Indications
Barbiturates are a category of sedative-hypnotic medications used for treating seizure disorders, neonatal withdrawal, insomnia, preoperative anxiety, and the induction of coma to address increased intracranial pressure (ICP). In addition, these medications are also helpful for inducing anesthesia. Thiopental was introduced in 1934 for general anesthesia induction.[1] This drug was the predominant intravenous (IV) anesthetic induction agent until propofol replaced it.[2] In refractory status epilepticus, a Cochrane Review found that thiopental was equally effective as propofol for controlling seizure activity.[3] In 2011, the primary supplier of thiopental chose to cease its production due to its involvement in lethal injection procedures, resulting in its unavailability in the United States.[4]
FDA-Approved Indications
Barbiturates approved by the US Food and Drug Administration (FDA) for clinical use are provided below.
Phenobarbital: Phenobarbitone has extensive use as an antiepileptic drug in the neonatal and pediatric population. It is the most cost-effective drug treatment for epilepsy in adults in low-resource countries.[5] IV barbiturates have been used for neurosurgery due to reduced cerebral metabolic rate of oxygen consumption.[6] For individuals with severe traumatic brain injury (TBI), high-dose barbiturates may be a consideration but are not indicated for prophylactic administration.[7] In a review of practice in 5 European countries, about 20% of patients received barbiturates.[8]
In refractory status epilepticus, a Cochrane Review found that thiopental was equally effective as propofol for controlling seizure activity.[3] A systematic review and meta-analysis evaluated interventions for benzodiazepine-resistant status epilepticus in both children and adults. Among the studied interventions, phenobarbital and high-dose levetiracetam were superior to phenytoin in achieving seizure cessation within 60 minutes. Phenobarbital is effective, but concerns about its safety profile exist, including cardiovascular instability.[9]
Methohexital: Methohexital has demonstrated safety and efficacy for procedural sedation of short duration for cardioversion and pediatric outpatient surgery.[10][11] Methohexital can be used for fracture reduction in the emergency department and sedation for elective intubation in neonates.[12][13] Methohexital has preferential use in electroconvulsive therapy due to longer seizure duration.[6]
Butalbital: Butalbital is used primarily for the treatment of headache disorders. The combination of butalbital and acetaminophen is approved for relieving symptoms associated with tension-type headaches.[14] A combination of acetaminophen-butalbital-caffeine is also available. Severe acetaminophen-butalbital-caffeine withdrawal has been described.[15] The combination of butalbital-aspirin-caffeine is FDA-approved for tension-type headaches. Medications incorporating butalbital demonstrate a 2-fold increased risk for the development of medication overuse headaches when contrasted with the usage of simple analgesics and triptans.[16][17]
Pentobarbital: Pentobarbital is used as a pre-anesthetic medication for status epilepticus.[18] Pentobarbital is used off-label for TBI associated with refractory elevated ICP.[19]
Primidone: Primidone is prescribed for the treatment of seizure disorders. According to the American Academy of Neurology (AAN), the choice between primidone (a barbiturate) and propranolol for essential tremors depends on comorbidities and potential adverse drug reactions.[20]
Amobarbital: Amobarbital has a labeled indication for insomnia, but the American Association of Sleep Medicine does not endorse its use.[21]
Mechanism of Action
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Mechanism of Action
Barbiturates cause postsynaptic enhancement of gamma-aminobutyric acid (GABA), interacting with alpha- and beta subunits of the GABA-A receptor.[22] Barbiturates increase chloride ion flux, resulting in postsynaptic hyperpolarization and central nervous system (CNS) depression. Phenobarbital and pentobarbital affect the GABA-A receptors with a dose-dependent response. These drugs activate chloride channels at higher micromolar concentrations associated with anesthetic levels.[23] Although both barbiturates and benzodiazepines interact with GABA-A receptors, they are unique because they potentiate GABA-A receptors while increasing chloride ion influx even with very low concentrations of the GABA neurotransmitter.[24]
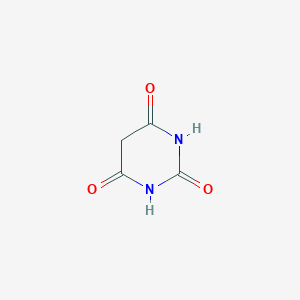
Structure-Activity Relationship
Barbituric acid was the basis of many formulations patented by the Bayer company. Due to its low lipophilicity, barbituric acid had no innate CNS activity. A lipophilic derivative of barbituric acid was developed (barbital: 5,5-diethylbarbituric acid) and successfully induced sleep in dogs.[23]
Amylobarbitone became the first IV anesthetic used in 1928. The formulation of parenteral dosage forms occurred due to the addition of sodium at the C2 position.[25] Lipophilicity was enhanced by Volviler and Tabern with the addition of a sulfur group while replacing an oxygen atom, creating the thiobarbiturates in 1934.[25] In 1957, methohexital was created by Stoelting by adding an aliphatic side chain at carbon 5, along with methylation of the nitrogen atom.[24] The R(+) enantiomer of many barbiturates produces excitatory effects, while the S(−) enantiomers produce more depressant effects.[26]
Classification of Barbiturates
Barbiturates are classified according to the duration of their action. The short- and intermediate-acting ones have effects lasting 2 to 6 hours, while long-acting barbiturates exert their effects for longer than 6 hours.[27][28]
Ultra-short-acting: This category of barbiturates includes methohexital and thiopental.
Short-acting: This category of barbiturates includes pentobarbital and secobarbital.
Intermediate-acting: This category of barbiturates includes amobarbital and butalbital.
Long-acting: This category of barbiturates includes phenobarbital and primidone.
Pharmacokinetics
Absorption: Phenobarbital is rapidly absorbed with a time-to-peak concentration of 2 to 4 hours. The bioavailability of phenobarbital is approximately 90% in adults and less in neonatal populations.[29] Sodium salts of barbiturates are absorbed more rapidly, and food delays the onset of action of orally administered barbiturates. The IV route is usually reserved for managing status epilepticus (phenobarbital sodium) or the induction or maintenance of general anesthesia (eg, methohexital or thiopental). Thiopental observes first-order kinetics in low doses of 5 mg/kg boluses. In high-dose or prolonged infusions, non-linear kinetics will occur due to the progressive saturation of enzyme systems.[30]
Distribution: Highly lipid-soluble barbiturates cross the blood-brain barrier rapidly, but rapid redistribution from the CNS to peripheral tissues occurs.[28] Thiopental and methohexital undergo rapid redistribution after IV injections into less-vascular tissues, particularly muscle and fat, decreasing the concentration of barbiturates in the plasma and brain. Terminating the effect of a single bolus IV injection of thiopental occurs by redistribution from the central compartment to peripheral compartments.[31]
Metabolism: The oxidation of barbiturates is the most important biotransformation that terminates biological activity. In addition, n-glycosylation is important for the metabolism of phenobarbital. Phenobarbital is metabolized extensively by the cytochrome P450, and the maturation of this enzyme family mainly occurs during the neonatal period.[32][33]
Repeated administration of phenobarbital decreases the half-life due to the induction of microsomal enzymes. The self-induced increase in barbiturate metabolism partially accounts for tolerance to barbiturates. In addition, with chronic administration, an increase in aminolevulinic acid (ALA) synthetase enzymes is detected. The effect of barbiturates on ALA synthetase can cause dangerous disease exacerbations in patients with porphyria. Primidone undergoes metabolism to phenylethylmalonamide and phenobarbital. The efficacy of primidone in treating essential tremor is not dependent on its phenobarbital metabolite.[20]
Elimination: About 25% of phenobarbital is excreted unchanged in the urine. The renal excretion can be increased by osmotic diuresis or alkalinization of the urine. The metabolic elimination of barbiturates is more rapid in young people than in older people and infants. Age-related changes have been demonstrated in pharmacokinetics due to slower clearance in older patients, resulting in higher serum concentrations with smaller drug doses.[34] In children, a shorter elimination half-time occurs due to greater clearance.[31] The half-life of phenobarbital decreases by approximately 4.6 hours/day on chronic administration.[35]
Administration
Available Dosage Forms and Strengths
Barbiturates are administered in oral and parenteral forms (intramuscular (IM) and IV). IM injections of solutions of sodium salts such as phenobarbital or amobarbital should be administered in large muscle masses to avoid potential necrosis at superficial sites.
Adult Dosage
Phenobarbital: According to the American Epilepsy Society guidelines, phenobarbital 15 mg/kg in a single dose is suggested for status epilepticus (parenteral benzodiazepines are the first line choice).[36] When administered as an antiepileptic drug for pediatric patients, phenobarbital may be given as an IV loading dose, followed by IV or oral administration.[37]
In neonates, the loading dose of phenobarbital is 20 mg/kg IV, and the maintenance dose is 3 to 4 mg/kg by mouth. Nonresponders should be administered additional doses of 5 to 10 mg/kg till seizure control. The indication for use typically determines the route of administration for adults. Maintenance therapy for antiepileptic drugs in adults generally is the oral route; other first-line drugs have replaced phenobarbital.[38]
Methohexital: Methohexital and thiopental may be administered rectally in pediatrics, particularly if the child cannot cooperate with IV needle administration. This method is best suited in procedures of short duration, such as radiology or dentistry. The usual dose for methohexital is 1 to 1.5 mg/kg for induction. Barbiturates administered for the induction of anesthesia in adults are most commonly given as an IV bolus for a rapid and pleasant loss of consciousness.[39][40]
Thiopental: When using the IV route of administration in pediatrics, wide variation in the required dose is noted. Cote recommended a higher dose range for unpremeditated children.[41] Thiopental was removed from the United States market in 2011 primarily based on the diversion of the drug within the United States as a lethal injection drug.[42]
Pentobarbital: Pentobarbital is administered by IM and IV routes. Pentobarbital is administered by IM route 150 mg to 200 mg as a single-dose pre-anesthetic medication. For status epilepticus, pentobarbital is given as a 5 to 15 mg/kg IV loading dose followed by a continuous infusion of 0.5 to 5 mg/kg/h. Continuous infusion dosing of pentobarbital is titrated electroencephalogram (EEG), following the guidelines set by the Neurocritical Care Society.[18]
Butalbital: Butalbital is used with aspirin-acetaminophen-caffeine for migraine and tension headaches. AAN does not endorse its use for a long duration due to the risk of dependence and medication overuse headaches.[17]
Primidone: The usual starting dose of primidone is 100 to 125 mg at bedtime for seizure control in treatment-naive patients. The regular maintenance beyond 10 days is 250 mg, 3 times a day. The total daily dose of primidone should not exceed 2000 mg. Primidone is also used to treat essential tremors; the suggested starting dose is 25 mg daily, increasing by 25 or 50 mg per month as tolerated.[43]
Amobarbital: The sedative dose of amobarbital is 30 to 50 mg, given 2 or 3 times daily. The hypnotic dose is 65 to 200 mg at bedtime. Amobarbital is a DEA-scheduled II substance, and agents with better safety profiles should be used due to misuse potential.[44]
Specific Patient Populations
Renal impairment: No dose adjustment is provided for methohexital. The use of thiopental is relatively contraindicated in renal disease. Dose reduction is recommended in phenobarbital. Nephrotoxicity is reported with an overdose of phenobarbital.[45]
Hepatic impairment: No dose adjustment is provided for methohexital. As phenobarbital undergoes extensive hepatic metabolism, dose reduction is advised.[46]
Pregnancy considerations: The placental transfer occurs within 1 minute of administration.[24] Neonatal depression may occur if thiopental is used as an induction agent for cesarean section. Methohexital can also cross the placental barrier. For general anesthesia, drugs other than methohexital are recommended by ACOG (American College of Obstetricians and Gynecologists).[47] The use of phenobarbitone is associated with major malformations. Antiepileptic agents, lamotrigine and levetiracetam, are preferred during pregnancy.[48][49]
Breastfeeding considerations: Clinical data on the effects of phenobarbital indicate that inter and intrapatient variability of excretion in breast milk is apparent. Phenobarbital can cause drowsiness in infants, especially when used with other sedating drugs. In a series of breastfeeding infants, for each mg/kg of phenobarbital taken by mothers, the infant's serum concentration increased by 2 to 5 mg/L. Several case reports exist of infant sedation occurring in mothers treated with phenobarbital. Consequently, the infant requires monitoring drowsiness and weight gain, especially in younger, exclusively breastfed infants. If excessive sedation ensues, discontinuation of breastfeeding is suggested.[50]
Concerning the short-acting IV barbiturates, methohexital was found in breastmilk at the highest concentrations 1 to 2 hours after an IV dose and undetectable 24 to 48 hours after an IV dose.[51] For thiopental, when used for induction of anesthesia for cesarean section, the highest concentration of thiopental in breast milk was in the first nursing after anesthesia, about 0.9 mg/L. Breastfeeding can be resumed as soon as the mother has recovered sufficiently from general anesthesia. However, if a combination of drugs is used during the procedure, follow the standard operating procedure considering the elimination half-life of each agent.[52]
Pediatric patients: In the pediatric population, the therapeutic approach for refractory and super-refractory status epilepticus (RSE/SRSE) involves using barbiturates such as phenobarbitone and thiopental for coma induction. These drugs act on GABA receptors, inhibiting N-methyl-D-aspartate (NMDA) receptors. While effective in controlling seizures, unique considerations exist in the pediatric population. Barbiturates, including thiopental, may have a prolonged recovery time and have adverse effects such as hypotension and respiratory depression, which may have specific implications in pediatric patients.
Careful monitoring and individualized dosing are essential, and the decision-making process should consider the potential risks and benefits, considering the patient's age, weight, and overall health status. The treatment approach in pediatric RSE/SRSE involves a tailored, trial-and-error strategy due to the limited evidence and variability in individual responses.[53] Guidelines for severe pediatric TBI emphasize ICP control. In cases of refractory intracranial hypertension persisting after maximal medical and surgical interventions, the use of high-dose barbiturate therapy is recommended for hemodynamically stable patients. However, when implementing high-dose barbiturate therapy to address refractory intracranial hypertension, continuous monitoring of arterial blood pressure and providing cardiovascular support to uphold adequate cerebral perfusion pressure are imperative. This is crucial due to the common occurrence of cardiorespiratory instability in patients undergoing barbiturate coma.[54]
Older patients: As per the American Geriatrics Society (AGS) 2023 Beers Criteria, the use of barbiturates, including butalbital, phenobarbital, and primidone, is discouraged due to a high rate of physical dependence, development of tolerance to sleep benefits, and an increased risk of overdose at low dosages. The use of these medications is avoided in older adults.[55]
Adverse Effects
For women taking phenobarbital as monotherapy, the drug correlates with congenital defects in exposed infants.[5]
When given in IV anesthetics, barbiturates produce a reduction in blood pressure and an increase in heart rate. Respiratory depression and apnea may occur.[24]
Thiopental and thiamylal release histamine, while methohexital and pentobarbital have minimal histamine release.[56]
Extravasation of thiopental (a vesicant) may cause severe tissue necrosis. If extravasation occurs, treatment measures include hyaluronidase and phentolamine.[57] Case reports of successful treatment also include the topical application of a eutectic mixture of local anesthetics and the local injection of lidocaine.[58]
Barbiturates such as butalbital can lead to withdrawal symptoms, including seizures. The recommended risk mitigation strategy is to taper off barbituates under supervision.[15]
Hepatotoxicity
Barbiturates can cause allergic reactions and skin rashes associated with mild liver injury. Phenobarbital is predominantly linked with drug-induced liver injury. Phenobarbital-induced severe adverse drug reactions are DRESS (drug reaction with eosinophilia and systemic symptoms), Stevens-Johnson syndrome, and toxic epidermal necrolysis.[59]
Drug-Drug Interactions
- Phenobarbital is an inducer of the cytochrome enzyme system, specifically the CYP1A2, 2B6, 2C9, and 3A4/5 isozymes that will reduce the efficacy of warfarin, steroids, psychoactive drugs, and immunosuppressants.
- Phenobarbital will also lower the plasma concentrations of other antiepileptic drugs, such as lamotrigine, oxcarbazepine, phenytoin, tiagabine, and valproate.[60]
- Contraceptive failure can occur when systemic hormonal contraception drugs are administered with enzyme inducers like phenobarbital.[61]
- Phenobarbital is a strong CYP3A4 inducer; avoid combination with hepatitis C drugs paritaprevir-ritonavir, ombitasvir, and dasabuvir.[62]
- As primidone is a CYP3A4 inducer, combining it with apremilast is strictly contraindicated.[63]
Contraindications
Box Warnings
Methohexital
Methohexital should be administered exclusively in hospitals or ambulatory care settings equipped to continuously monitor respiratory functions, such as pulse oximetry and cardiac activity. The immediate availability of resuscitative drugs is imperative, as well as age-appropriate equipment for ventilation and intubation. Healthcare professionals proficient in airway management should be consulted.
Phenobarbital
The risks associated with the concomitant use of phenobarbital and opioids include profound sedation, respiratory depression, coma, and death. Concomitant prescribing should be reserved for cases where alternative treatments are insufficient. If combined, dosage and duration should be minimized, and patients should be monitored for sedation and respiratory depression.[66] Prolonged use of phenobarbital may lead to physical dependence, with withdrawal risks increasing with duration and dosage. Although indicated for short-term use, exceeding recommended durations may necessitate a gradual taper to mitigate life-threatening withdrawal reactions. In addition, phenobarbital is not approved for use in adolescents or adults, exposing them to potential risks of abuse, misuse, and addiction, with concomitant use of other substances increasing the likelihood of serious adverse outcomes.
Warnings and Precautions
Absolute contraindications for any barbiturate include status asthmaticus and acute and intermittent variegate porphyria.[24] Hypersensitivity to barbiturates or excipients is a contraindication to their use. Hypersensitivity reactions, including anaphylaxis, have been reported. Barbiturates can trigger hypersensitivity reactions by direct histamine release or immunoglobulin E–mediated mechanisms.[67]
Monitoring
Monitoring for Misuse
In response to the abuse potential of barbiturates, restricted access was initiated with the enactment of the Federal Comprehensive Drug Abuse and Control Act of 1970. Barbiturates are categorized as Schedule II to IV substances, reflecting their varying levels of abuse potential.[68]
Evaluation and Monitoring for Anesthesia
Pre-anesthetic evaluation is required when barbiturates are used for general anesthesia. The Revised Cardiac Risk Index for Pre-Operative Risk (RCRI) is a tool used to estimate the risk of cardiac complications following noncardiac surgery.[69] Guidelines from the American Society of Anesthesiologists (ASA) advocate for monitoring oxygenation, ventilation, circulation, and temperature during anesthesia, as outlined in the Standards for Basic Anesthetic Monitoring. Additionally, the ASA Task Force on postanesthetic care recommends monitoring mental status, patient temperature, pain, nausea and vomiting, and volume status.[70]
Development of Tolerance and Dependence
Tolerance is a gradual loss of effectiveness such that the dose has to be increased to maintain the same effect.[27] This effect is partly explained by enzyme induction in the liver. Animal models have demonstrated tolerance. Withdrawal symptoms may manifest, with nervousness, tremors, agitation, and hypotension potentially developing 2 to 8 days after the abrupt discontinuation of barbiturates. In more severe cases, the patient may experience delirium or grand mal seizures.[27]
Phenobarbital has a narrow therapeutic range of 10 to 30 mg/L, and its fatal dose is 80 mg/L.[71] A Cochrane review found no clear evidence of a benefit to routine serum monitoring drug concentrations for antiepileptic drugs. Dose titration to control seizures was found to be effective.[72] A case report underscores the potential for tolerance, dependence, and misuse associated with butalbital-containing combination analgesics, urging careful consideration in patients presenting with new-onset psychosis. The patient's prolonged daily use of butalbital-containing medication and subsequent admission to a drug rehabilitation facility emphasizes the critical need to recognize and address the potential for misuse early in the clinical setting.[15]
Toxicity
Signs and Symptoms of Overdose
Acute barbiturate toxicity can arise from intentional or unintentional overdose. Barbiturates, with a history of abuse, were associated with 8469 cases of poisoning, according to data from the New York City Health Department, spanning the period from 1957 through 1963.[73] Overdosage of phenobarbital symptoms includes CNS depression, respiratory failure, and hemodynamic instability.
Management of Overdose
No specific antidote exists for barbiturates, and overdose treatment includes supportive care and urinary alkalinization.[71] A systematic review demonstrates the efficacy of multiple-dose activated charcoal for phenobarbital and primidone overdose. Hemodialysis and haemoperfusion may be considered in patients with life-threatening barbiturate toxicity.[74] Extracorporeal clearance with dialysis can augment drug elimination in cases of severe butalbital overdose.[75] During recovery, patients with chronic barbiturate misuse can present with seizures and autonomic instability.[15]
Enhancing Healthcare Team Outcomes
Barbiturates have historically been a widely prescribed class of drugs in outpatient and inpatient settings. Barbiturates are classified as controlled substances, necessitating adherence to all DEA prescription requirements. The prescription drug monitoring program serves to identify potential misuse and abuse.[76] Benzodiazepines have primarily replaced them when used for anti-anxiety or insomnia.
The utilization of barbiturates for IV anesthesia has significantly diminished for the following 2 primary reasons:
- After 2011, leading manufacturers ceased the production of thiopental or methohexital.
- Propofol has emerged as the favored routine IV anesthetic induction agent owing to its ready availability, rapid onset, and quick offset.
Phenobarbital continues to be used as a second-line antiepileptic drug in the United States and has frequent use in low-resource countries as a first-line drug due to its low cost. The systematic review and meta-analysis concluded that phenobarbital is an effective tool in the management of alcohol withdrawal syndrome in an ICU setting.[77] All healthcare professionals, including physicians and nurse practitioners who prescribe these agents, must be fully aware of the adverse drug reactions, misuse, drug-drug interactions, and the potential to develop physical dependence.
When barbiturates are used in anesthesia, supervision by anesthetics and certified registered nurse anesthetists is necessary. Movement disorder specialists should oversee the use of primidone for essential tremors. Given the potential for severe adverse events, including death, a pharmacist should verify the dosing and perform a thorough medication reconciliation to ensure no drug interactions, particularly additive CNS-depressing effects.
The healthcare team must be proficient in resuscitating a patient in the event of an overdose, often necessitating MICU-level care and consultation with a critical care clinician. In cases of severe overdose, consultation with a toxicologist is advisable. A psychiatrist should be consulted once the patient has recovered in case of an overdose. The prescription of barbiturates and subsequent monitoring necessitates an interprofessional team approach, fostering collaboration across various disciplines to achieve optimal patient outcomes in barbiturate therapy.
Media
(Click Image to Enlarge)
References
Sneyd JR. Thiopental to desflurane - an anaesthetic journey. Where are we going next? British journal of anaesthesia. 2017 Dec 1:119(suppl_1):i44-i52. doi: 10.1093/bja/aex328. Epub [PubMed PMID: 29161390]
Brown TC. Thiopentone and its challengers. Paediatric anaesthesia. 2013 Oct:23(10):957-8. doi: 10.1111/pan.12083. Epub 2012 Dec 6 [PubMed PMID: 23216953]
Prabhakar H, Kalaivani M. Propofol versus thiopental sodium for the treatment of refractory status epilepticus. The Cochrane database of systematic reviews. 2017 Feb 3:2(2):CD009202. doi: 10.1002/14651858.CD009202.pub4. Epub 2017 Feb 3 [PubMed PMID: 28155226]
Level 1 (high-level) evidenceRuble JH. The "death" of lethal injection as we know it? The role of chemical execution in the American criminal justice system. Journal of pain & palliative care pharmacotherapy. 2014 Sep:28(3):276-81. doi: 10.3109/15360288.2014.941133. Epub 2014 Aug 14 [PubMed PMID: 25121632]
Brodie MJ, Kwan P. Current position of phenobarbital in epilepsy and its future. Epilepsia. 2012 Dec:53 Suppl 8():40-6. doi: 10.1111/epi.12027. Epub [PubMed PMID: 23205961]
Level 1 (high-level) evidenceKadiyala PK, Kadiyala LD. Anaesthesia for electroconvulsive therapy: An overview with an update on its role in potentiating electroconvulsive therapy. Indian journal of anaesthesia. 2017 May:61(5):373-380. doi: 10.4103/ija.IJA_132_17. Epub [PubMed PMID: 28584345]
Level 3 (low-level) evidenceHaddad SH, Arabi YM. Critical care management of severe traumatic brain injury in adults. Scandinavian journal of trauma, resuscitation and emergency medicine. 2012 Feb 3:20():12. doi: 10.1186/1757-7241-20-12. Epub 2012 Feb 3 [PubMed PMID: 22304785]
Majdan M, Mauritz W, Wilbacher I, Brazinova A, Rusnak M, Leitgeb J. Barbiturates use and its effects in patients with severe traumatic brain injury in five European countries. Journal of neurotrauma. 2013 Jan 1:30(1):23-9. doi: 10.1089/neu.2012.2554. Epub 2012 Dec 6 [PubMed PMID: 22950895]
Jain P, Aneja S, Cunningham J, Arya R, Sharma S. Treatment of benzodiazepine-resistant status epilepticus: Systematic review and network meta-analyses. Seizure. 2022 Nov:102():74-82. doi: 10.1016/j.seizure.2022.09.017. Epub 2022 Sep 26 [PubMed PMID: 36209676]
Level 1 (high-level) evidenceWood J, Ferguson C. Best evidence topic report. Procedural sedation for cardioversion. Emergency medicine journal : EMJ. 2006 Dec:23(12):932-4 [PubMed PMID: 17130605]
Jones NE, Kelleman MS, Simon HK, Stockwell JA, McCracken C, Mallory MD, Kamat PP. Evaluation of methohexital as an alternative to propofol in a high volume outpatient pediatric sedation service. The American journal of emergency medicine. 2017 Aug:35(8):1101-1105. doi: 10.1016/j.ajem.2017.03.008. Epub 2017 Mar 8 [PubMed PMID: 28330689]
Miner JR, Biros M, Krieg S, Johnson C, Heegaard W, Plummer D. Randomized clinical trial of propofol versus methohexital for procedural sedation during fracture and dislocation reduction in the emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2003 Sep:10(9):931-7 [PubMed PMID: 12957974]
Level 1 (high-level) evidenceNaulaers G, Deloof E, Vanhole C, Kola E, Devlieger H. Use of methohexital for elective intubation in neonates. Archives of disease in childhood. Fetal and neonatal edition. 1997 Jul:77(1):F61-4 [PubMed PMID: 9279186]
Bendtsen L, Evers S, Linde M, Mitsikostas DD, Sandrini G, Schoenen J, EFNS. EFNS guideline on the treatment of tension-type headache - report of an EFNS task force. European journal of neurology. 2010 Nov:17(11):1318-25. doi: 10.1111/j.1468-1331.2010.03070.x. Epub [PubMed PMID: 20482606]
Rodulfo A, Augsten A, Wainwright E, Abramovici G. A Case of Severe Fioricet Withdrawal Presenting During Admission to an Inpatient Psychiatric Unit. Case reports in psychiatry. 2021:2021():6371953. doi: 10.1155/2021/6371953. Epub 2021 Nov 8 [PubMed PMID: 34790421]
Level 3 (low-level) evidenceVanderPluym JH, Halker Singh RB, Urtecho M, Morrow AS, Nayfeh T, Torres Roldan VD, Farah MH, Hasan B, Saadi S, Shah S, Abd-Rabu R, Daraz L, Prokop LJ, Murad MH, Wang Z. Acute Treatments for Episodic Migraine in Adults: A Systematic Review and Meta-analysis. JAMA. 2021 Jun 15:325(23):2357-2369. doi: 10.1001/jama.2021.7939. Epub [PubMed PMID: 34128998]
Level 1 (high-level) evidenceMarmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: the american headache society evidence assessment of migraine pharmacotherapies. Headache. 2015 Jan:55(1):3-20. doi: 10.1111/head.12499. Epub [PubMed PMID: 25600718]
Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, Laroche SM, Riviello JJ Jr, Shutter L, Sperling MR, Treiman DM, Vespa PM, Neurocritical Care Society Status Epilepticus Guideline Writing Committee. Guidelines for the evaluation and management of status epilepticus. Neurocritical care. 2012 Aug:17(1):3-23. doi: 10.1007/s12028-012-9695-z. Epub [PubMed PMID: 22528274]
Bernstein JE, Ghanchi H, Kashyap S, Podkovik S, Miulli DE, Wacker MR, Sweiss R. Pentobarbital Coma With Therapeutic Hypothermia for Treatment of Refractory Intracranial Hypertension in Traumatic Brain Injury Patients: A Single Institution Experience. Cureus. 2020 Sep 22:12(9):e10591. doi: 10.7759/cureus.10591. Epub 2020 Sep 22 [PubMed PMID: 33110727]
Shanker V. Essential tremor: diagnosis and management. BMJ (Clinical research ed.). 2019 Aug 5:366():l4485. doi: 10.1136/bmj.l4485. Epub 2019 Aug 5 [PubMed PMID: 31383632]
Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2017 Feb 15:13(2):307-349. doi: 10.5664/jcsm.6470. Epub 2017 Feb 15 [PubMed PMID: 27998379]
Level 1 (high-level) evidenceChau PL. New insights into the molecular mechanisms of general anaesthetics. British journal of pharmacology. 2010 Sep:161(2):288-307. doi: 10.1111/j.1476-5381.2010.00891.x. Epub [PubMed PMID: 20735416]
Level 3 (low-level) evidenceLöscher W, Rogawski MA. How theories evolved concerning the mechanism of action of barbiturates. Epilepsia. 2012 Dec:53 Suppl 8():12-25. doi: 10.1111/epi.12025. Epub [PubMed PMID: 23205959]
Level 3 (low-level) evidenceMartone CH, Nagelhout J, Wolf SM. Methohexital: a practical review for outpatient dental anesthesia. Anesthesia progress. 1991 Nov-Dec:38(6):195-9 [PubMed PMID: 1842156]
Cozanitis DA. One hundred years of barbiturates and their saint. Journal of the Royal Society of Medicine. 2004 Dec:97(12):594-8 [PubMed PMID: 15574863]
Ho IK, Harris RA. Mechanism of action of barbiturates. Annual review of pharmacology and toxicology. 1981:21():83-111 [PubMed PMID: 6263177]
Level 3 (low-level) evidenceDevenyi P, Wilson M. Barbiturate abuse and addiction and their relationship to alcohol and alcoholism. Canadian Medical Association journal. 1971 Feb 6:104(3):215-8 [PubMed PMID: 4924250]
Zhang Q, Yu Y, Lu Y, Yue H. Systematic review and meta-analysis of propofol versus barbiturates for controlling refractory status epilepticus. BMC neurology. 2019 Apr 6:19(1):55. doi: 10.1186/s12883-019-1281-y. Epub 2019 Apr 6 [PubMed PMID: 30954065]
Level 1 (high-level) evidenceJalling B. Plasma concentrations of phenobarbital in the treatment of seizures in newborns. Acta paediatrica Scandinavica. 1975 May:64(3):514-24 [PubMed PMID: 1155069]
Stanski DR, Mihm FG, Rosenthal MH, Kalman SM. Pharmacokinetics of high-dose thiopental used in cerebral resuscitation. Anesthesiology. 1980 Aug:53(2):169-71 [PubMed PMID: 7416528]
Sorbo S, Hudson RJ, Loomis JC. The pharmacokinetics of thiopental in pediatric surgical patients. Anesthesiology. 1984 Dec:61(6):666-70 [PubMed PMID: 6507924]
Stanski DR, Maitre PO. Population pharmacokinetics and pharmacodynamics of thiopental: the effect of age revisited. Anesthesiology. 1990 Mar:72(3):412-22 [PubMed PMID: 2310020]
Burch PG, Stanski DR. The role of metabolism and protein binding in thiopental anesthesia. Anesthesiology. 1983 Feb:58(2):146-52 [PubMed PMID: 6824168]
Homer TD, Stanski DR. The effect of increasing age on thiopental disposition and anesthetic requirement. Anesthesiology. 1985 Jun:62(6):714-24 [PubMed PMID: 4003792]
Pacifici GM. Clinical Pharmacology of Phenobarbital in Neonates: Effects, Metabolism and Pharmacokinetics. Current pediatric reviews. 2016:12(1):48-54 [PubMed PMID: 26496779]
Glauser T, Shinnar S, Gloss D, Alldredge B, Arya R, Bainbridge J, Bare M, Bleck T, Dodson WE, Garrity L, Jagoda A, Lowenstein D, Pellock J, Riviello J, Sloan E, Treiman DM. Evidence-Based Guideline: Treatment of Convulsive Status Epilepticus in Children and Adults: Report of the Guideline Committee of the American Epilepsy Society. Epilepsy currents. 2016 Jan-Feb:16(1):48-61. doi: 10.5698/1535-7597-16.1.48. Epub [PubMed PMID: 26900382]
Level 1 (high-level) evidenceMoffett BS, Weingarten MM, Galati M, Placencia JL, Rodman EA, Riviello JJ, Kayyal SY. Phenobarbital population pharmacokinetics across the pediatric age spectrum. Epilepsia. 2018 Jul:59(7):1327-1333. doi: 10.1111/epi.14447. Epub 2018 Jun 13 [PubMed PMID: 29897629]
Nevitt SJ, Sudell M, Weston J, Tudur Smith C, Marson AG. Antiepileptic drug monotherapy for epilepsy: a network meta-analysis of individual participant data. The Cochrane database of systematic reviews. 2017 Jun 29:6(6):CD011412. doi: 10.1002/14651858.CD011412.pub2. Epub 2017 Jun 29 [PubMed PMID: 28661008]
Level 1 (high-level) evidenceHunter MJ, Griswold JD, Rosenberg M. Administration of methohexital for pediatric outpatient dentistry. Anesthesia progress. 1990 Sep-Oct:37(5):248-51 [PubMed PMID: 2096749]
Carrel R, Binns WH Jr. Rectal pentothal sedation for selected patients. Anesthesia progress. 1975 Sep-Oct:22(5):151-4 [PubMed PMID: 1060389]
Coté CJ, Goudsouzian NG, Liu LM, Dedrick DF, Rosow CE. The dose response of intravenous thiopental for the induction of general anesthesia in unpremedicated children. Anesthesiology. 1981 Dec:55(6):703-5 [PubMed PMID: 7305061]
American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002 Apr:96(4):1004-17 [PubMed PMID: 11964611]
Level 1 (high-level) evidenceLenka A, Louis ED. Primidone Intolerance in Essential tremor: Is it More than Just Age? Tremor and other hyperkinetic movements (New York, N.Y.). 2021:11():57. doi: 10.5334/tohm.672. Epub 2021 Dec 31 [PubMed PMID: 35070493]
Caulkins JP, Goyeneche LA, Guo L, Lenart K, Rath M. Outcomes associated with scheduling or up-scheduling controlled substances. The International journal on drug policy. 2021 May:91():103110. doi: 10.1016/j.drugpo.2021.103110. Epub 2021 Jan 18 [PubMed PMID: 33476862]
Mahmoud SH, Zhou XY, Ahmed SN. Managing the patient with epilepsy and renal impairment. Seizure. 2020 Feb 10:76():143-152. doi: 10.1016/j.seizure.2020.02.006. Epub 2020 Feb 10 [PubMed PMID: 32087549]
Patsalos PN, Spencer EP, Berry DJ. Therapeutic Drug Monitoring of Antiepileptic Drugs in Epilepsy: A 2018 Update. Therapeutic drug monitoring. 2018 Oct:40(5):526-548. doi: 10.1097/FTD.0000000000000546. Epub [PubMed PMID: 29957667]
American College of Obstetricians and Gynecologists' Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 209: Obstetric Analgesia and Anesthesia. Obstetrics and gynecology. 2019 Mar:133(3):e208-e225. doi: 10.1097/AOG.0000000000003132. Epub [PubMed PMID: 30801474]
Gedzelman E, Meador KJ. Antiepileptic drugs in women with epilepsy during pregnancy. Therapeutic advances in drug safety. 2012 Apr:3(2):71-87. doi: 10.1177/2042098611433192. Epub [PubMed PMID: 25083227]
Level 3 (low-level) evidencePatel SI, Pennell PB. Management of epilepsy during pregnancy: an update. Therapeutic advances in neurological disorders. 2016 Mar:9(2):118-29. doi: 10.1177/1756285615623934. Epub 2015 Dec 27 [PubMed PMID: 27006699]
Level 3 (low-level) evidence. Phenobarbital. Drugs and Lactation Database (LactMed®). 2006:(): [PubMed PMID: 30000331]
. Methohexital. Drugs and Lactation Database (LactMed®). 2006:(): [PubMed PMID: 30000358]
. Thiopental. Drugs and Lactation Database (LactMed®). 2006:(): [PubMed PMID: 30000360]
Vasquez A, Farias-Moeller R, Tatum W. Pediatric refractory and super-refractory status epilepticus. Seizure. 2019 May:68():62-71. doi: 10.1016/j.seizure.2018.05.012. Epub 2018 May 19 [PubMed PMID: 29941225]
Kochanek PM, Tasker RC, Carney N, Totten AM, Adelson PD, Selden NR, Davis-O'Reilly C, Hart EL, Bell MJ, Bratton SL, Grant GA, Kissoon N, Reuter-Rice KE, Vavilala MS, Wainwright MS. Guidelines for the Management of Pediatric Severe Traumatic Brain Injury, Third Edition: Update of the Brain Trauma Foundation Guidelines. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2019 Mar:20(3S Suppl 1):S1-S82. doi: 10.1097/PCC.0000000000001735. Epub [PubMed PMID: 30829890]
By the 2023 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society. 2023 Jul:71(7):2052-2081. doi: 10.1111/jgs.18372. Epub 2023 May 4 [PubMed PMID: 37139824]
Hirshman CA, Edelstein RA, Ebertz JM, Hanifin JM. Thiobarbiturate-induced histamine release in human skin mast cells. Anesthesiology. 1985 Oct:63(4):353-6 [PubMed PMID: 2412468]
Le A, Patel S. Extravasation of Noncytotoxic Drugs: A Review of the Literature. The Annals of pharmacotherapy. 2014 Jul:48(7):870-886 [PubMed PMID: 24714850]
Mao CC, Hsieh YC, Hseu SS, Tsai SK, Lee TY. EMLA cream and lidocaine local injection in the treatment of extravenous thiopental injection--a case report. Acta anaesthesiologica Sinica. 1997 Jun:35(2):103-6 [PubMed PMID: 9293651]
Level 3 (low-level) evidence. Barbiturates. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012:(): [PubMed PMID: 31643584]
Brodie MJ, Mintzer S, Pack AM, Gidal BE, Vecht CJ, Schmidt D. Enzyme induction with antiepileptic drugs: cause for concern? Epilepsia. 2013 Jan:54(1):11-27. doi: 10.1111/j.1528-1167.2012.03671.x. Epub 2012 Sep 27 [PubMed PMID: 23016553]
Anderson S, Mauskopf J, Talbird SE, White A, Srinivasan M. Antiseizure medications and oral contraceptives: Impact of enzyme inducers on pregnancy outcomes and costs. Epilepsy & behavior : E&B. 2021 Dec:125():108368. doi: 10.1016/j.yebeh.2021.108368. Epub 2021 Nov 12 [PubMed PMID: 34775242]
Menon RM, Badri PS, Wang T, Polepally AR, Zha J, Khatri A, Wang H, Hu B, Coakley EP, Podsadecki TJ, Awni WM, Dutta S. Drug-drug interaction profile of the all-oral anti-hepatitis C virus regimen of paritaprevir/ritonavir, ombitasvir, and dasabuvir. Journal of hepatology. 2015 Jul:63(1):20-9. doi: 10.1016/j.jhep.2015.01.026. Epub 2015 Jan 31 [PubMed PMID: 25646891]
Level 1 (high-level) evidenceLiu Y, Zhou S, Wan Y, Wu A, Palmisano M. The impact of co-administration of ketoconazole and rifampicin on the pharmacokinetics of apremilast in healthy volunteers. British journal of clinical pharmacology. 2014 Nov:78(5):1050-7. doi: 10.1111/bcp.12448. Epub [PubMed PMID: 24962564]
Savelloni J, Gunter H, Lee KC, Hsu C, Yi C, Edmonds KP, Furnish T, Atayee RS. Risk of respiratory depression with opioids and concomitant gabapentinoids. Journal of pain research. 2017:10():2635-2641. doi: 10.2147/JPR.S144963. Epub 2017 Nov 10 [PubMed PMID: 29180889]
Abrahamsson T, Berge J, Öjehagen A, Håkansson A. Benzodiazepine, z-drug and pregabalin prescriptions and mortality among patients in opioid maintenance treatment-A nation-wide register-based open cohort study. Drug and alcohol dependence. 2017 May 1:174():58-64. doi: 10.1016/j.drugalcdep.2017.01.013. Epub 2017 Feb 28 [PubMed PMID: 28315808]
Miller TR, Swedler DI, Lawrence BA, Ali B, Rockett IRH, Carlson NN, Leonardo J. Incidence and Lethality of Suicidal Overdoses by Drug Class. JAMA network open. 2020 Mar 2:3(3):e200607. doi: 10.1001/jamanetworkopen.2020.0607. Epub 2020 Mar 2 [PubMed PMID: 32202643]
Montañez MI, Mayorga C, Bogas G, Barrionuevo E, Fernandez-Santamaria R, Martin-Serrano A, Laguna JJ, Torres MJ, Fernandez TD, Doña I. Epidemiology, Mechanisms, and Diagnosis of Drug-Induced Anaphylaxis. Frontiers in immunology. 2017:8():614. doi: 10.3389/fimmu.2017.00614. Epub 2017 May 29 [PubMed PMID: 28611774]
Gabay M. The federal controlled substances act: schedules and pharmacy registration. Hospital pharmacy. 2013 Jun:48(6):473-4. doi: 10.1310/hpj4806-473. Epub [PubMed PMID: 24421507]
Roshanov PS, Walsh M, Devereaux PJ, MacNeil SD, Lam NN, Hildebrand AM, Acedillo RR, Mrkobrada M, Chow CK, Lee VW, Thabane L, Garg AX. External validation of the Revised Cardiac Risk Index and update of its renal variable to predict 30-day risk of major cardiac complications after non-cardiac surgery: rationale and plan for analyses of the VISION study. BMJ open. 2017 Jan 9:7(1):e013510. doi: 10.1136/bmjopen-2016-013510. Epub 2017 Jan 9 [PubMed PMID: 28069624]
Level 1 (high-level) evidenceApfelbaum JL, Silverstein JH, Chung FF, Connis RT, Fillmore RB, Hunt SE, Nickinovich DG, Schreiner MS, Silverstein JH, Apfelbaum JL, Barlow JC, Chung FF, Connis RT, Fillmore RB, Hunt SE, Joas TA, Nickinovich DG, Schreiner MS, American Society of Anesthesiologists Task Force on Postanesthetic Care. Practice guidelines for postanesthetic care: an updated report by the American Society of Anesthesiologists Task Force on Postanesthetic Care. Anesthesiology. 2013 Feb:118(2):291-307. doi: 10.1097/ALN.0b013e31827773e9. Epub [PubMed PMID: 23364567]
Level 1 (high-level) evidenceHoyland K, Hoy M, Austin R, Wildman M. Successful use of haemodialysis to treat phenobarbital overdose. BMJ case reports. 2013 Nov 21:2013():. doi: 10.1136/bcr-2013-010011. Epub 2013 Nov 21 [PubMed PMID: 24265338]
Level 3 (low-level) evidenceTomson T, Dahl ML, Kimland E. Therapeutic monitoring of antiepileptic drugs for epilepsy. The Cochrane database of systematic reviews. 2007 Jan 24:2007(1):CD002216 [PubMed PMID: 17253477]
Level 1 (high-level) evidenceBUCOVE A. MISUSE OF VALUABLE THERAPEUTIC AGENTS: BARBITURATES, TRANQUILIZERS, AND AMPHETAMINES. Bulletin of the New York Academy of Medicine. 1964 Dec:40(12):972-9 [PubMed PMID: 14232143]
Roberts DM, Buckley NA. Enhanced elimination in acute barbiturate poisoning - a systematic review. Clinical toxicology (Philadelphia, Pa.). 2011 Jan:49(1):2-12. doi: 10.3109/15563650.2010.550582. Epub [PubMed PMID: 21288146]
Level 1 (high-level) evidencePoyant JO, Albright R, Clain J, Pandompatam G, Barreto EF. Extracorporeal elimination of butalbital in acute aspirin-butalbital-caffeine-codeine (Fiorinal with Codeine) poisoning. Clinical toxicology (Philadelphia, Pa.). 2018 Jun:56(6):439-441. doi: 10.1080/15563650.2017.1400554. Epub 2017 Nov 10 [PubMed PMID: 29124988]
Weaver MF. Prescription Sedative Misuse and Abuse. The Yale journal of biology and medicine. 2015 Sep:88(3):247-56 [PubMed PMID: 26339207]
Umar Z, Haseeb Ul Rasool M, Muhammad S, Yousaf S, Nassar M, Ilyas U, Hosna AU, Parikh A, Bhangal R, Ahmed N, Ariyaratnam J, Trandafirescu T. Phenobarbital and Alcohol Withdrawal Syndrome: A Systematic Review and Meta-Analysis. Cureus. 2023 Jan:15(1):e33695. doi: 10.7759/cureus.33695. Epub 2023 Jan 12 [PubMed PMID: 36788902]
Level 1 (high-level) evidence