the skin's surface, offer convenient access to the circulatory system. Scalp veins, with their superficial location and easy visibility, provide accessibility for catheterization. The 3 primary veins commonly targeted for scalp vein catheterization in peripheral IV access are the posterior auricular veins, superficial temporal veins, and frontal veins (see Image. Scalp Veins and see Image. Veins of the Scalp).[2] Frontal veins extend vertically along the forehead's center, while superficial temporal veins course along the head's side, draining the temporal region's skin and muscles. Posterior auricular veins, parallel to the cranial-caudal axis, serve the skin and superficial scalp muscles, running posteriorly to the ear.
Indications
Like other peripheral IV catheterizations, scalp vein catheterization serves the purpose of sampling blood for laboratory analysis and providing direct access to the circulatory system for infusing IV fluids, blood products, or medications. Typically, extremities are the primary sites explored for peripheral IV catheterization. However, scalp vein cannulation becomes essential in young patients, necessitating IV administration when peripheral access in the extremities is impossible.[3] Scalp vein catheterization is also viable for patients lacking limbs (eg, phocomelia) or facing difficulties in obtaining peripheral IV access in the arms or legs. While peripheral vein catheterization is generally suitable for short-term use (≤72 hours), whether in extremities or scalp veins, the latter is ideal for smaller caliber catheters in short-term access scenarios.[3] Additionally, direct percutaneous scalp vein catheterization finds application in the endovascular treatment of arteriovenous malformations involving the scalp.[4]
Contraindications
Relative contraindications encompass overlying skin infections and thrombophlebitis at the catheterization site. Careful attention should be paid to patient discomfort, whether related to the catheterization process or the continuous presence of hardware maintaining the catheter position, as well as potential sensory or motor deficits around the chosen site. As with any superficial vein catheterization procedure, a thorough consideration of risks and benefits is essential. Despite these considerations, peripheral IV catheterization remains crucial for emergent and life-saving access to administer medications, fluids, and blood products, prioritizing clinical urgency in emergency settings.
Equipment
For scalp vein catheterization, the following equipment is required:
- Gauze
- Gloves
- Hair clippers
- Chlorhexidine or alcohol swabs
- An elastic constricting tourniquet of thin caliber (eg, a rubber band)
- An appropriately gauged IV catheter
- Transparent film dressing
- Tape
- Syringe (for blood collection as necessary)
- Saline flush
- IV tubing
- Tubing extension set
- Saline lock
Personnel
Scalp vein catheterization requires the expertise of an individual authorized and experienced in IV catheterization, given that scalp veins are not typically the primary access site. When exploring scalp veins for peripheral IV access, urgency often underscores the need for successful catheterization, making it advisable to utilize personnel with extensive experience. Generally, a technician, medic, nurse, or clinician is qualified to perform the procedure. In pediatric cases, additional trained personnel may be required to stabilize the child, and child life specialists can contribute by offering distraction or developmentally appropriate support.
Preparation
Adherence to universal precautions and aseptic techniques is crucial for all procedures, including scalp vein catheterization. Proper positioning for finding appropriate scalp veins for catheterization in children and adults involves:
- Minimizing neck mobility
- Reducing body movements during IV catheter placement
- Maintaining the head at the appropriate angle for a straight path to the scalp vein [5]
- Site selection is the key first step before scalp vein catheterization
After eliminating sites that may pose potential contraindications, choosing a visible vein with adequate caliber to accommodate the catheter is imperative. Optimal success is achieved when selecting a vein that follows a relatively straight path, as tortuous veins can complicate the advancement of the catheter. This strategic approach ensures procedural efficiency and minimizes challenges during catheterization.
Rapid superficial vein assessment (RaSuVA) is intended to provide a comprehensive preprocedural examination of all newborn superficial veins to allow a reasonable choice of the optimal insertion site suited to the individual patient and optimized for the specific type of venous access device. The superficial veins are methodically inspected, both with and without near-infrared technology, and 7 skin locations are explored in the following order:
- Medial malleolus
- Lateral malleolus
- Retropopliteal fossa
- Back of the hand and wrist
- Antecubital fossa
- Anterior scalp surface
- Posterior scalp surface [6]
Ultrasound guidance, administered by trained personnel, can be crucial for enhancing the success of scalp vein catheterization. An elastic band around the scalp, like a rubber band, is recommended. The optimal placement of this band is caudal to the catheterization site, and gentle pressure can be applied manually or with an assistant's help. If using a circumferential band, it should be positioned distal to the catheterization site but superior to the ears and eyes, avoiding compression of these areas. This compressive application aids in vein distension and enhances visualization. Clipping or shaving hair, especially if the site is within the hair, ensures maximal visualization and reduces the risk of visible scars. Following site identification, meticulous skin preparation with alcohol or chlorhexidine is essential, adhering to aseptic protocols for blood culture acquisition. Consistent utilization of aseptic techniques, including gloves, should be maintained throughout the procedure.
Technique or Treatment
Once the site is selected and prepared, unsheath the catheter and align it with the chosen vein. Maintain the bevel of the needle upwards, angled approximately 30° from the skin's surface, and advance it as the needle pierces the skin. Continue advancing toward the vein until blood appears in the chamber, indicating a successful vein puncture. Adjust the catheter's angle to approximately 10° above the skin and advance it into the vein. After ensuring proper catheter placement, retract the needle while maintaining the catheter position, applying distal pressure on the vein to prevent blood leakage.[7]
Consider applying a transparent film dressing over the catheter hub to secure the catheter. Attach a syringe, IV tubing, or other connectors as needed, flush the catheter with saline, and monitor the site for fluid extravasation and appropriate catheter positioning—place gauze under the catheter hub to prevent scalp compression and tape it securely. Given the head's shape, location, and movement, consider stabilizing the scalp vein catheter with a plastic medicine cup, cut and taped over the catheter, as an example.
Complications
Most complications from scalp vein catheterization are similar to other peripheral IV access complications: pain, bleeding, including hematoma, and infection. Rarer complications include extravasation of fluids or medication, phlebitis, thrombophlebitis, penetration of deeper structures or damage to surrounding tissues, nerve damage, or embolism.[8] Specific to scalp vein catheterization are rare complications related to the site of IV catheterization. Case reports of intracranial air, epidural infection, and the introduction of air into the cavernous sinus are some of the complications that have been reported.[9][10][11][12][13]
Clinical Significance
IV catheterization is a crucial, life-preserving procedure necessary for drug and fluid administration. Scalp veins provide a safe and reliable alternative for establishing peripheral IV access, especially in patients without extremities or facing challenges with extremity IV access, as long as more invasive options are not warranted.
The insertion of peripherally inserted central catheters through scalp veins is a feasible option without higher complication rates than other sites.[14] In specific cases, administering a single prophylactic dose of vancomycin in infants before line removal can reduce sepsis incidence.[15]
Enhancing Healthcare Team Outcomes
Scalp vein catheterization involves a collaborative effort among various healthcare professionals to ensure patient-centered care, optimize outcomes, prioritize safety, and enhance overall team performance. Physicians, advanced practitioners, nurses, pharmacists, and other health professionals play distinct roles in the procedure. Physicians are responsible for proper patient evaluation, determining the need for catheterization, and overseeing the procedure. Advanced practitioners and nurses are involved in hands-on catheterization, requiring skills in site selection, aseptic technique, and catheter insertion. Pharmacists contribute by ensuring appropriate drug administration protocols. Child life specialists may help provide comfort and distraction during the procedure in cases with children. Effective communication between all team members is essential for seamless coordination. This collaborative approach fosters patient safety, improves outcomes, and promotes a patient-centered care environment.